Char ac ter is tics of Au to im mune Hep a ti tis in Tai wan: the 11
advertisement

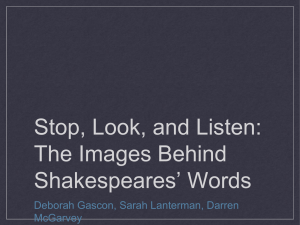
Chi nese Med i cal Jour nal (Taipei) 2002;65:563-569 Original Characteristics of Autoimmune Hepatitis in Taiwan: the 11 Years’ Experiences of a Medical Center Hui-Chun Huang1 Yi-Shin Huang1 Jaw-Ching Wu1 Shyh-Haw Tsay2 Teh-Ia Huo 1 Yuan-Jen Wang1 Jing-Chuan Lo1 Chih-Yen Chen1 Chun-Ping Li1 Full-Young Chang1 Shou-Dong Lee1 1 Di vi sion of Gastroenterology, De part ment of Med i cine, and 2 De part ment of Pa thol ogy, Tai pei Vet erans Gen eral Hos pi tal; and Na tional Yang-Ming Uni ver sity School of Med i cine, Tai pei, Tai wan, R.O.C. Key Words antinuclear an ti body; au to im mune hep a ti tis Background. Un like in West ern coun tries, au to im mune hep a ti tis (AIH) is an in fre quent di ag no sis in Tai wan. The clin i cal char ac ter is tics of AIH in this area are un clear. The aim of this study was to elu ci date the clin i cal features of AIH in Tai wan. Methods. All the med i cal re cords of in-patients with the di ag no sis of chronic hep a ti tis in our hos pi tal from 1990 to 2001 were re viewed for the pos si bil ity of AIH. The clin i cal fea tures, bio chem i cal data, im munological pre sen ta tions, treat ments and sur vival of the pa tients were evaluated. Results. Twenty-two pa tients (15 fe males and 7 males) were di ag nosed as hav ing AIH within 11 years. The me dian age at on set was 64 years (range: 17-77 years). Compared with fe male pa tients, male pa tients had older age (p = 0.001), shorter du ra tion from ini tial pre sen ta tion of symp toms to diag no sis ( p = 0.015), lower se rum lev els of al ka line phosphatase (ALK-P, p = 0.022) and al bu min (p = 0.043). Five (23%) pa tients pre sented with cirrho sis upon di ag no sis. Compared with non-cirrhotic pa tients, cirrhotic patients had lower serum levels of alanine aminotransferase (p = 0.002), aspartate aminotransferase (p = 0.015), gamma-glutamyl transferase (G-GT, p = 0.002), al bu min (p = 0.14), white cell counts (p = 0.009) and platelet counts (p = 0.002). Thirteen (59%) patients had concomitant clinico-pathological fea tures of cholestatic liver dis ease (ALK-P ≥ 2 times of up per nor mal limit or patho logic ev i dence of cholangiopathy). They had higher se rum lev els of ALK-P (p < 0.001) and G-GT (p = 0.004) than 9 non-cholestatic pa tients. There were no sig nif i cant dif fer ences in survival between these groups. The prescribed initial and maintained prednisolone dos ages for our pa tients to con trol dis ease ac tiv ity were 19 ± 15 mg and 8 ± 1 mg, re spec tively, which were lower than those rec ommended in West ern coun tries. The re mis sion rate to ste roid treat ment and re lapse rate af ter dis con tinu ing corticosteroids were 87.5% and 50%, respectively. Conclusions. Compared with West ern AIH pa tients, the AIH pa tients in Tai wan are older and more likely to de velop cholestasis, and need a rel atively lower dose of ste roid for treat ment. Ow ing to one quar ter of the patients already having liver cirrhosis on diagnosis, AIH should be sus pected in any Tai wan ese pa tient with cryptogenic hep a ti tis or cir rho sis. [Chin Med J (Taipei) 