From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
Peripheral Blood Progenitor Cell (PBPC) Counts During Steady-State
Hematopoiesis Allow to Estimate the Yield of Mobilized PBPC After
Filgrastim (R-metHuG-CSF)-Supported Cytotoxic Chemotherapy
By Stefan Fruehauf, Rainer Haas, Christian Conradt, Simona Murea, Barbara Witt, Robert Mohle,
and Werner Hunstein
Peripheral blood progenitor cells (PBPC) can be mobilized
using cytotoxicchemotherapy and cytokines. There is a substantial variability in the yield of hematopoietic progenitor
cells between patients. We were looking for predictive parameters indicatinga patient's response t o a given mobilization regimen. Multiparameter flow-cytometry analysis and
clonogenic assays were used t o examine the hematopoietic
progenitor cells in bone marrow (BM) and peripheral blood
(PB) before filgrastim (R-metHuG-CSF;Amgen, Thousand
Oaks, CA)aupported chemotherapy and in PB and leukapheresis products (LPs) in the recovery phase. Fifteen patients
(four with high-grade non-Hodgkin's lymphoma [NHLI, t w o
with low-grade NHL, t w o with Hodgkin's disease, t w o with
multiple myeloma, three with breast cancer, one with ovarian cancer, and one with germ cell tumor) were included
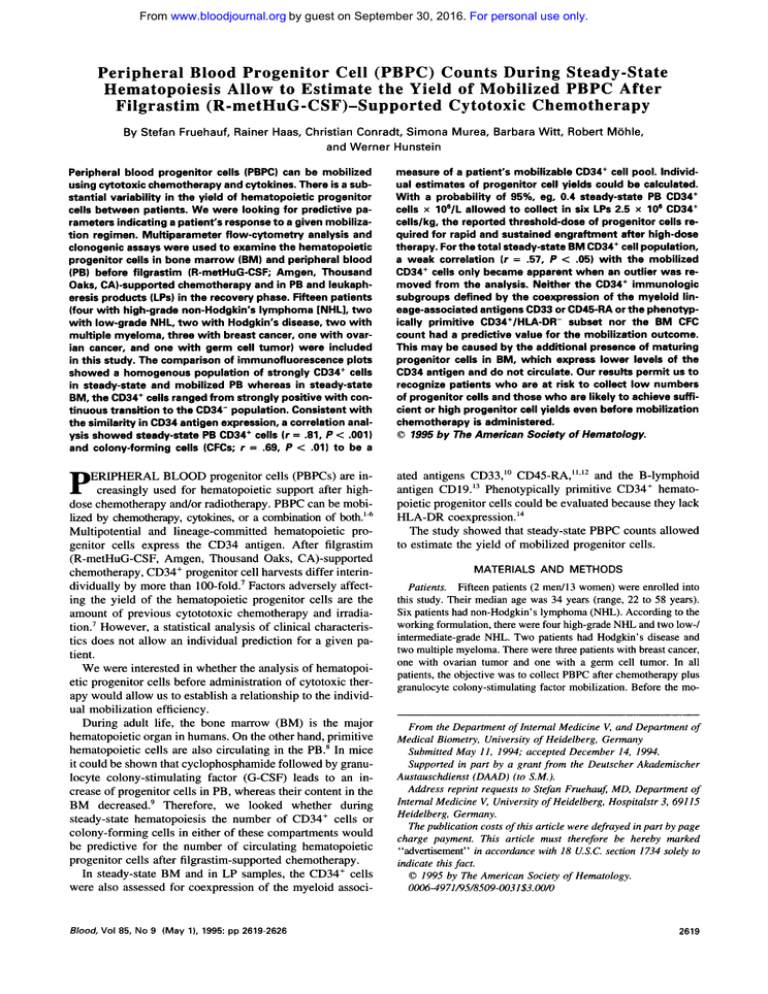
in this study. The comparison of immunofluorescence plots
showed a homogenous population of strongly CD34+ cells
in steady-state and mobilized PB whereas in steady-state
BM, the CD34+cells ranged from strongly positivewith continuous transitionto theCD34- population. Consistent with
the similarityin CD34 antigen expression, acorrelation analysis showed steady-state PB CD34+ cells ( r = 31, P < .OOl)
and colony-forming cells (CFCs; r = .m, P < .01) t o be a
measure of a patient's mobilizable CD34+ cell pool. Individual estimates of progenitor cell yields could be calculated.
With a probability of 95%. eg.0.4 steady-state PBCD34+
cells x 106/L allowed t o collect in six LPs 2.5 x lo6 CD34+
cells/kg, the reported threshold-dose of progenitor cells required for rapid and sustained engraftment after high-dose
therapy. For the total
steady-state BM CD34+cell population,
a weak correlation ( r = .57, P < .05) with the mobilized
CD34+ cells only became apparent when an outlier was removed from the analysis. Neither the CD34+ immunologic
subgroups defined by the coexpression of the myeloid lineage-associatedantigens CD33 or CD45-RA or the phenotypically primitive CD34+/HLA-DR- subset nor the BM CFC
count had a predictive value for the mobilization outcome.
This may be caused by theadditional presence of maturing
progenitor cells in BM, which express lower levels of the
CD34 antigen and do not circulate. Our results permit us t o
recognize patients who are at risk t o collect low numbers
of progenitor cells and those who are likely t o achieve sufficient or high progenitor cell yields even before mobilization
chemotherapy is administered.