2002;65:563-569] Re ceived: March 4, 2002. Ac cepted: August 27, 2002. Cor re spon dence to: Yi-Shin Huang, MD, Di vi sion of Gastroenterology, De part ment of Med i cine, Tai pei Vet erans Gen eral Hos pi tal, 201, Sec. 2, Shih-Pai Road, Tai pei 112, Tai wan. Fax: +886-2-2873-9318; E-mail: yshuang@vghtpe.gov.tw 564 Hui-Chun Huang, et al. A utoimmune hep a ti tis (AIH) is a chronic ac tive hepa ti tis char ac ter ized by un re lent ing hepatocellular necrosis and the presence of special serum autoantibodies. 1,2 This dis or der is not un com mon and has been well in ves ti gated in West ern coun tries.3 Nev erthe less, the role of AIH in the pathogenesis of chronic hep a ti tis is likely to be ne glected in Tai wan that is an en demic area with hep a ti tis B and C vi ral in fec tion. To the best of our knowl edge, only spo radic cases of AIH have been re ported in Tai wan lit er a ture. 4 The clin i cal char ac ter is tics of AIH here are un known. The pur pose of this study was to in ves ti gate the clin i cal char ac ter istics of AIH in Tai wan. Methods Subjects We ret ro spec tively re viewed all the med i cal records of in pa tients with the di ag no sis of chronic hep ati tis (code of In ter na tional Clas si fi ca tion of Dis ease: 571.40) upon dis charge from our hos pi tal from Novem ber 1990 to Au gust 2001. Au to im mune hep a ti tis was di ag nosed based on the cri te ria pro posed by the In ter na tional Au to im mune Hep a ti tis Group. 5,6 It is a scor ing sys tem com posed of gen der, se rum liver biochemistry, serum glob u lin (or im mu no glob u lin G), antinuclear an ti body (ANA), anti-smooth mus cle anti body (ASMA), anti-mitochondrial an ti body (AMA), vi ral hep a ti tis mark ers, drug his tory, al co hol in take, liver histology, other autoimmune disease and re sponse to ther apy. Def i nite AIH is di ag nosed when the aggregate scores are greater than 15 before treatment.5,6 Prob a ble AIH is de fined if the scores are between 10 and 15 be fore treat ment.5,6 For strict di ag nosis, we fur ther ex cluded the prob a ble cases who had (1) neg a tive se rum ANA; (2) pos i tive se rum AMA, hep a ti tis B sur face an ti gen, or hep a ti tis C an ti body; (3) im ag ing ev i dence of biliary tree ab nor mal i ties; (4) pos i tive causal re la tion ship of re cent drug in take and hepatic dys func tion; or (5) ha bit ual al co hol drink ing. The clin i cal char ac ter is tics in clud ing age, gen der, dura tion from the ini tial pre sen ta tion of symp tom to diagnosis, symptoms, signs, associated autoimmune Chi nese Med i cal Jour nal (Taipei) Vol. 65 No. 12 disease, biochemical data, serum ANA, ASMA, AMA and response to treatment were re corded for fur ther eval u a tion. The se rum autoantibodies, in clud ing ANA, ASMA and AMA markers, were measured by an indirect immunofluorescence assay using the Fluoro-KitTM (Incstar Corp. Stillwater, Min ne sota, USA) ac cord ing to the man u fac turer’s in struc tions. Liver bio chem i cal tests were measured by an auto-analyzer (Hitachi Model 736 au to matic an a lyzer; Hitachi, To kyo, Ja pan). Statistics Nu mer i cal data were ex pressed as mean ± SD. The Fisher’s ex act test or Mann-Whitney U test was used to com pare the pa ram e ters be tween groups as appropriate. The Kaplan- Meier model with log rank test was per formed for sur vival anal y sis. A p value less than 0.05 was con sid ered sta tis ti cally sig nif i cant. R esults Twenty-two (1.62%) of the 1,357 pa tients with chronic hep a ti tis were di ag nosed to have AIH, including 11 def i nite and 11 prob a ble cases ac cord ing to the Scoring sys tem.5,6 The ini tial symp toms/signs are sum ma rized in Ta ble 1. Of the 22 AIH pa tients, 15 (68%) were fe males and 7 (32%) were males (Table 2). The me dian age upon the on set of symp toms was 64 years (range: 17-77 years) whereas that upon Table 1. Initial symptoms/signs of 22 Chinese patients with autoimmune hepatitis Symptoms/signs No. (%) Poor appetite Abdominal fullness Fever Jaundice General malaise Nausea Abdominal pain Pruritus Fatigue Weight loss 5 (22.7) 5 (22.7) 4 (18.2) 4 (18.2) 3 (13.6) 2 (9.1) 2 (9.1) 2 (9.1) 2 (9.1) 2 (9.1) De cem ber 2002 Au to im mune Hep a ti tis in Tai wan 565 Table 2. The characteristics of 22 Chinese patients with autoimmune hepatitis before steroid treatment Parameters Age (years, upon onset) Age (years, upon diagnosis) Female/male Duration (weeks) a ANAb ALT (U/L) AST (U/L) ALK-P (U/L) G-GT (U/L) DB (mg/dl) TB (mg/dl) Globulin (g/dl) Albumin (g/dl) IgG (mg/dl) WBC (/cumm) Hemoglobin (g/dl) Platelet (/cumm) Patient values Reference values 54 ± 20 55 ± 20 15/7 76 ± 184 1:798 (1:80-1:2560) 513 ± 416 539 ± 476 218 ± 104 275 ± 267 4.1 ± 4.7 5.6 ± 6.8 4.0 ± 0.9 3.5 ± 0.6 3,021 ± 1,135 5,454 ± 2,270 11.9 ± 2.4 175,368 ± 91,384 Undetectable 0-40 5-45 10-100 8-61 0-0.3 0.2-1.6 0.9-4.7 3.7-5.3 751-1,560 4,800-10,800 14-18 130,000-400,000 Data are expressed as Mean ± SD except otherwise stated. a Duration: the time interval from initial symptoms to definite diagnosis; bgeometric mean (range). ANA = antinuclear antibody; ALT = alanine aminotransferase; AST = aspartate aminotransferase; ALK-P = alkaline phosphatase; G-GT = gamma-glutamyl transferase; DB = direct bilirubin; TB = total bilirubin; IgG = immunoglobulin G; WBC = white blood cell count. Table 3. Comparison of pretreatment data between male and female patients with autoimmune hepatitis Parameters Age (years)a Duration (weeks) b ALT (U/L) AST (U/L) ALK-P (U/L) G-GT (U/L) DB (mg/dl) TB (mg/dl) Globulin (g/dl) Albumin (g/dl) IgG (mg/dl) WBC (/cumm) Hemoglobin (g/dl) Platelet (/cumm) Male (n = 7) Female (n = 15) p 72 ± 5 44 ± 78 603 ± 431 555 ± 404 150 ± 49 147 ± 83 4.7 ± 6.5 7.1 ± 9.3 4.1 ± 1.0 3.1 ± 0.3 3,400 ± 746 5,791 ± 2,011 12.7 ± 2.4 140,286 ± 62,543 47 ± 20 91 ± 217 470 ± 417 532 ± 520 250 ± 108 335 ± 304 3.8 ± 3.6 4.8 ± 5.3 4 ± 0.9 3.7 ± 0.7 2,894 ± 1,239 5,286 ± 2,443 11.6 ± 2.5 195,833 ± 101,448 0.001 0.630 0.418 0.832 0.022 0.217 0.606 0.794 0.691 0.043 0.430 0.881 0.262 0.272 Data are expressed as Mean ± SD. a Age: upon diagnosis. b Duration: the time interval from initial symptoms to definite diagnosis. Abbreviated as Table 1. diagnosis was 65 years (range: 17-77 years). The pretreat ment char ac ter is tics and re sults of lab o ra tory survey of all AIH patients are shown in Table 2. Compared with fe male pa tients, the male pa tients displayed older age, lower se rum al bu min and al ka line phosphatase (ALK-P) lev els upon the time of di ag no- 566 Hui-Chun Huang, et al. Chi nese Med i cal Jour nal (Taipei) Vol. 65 No. 12 Table 4. Comparison of pretreatment data between cirrhotic and non-cirrhotic patients with autoimmune hepatitis Parameters Age (years) a Female/male Duration (weeks)b ALT (U/L) AST (U/L) ALK-P (U/L) G-GT (U/L) DB (mg/dl) TB (mg/dl) Globulin (g/dl) Albumin (g/dl) IgG (mg/dl) WBC (/cumm) Hemoglobin (g/dl) Platelet (/cumm) Cirrhotic (n = 5) Non-cirrhotic (n = 17) p 60 ± 22 3/2 209 ± 360 100 ± 102 154 ± 181 177 ± 127 71 ± 37 0.9 ± 0.6 1.7 ± 0.6 4.2 ± 0.4 2.8 ± 0.4 3,650 ± 1,143 3,004 ± 1,465 10.0 ± 3.5 79,600 ± 24,876 53 ± 20 12/5 37 ± 69 634 ± 394 652 ± 479 230 ± 97 335 ± 277 5.2 ± 5.0 6.8 ± 7.4 4.0 ± 1.0 3.7 ± 0.6 2,875 ± 1,127 6,048 ± 1,985 12.5 ± 1.8 209,571 ± 81,149 0.446 0.762 0.002 0.015 0.256 0.002 0.137 0.247 0.636 0.014 0.545 0.009 0.083 0.002 Data are expressed as Mean ± SD. a Age: upon diagnosis. b Duration: the time interval from initial symptoms to definite diagnosis. Abbreviated as Table 1. Table 5. Comparison of pretreatment data between cholestatic and non-cholestatic patients with autoimmune hepatitis Parameters Age (years) a Female/male Duration (weeks)b ALT (U/L) AST (U/L) ALK-P (U/L) G-GT (U/L) DB (mg/dl) TB (mg/dl) Globulin (g/dl) Albumin (g/dl) IgG (mg/dl) WBC (/cumm) Hemoglobin (g/dl) Platelet (/cumm) Cholestatic (n = 13) Non-cholestatic (n = 9) p 53 ± 20 10/3 44 ± 77 452 ± 378 504 ± 506 269 ± 100 381 ± 300 3.2 ± 3.5 3.4 ± 3.6 3.9 ± 0.9 3.7 ± 0.7 2,954 ± 1,399 5,308 ± 2,455 10.0 ± 3.5 176,500 ± 70,304 57 ± 21 5/4 122 ± 275 600 ± 474 590 ± 454 144 ± 55 123 ± 92 5.3 ± 5.8 8.5 ± 8.9 4.2 ± 1.0 3.2 ± 0.5 3,106 ± 774 5,693 ± 2,069 12.5 ± 1.8 174,111 ± 115,004 0.512 0.896 0.744 0.601 0.004 0.014 0.295 0.095 0.331 0.095 0.918 0.804 0.247 0.720 Data are expressed as Mean ± SD. a Age: upon diagnosis b Duration: the time interval from initial symptoms to definite diagnosis. Abbreviated as Table 1. sis (Ta ble 3). Five pa tients (23%) pre sented with cirrho sis upon di ag no sis. They had sig nif i cantly lower serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), gamma-glutamyl transferase (G-GT), al bu min, white blood cell count and platelet count (Ta ble 4). Thir teen (59%) pa tients De cem ber 2002 who had a more than 2-fold in crease of ALK-P and/or histologic evidence of biliary tree injury were regarded as cholestatic group (Table 5). They had higher se rum lev els of ALK-P and G-GT com pared with non-cholestatic pa tients (Ta ble 5). Four pa tients were as so ci ated with au to im mune diseases, in clud ing 3 with Sjögren’s syn drome and one with sys temic lupus erythematosus. Ste roid ther apy was in sti tuted to 16 pa tients. Two pa tients lost fol low-up af ter ini tial treat ment. The remaining 14 patients responded well (a decline of ALT) in an av er age of 27± 13 days. The ALT level before ste roid ther apy in sti tu tion was 697 ± 386 U/L and re sponded to the ther apy to fall to 71 ± 57 U/L. They ex pressed nor mal ized liver en zyme lev els (87.5%) after an av er age of 57 ± 22 days. The av er age time of main te nance was 49 ± 40 months. The mean ini tial and main tained doses of prednisolone were 19 ± 15 mg and 8 ± 1 mg/day, re spec tively. Among the 14 patients, 1 pa tient dis con tin ued ste roid treat ment due to per sis tent nor mal iza tion of liver bio chem is try tests; 4 pa tients un der went ta per ing of ste roids upon the end of our fol low-up; whereas 7 pa tients (50%) suf fered from ag gra va tion of liver bio chem is try data af ter taper ing ste roids. Ste roid ther apy was not pre scribed to 6 pa tients, be cause 5 of them were cirrhotic pa tients with nearly nor mal liver en zyme lev els and 1 pa tient lost fol low-up af ter clin i cal di ag no sis. Liver bi opsy was per formed in 12 pa tients, and had ev i dence of periportal necroinflammation (in terface hep a ti tis) (Fig. 1) in all. Con com i tant non spe cific biliary tree dam age was found in 9. Of these 9 patients, 6 re sponded to ste roid ther apy well with normal iza tion of liver en zyme lev els. The other 3 pa tients did not re ceive ste roid ther apy be cause of ini tial di agno sis of cir rho sis in 2 and loss of fol low-up in 1. Three pa tients died of liver cir rho sis with esoph ageal variceal bleed ing, hepatic decompensation, and pneu mo nia with sep tic shock, re spec tively and 1 patient lost fol low-up af ter di ag no sis, 2 pa tients lost follow-up af ter ini tial treat ment. There was no sig nif icant dif fer ence in sur vival be tween fe male and male pa tients (72 ± 12 vs. 54 ± 19 months, p = 0.6020), cholestatic and non-cholestatic (75 ± 9 vs. 55 ± 22 months, p = 0.3689), and cirrhotic and non-cirrhotic Au to im mune Hep a ti tis in Tai wan 567 Fig.1. The liver pa thol ogy of an au to im mune hep a ti tis patient re vealed mononuclear cell in fil tra tion at the peri-portal zone, with ne cro sis or de gen er a tion of hepatocytes, which shows a typ i cal char ac ter is tic of interphase hep a ti tis (H&E stain, 40 X). pa tients (81 ± 43 vs. 65 ± 9 months, p = 0.6769). D iscussion AIH is a dis ease of un known eti ol ogy, char ac ter ized by female predominance, hypergammaglobulinemia, circulating antibodies, hepatocytic damage, and marked re sponse to immunosuppressive ther apy. 1,2 Ac cu rate di ag no sis for AIH is in deed im por tant for an ap pro pri ate ther apy. 7 How ever, the spec trum of au toimmune hepatic injury varies markedly from pure hepatocytic to biliary ep i the lial dam age, 1,8,9 which occa sion ally makes the dis tinc tion quite dif fi cult. Since the cur rent study was per formed ret ro spec tively, to avoid cases with con tro ver sies re gard ing in ad e quate study or in def i nite di ag no sis, out-patients and those with AMA positivity were ex cluded. Se lec tion bias may be pres ent un der such a set ting, but the re main ing cases can be eval u ated as an AIH group un doubt edly. Au to im mune hep a ti tis can be clas si fied as type 1 with the pres ence of ANA, ASMA and type 2 with liver-kidney microsomal an ti body (LKM1).10,11 Further more, the re la tion ships of AIH clas si fi ca tion and clinical characteristics to HLA-DR3 and -4 status have been re ported.12 Due to the ret ro spec tive na ture of our study, how ever, LKM1 and HLA tests were not 568 Hui-Chun Huang, et al. per formed upon ini tial pre sen ta tion of the pa tients. In our se ries, fe male to male ra tio was 2.1, which was sig nif i cantly lower than that re ported for the Jap anese (ra tio: 6:1) 13 and for the West erns (ra tio: 8:1).14 It may count that our hos pi tal serves mainly for vet er ans. Al though AIH usu ally af fects young fe males and the meno pause women in West ern ar eas,3,14 our AIH patients seemed older at on set (54 ± 20 years). Sim i larly, two Jap a nese se ries re ported the on set at older age, too (50 and 70 years, re spec tively).13,15 Thir teen of our AIH pa tients had el e vated ALK-P and G-GT lev els and/or cholangiopathy ver i fied by pa thol ogy. How ever, the fol low ing rea sons still support the di ag no sis of AIH in these pa tients: 1) high titer of ANA with out AMA; 2) el e vated se rum lev els of im mu no glob u lin G in stead of M, which is con sis tent with the fea tures of AIH rather than pri mary biliary cir rho sis (PBC); 3) the ab sence of biliary tree dis ease to de velop over a me dian fol low-up of 91 months; 4) except 2 patient lacking follow-up, those who received corticosteroid ther apy sig nif i cantly im proved with nor mal iza tion of liver bio chem is try data. This fur ther sup ported the di ag no sis of AIH;16 and 5) no biliary tree ab nor mal ity iden ti fied by sonography. The cause of a higher per cent age of cholestatic pa tients in our AIH pa tients, how ever, re mains to be clar i fied. Au to im mune cholangitis can be very sim i lar to PBC re gard ing its clin i cal, bio chem i cal, and histopathological fea tures ex cept neg a tive AMA and pos itive ANA. Its clas si fi ca tion in the field of au to im mune liver disease remains uncertain. 17,18 Autoimmune cholangitis may be a vari ant of pri mary biliary cir rhosis.18,19 Though un cer tainty ex ists,20-22 all of our patients, ex cept 5 cirrhotic pa tients, had at least 3-fold el e va tion of alanine transaminase lev els and/or pathological evidence of interphase hepatitis. Con sequently, the di ag no sis of AIH with cholestatic fea tures rather than au to im mune cholangitis was es tab lished. In the West ern ex pe ri ences, the rec om mended initial dose of prednisolone is 60 mg/day, and the main tenance dose is 20 mg/day.2 In con trast, we pre scribed the lower doses for the AIH pa tients (the ini tial and main te nance doses of prednisolone were 19 ± 15 and 8 ± 1 mg, re spec tively). The re mis sion rate in our series was 87.5%, which was com pa ra ble with that of a Chi nese Med i cal Jour nal (Taipei) Vol. 65 No. 12 Sin ga pore se ries (89%) 23 but higher than the West ern re ports (65%).24 The av er age time to re mis sion was also significantly shorter in our group than in the Westerns.24 Whether the Asian AIH pa tients ex ert the higher treat ment re spon sive ness and the lower dose re quire ment to ste roid re main to be clar i fied. Five (23%) pa tients were found to de velop cir rhosis upon di ag no sis. This im pli cates that the pa tient may de lay to con sult med i cal aids or the lo cal phy si cians may over look to di ag nose AIH. The mean sur vival of cirrhotics was not sig nif i cantly dif fer ent from that of non-cirrhotics, which may be re lated to the rel a tively small num ber of cirrhotic pa tients in our se ries. Ac cord ing to the cur rent sur vey, non-cholestatic pa tients pre sented with higher lev els of to tal and di rect bilirubin than cholestatic pa tients, though sta tis ti cal sig nif i cance was not found. The pos si ble ex pla na tion is that the non-cholestatic pa tients are more likely to have hepatocellular dam age, in stead of biliary tract in jury, than cholestatic pa tients. Pro found hepatocellular damage may cause jaun dice. The fol low ing con di tions may sup port this in fer ence. First, com pared with cholestatic cases, non-cholestatic cases tended to have higher lev els of ALT and AST, al though the dif fer ence was not sta tis ti cally sig nif i cant. This may im pli cate the more ac tive pro cess of hepatocellular de struc tion and necro sis in non-cholestatic cases. As cases that re ceived liver pa thol ogy sur vey in this group were lim ited, this point of view can still not be patho log i cally con firmed at pres ent. Sec ond, 4 out of 5 cirrhotic pa tients were non-cholestatic. Among them, 1 pa tient evolved into liver decompensation with re mark ably high lev els of to tal and di rect bil i ru bin. This may cause high mean bil i ru bin level in non-cholestatic group. In sum mary, cholangiopathy and cir rho sis are not un com mon in our Chi nese AIH pa tients, and they tend to be older than West ern pa tients. Since it can be controlled with a lower dose of ste roid here, the di ag no sis of AIH should be kept in mind when ever a Chi nese pa tient with cryptogenic hep a ti tis is un der eval u a tion. References 1. John son PJ, McFarlane IG, Eddleston ALWF. The nat u ral De cem ber 2002 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. course and het er o ge ne ity of au to im mune type chronic ac tive hep a ti tis. Semin Liver Dis 1991;11:187-96. Czaja A. Au to im mune chronic ac tive hep a ti tis. In: Czaja A, Dick son ER, eds. Chronic Ac tive Hep a ti tis: The Mayo Clinic Experience. New York: Dekker, 1986:105-26. Borberg KM, Aadland E, Jahnsen J, Raknerud N, Stiris M, Bell H. In ci dence and prev a lence of pri mary biliary cir rhosis, pri mary sclerosing cholangitis, and au to im mune hep a titis in a Nor we gian pop u la tion. Scand J Gastroenterol 1998; 33:99-103. Hou TI, Wu JC, Huang YS, Lai CR, Tsay SH, Lee SD. Au toim mune hep a ti tis in an area en demic for hep a ti tis B vi rus infec tion: a re port of three cases. Chin Med J (Tai pei) 1996; 57:360-4. Alvarez F, Berg PA, Bianchi FB, Bianchi L, Bur roughs AK, Cancado EL, et al. International Autoimmune Hepatitis Group Re port: re view of cri te ria for di ag no sis of au to immune hep a ti tis. J Hepatol 1999;31:929-38. John son PJ, McFarlane IG. Meet ing re port: In ter na tionalAuto im mune Hep a ti tis Group. Hepatology 1993;18:998-1005. Papo T, Marcellin P, Bernuau J, Durand F, Poynard T, Benhamou JP. Au to im mune chronic hep a ti tis ex ac er bated by al pha-interferon. Ann In tern Med 1992;116:51-3. Chazouillères O, Wendum D, Serfaty L, Montembault S, Rosmorduc O, Poupon R. Primary biliary cirrhosisautoimmune hep a ti tis over lap syn drome: clin i cal fea tures and re sponse to ther apy. Hepatology 1998;28:296-301. Lohse AW, Büschenfelde KHMZ, Franz B, Kanzler S, Gerken G, Dienes HP. Char ac ter iza tion of the over lap syndrome of pri mary biliary cir rho sis (PBC) and au to im mune hep a ti tis: ev i dence for it be ing a hepatitic form of PBC in genetically susceptible in di vid u als. Hepatology 1999;29: 1078-84. Macfarlane IG. The re la tion ship be tween au to im mune markers and dif fer ent clin i cal syn dromes in au to im mune hep a ti tis. Gut 1998;42:599-602. Czaja A, Manns M, Homburger H. Fre quency and sig nif icance of an ti bod ies to liver/kid ney microsome Type 1 in adults with chronic hep a ti tis. Gastroenterology 1992;103: 1290-5. Doherty DG, Donaldson PT, Underhill JA, Farrant JM, Duthie A, Mieli-Vergani G, et al. Allelic se quence vari a tion in the HLA class II genes and pro teins in pa tients with au toim mune hep a ti tis. Hepatology 1994;19:609-15. Au to im mune Hep a ti tis in Tai wan 569 13. Omagari K, Kinoshita H, Kato Y, Nakata K, Kanematsu T, Kusumoto Y, et al. Clin i cal fea tures of 89 pa tients with au toimmune hepatitis in Nagasaki Pre fec ture, Japan. J Gastroenterol 1999;34:221-6. 14. Sherlock S, Dooley J. Chronic hep a ti tis:gen eral fea tures and au to im mune chronic dis ease. In: Sherlock S, Dooley J, eds. Dis eases of the Lliver and Biliary Sys tem. Ox ford: Blackwell, 2002:321-33. 15. Toda G, Zeniya M, Watanabe F, Imawari M, Kiyosawa K, Nishioka M, et al., and the Jap a nese Na tional Study Group of Au to im mune Hep a ti tis. Pres ent sta tus of au to im mune hep atitis in Ja pan-correlating the char ac ter is tics with in ter national cri te ria in an area with a high rate of HCV in fec tion. J Hepatol 1997;26:1207-12. 16. Geubel AP, Baggentoss AH, Summerskill WHJ. Re sponses to treat ment can dif fer en ti ate chronic ac tive liver dis ease with cholangitis fea tures from the pri mary biliary cir rho sis syn drome. Gastroenterology 1976;71:444-9. 17. Colombato LA, Alvarez F, Côté J, Huet PM. Au to im mune cholangiopathy: the re sult of con sec u tive pri mary biliary cirrho sis and au to im mune hep a ti tis? Gastroenterology 1994; 107:1839-43. 18. Michieletti P, Wanless IR, Katz A, Scheuer PJ, Yeaman SJ, Bassendine MF, et al. Antimitochondrial an ti body neg a tive pri mary biliary cir rho sis: a dis tinct syn drome of au to im mune cholangitis. Gut 1994;35:260-5. 19. Goodman ZD, McNally PR, Davis DR, Ishak KG. Autoimmune cholangitis: a vari ant of pri mary biliary cirrho sis. Clinicopathologic and se ro logic cor re la tions in 200 cases. Dig Dis Sci 1995;40:1232-42. 20. Mackay IR, Wood IJ. Lupoid hep a ti tis: a com par i son of 22 cases with other types of chronic liver disease. Q J Med 1962;31:485-507. 21. NcNair ANB, Moloney M, Portmann BC, Williams R, MaFarlane IG. Au to im mune hep a ti tis over lap ping with primary sclerosing cholangitis in five cases. Am J Gastroenterol 1998;93:777-84. 22. Mackay IR. Au to im mune dis ease over laps and the liver: two for the price of one? J Gastroenterol Hepatol 2000;15:3-8. 23. Lee YM, Teo EK, NG TM, Khor C, Fock KM. Au to im mune hep a ti tis in Sin ga pore: a rare syn drome af fect ing mid dleaged women. J Gastroenterol Hepatol 2001;16:1384-9. 24. Czaja AJ. Autoimmune hepatitis: evolving concepts and treat ment strat e gies. Dig Dis Sci 1995;49:435-56.