0 1995 by The American Society of Hematology.
P
ated antigens CD33," CD45-RA,"*'* and the B-lymphoid
antigen CD19.I3 Phenotypically primitive CD34+ hematopoietic progenitor cells could be evaluated because they lack
HLA-DR coexpression.'4
The study showed that steady-state PBPC counts allowed
to estimate the yield of mobilized progenitor cells.
ERIPHERAL BLOOD progenitor cells (PBPCs) are increasingly used for hematopoietic support after highdose chemotherapy and/or radiotherapy. PBPC can be mobilized by chemotherapy, cytokines, or a Combination of
Multipotential and lineage-committed hematopoietic progenitor cells express the CD34 antigen. After filgrastim
(R-metHuG-CSF, Amgen, Thousand Oaks, CA)-supported
chemotherapy, CD34+ progenitor cell harvests differ interindividually by more than 100-fold.' Factors adversely affecting the yield of the hematopoietic progenitor cells are the
amount of previous cytototoxic chemotherapy and irradiation.' However, a statistical analysis of clinical characteristics does not allow an individual prediction for a given patient.
We were interested in whether the analysis of hematopoietic progenitor cells before administration of cytotoxic therapy would allow us to establish a relationship to the individual mobilization efficiency.
During adult life, the bone marrow (BM) is the major
hematopoietic organ in humans. On the other hand, primitive
hematopoietic cells are also circulating in the PB.' In mice
it could be shown that cyclophosphamide followed by granulocyte colony-stimulating factor (G-CSF) leads to an increase of progenitor cells in PB, whereas their content in the
BM decreased! Therefore, we looked whether during
steady-state hematopoiesis the number of CD34+ cells or
colony-forming cells in either of these compartments would
be predictive for the number of circulating hematopoietic
progenitor cells after filgrastim-supported chemotherapy.
In steady-state BM and in LP samples, the CD34' cells
were also assessed for coexpression of the myeloid associ-
Blood, Vol 85, No 9 (May l), 1995:pp 2619-2626
MATERIALS AND METHODS
Patients. Fifteen patients (2 medl3 women) were enrolled into
this study. Their median age was 34 years (range, 22 to 58 years).
Six patients had non-Hodgkin's lymphoma (NHL). According to the
working formulation, there were four high-grade NHL and two low-/
intermediate-grade NHL. Two patients had Hodgkin's disease and
two multiple myeloma. There were three patients with breast cancer,
one with ovarian tumor and one with a germ cell tumor. In all
patients, the objective was to collect PBPC after chemotherapy plus
granulocyte colony-stimulating factor mobilization. Before the mo-
From the Department of Intern1 Medicine V, and Department of
Medical Biometry, University of Heidelberg, Germany
Submitted May 11, 1994; accepted December 14, 1994.
Supported in part by a grant from the Deutscher Akademischer
Austauschdienst (DAAD) (toS.M.).
Address reprint requests to Stefan Fruehauj MD, Department of
Internal Medicine V, University of Heidelberg, Hospitalstr 3, 69115
Heidelberg, Germany.
The publication costs of this article were defrayed in part by page
charge payment. This article must therefore be hereby marked
"advertisement" in accordance with 18 U.S.C. section 1734 solely to
indicate this fact.
0 1995 by The American Society of Hematology.
0006-4971/95/8509-01$3.00/0
2619
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
FRUEHAUF ET AL
2620
Table 1. Patient Characteristics 1. Prernobilization Features
Bone Marrow Involvement
Patient
No. Sex Age
47
1
2
3
4
5
6
7
8
51
26
33
9
10
11
12
13
14
15
46
26
34
31
37
M
F
F
F
F
F
22
26
58
F
40
32
41
F
F
F
F
F
F
F
M
Diagnosis
Relapses
Cycles
High-grade N H L
7 NHL
High-grade
6
High-grade
NHL
High-grade N H L
Low-grade NHL
Low-grade NHL
Hodgkin‘s disease
3 disease
Hodgkin‘s
Multiple
myeloma
Multiple
myeloma
Breast cancer
Breast cancer
Breast cancer
Ovarian cancer
1 tumor
Germ-cell
1
1
1
14
0
6
0
0
8
1
1
Regimens
4
5
15
5
0
0
0
0
1
3
0
0
1
0
1
At Any Time
At Mobilization
No
No
No
No
No
Yes
No
MIF
CR
Progression
MF
PR
No
PR
No
No
No
No
PR
PR
Yes
Yes
PR
No
No
No
Yes
Yes
Yes
Yes
No
No
No
No
No
No
No
No
No
MF, IY, S
3
0
0
0
0
1
Irradiation
3
3
1
1
2
1
2
2
2
Status at
Mobilization
MF
No
No
No
No
No
No
No
Relapse
Relapse
PR
Adjuvant
Neoadjuvant
Relapse
NoPR
NoRelapse
No
No
Abbreviations: NHL, non-Hodgkin‘slymphoma; CR. complete remission; PR, partial remission; MIF, mediastinal involved field irradiation; MF,
mantle field irradiation; IY, inverted Y field irradiation; S, splenic irradiation.
bilization therapy, BM aspirates from the posterior iliac crest and
PB samples were obtained. The interval from the last chemotherapy
before the mobilization therapy was at least 34 days.
The patients with hematologic malignancies received cytotoxic
chemotherapy such as HAM (high-dose cytosine arabinoside, 2 g/
m’ every 12 hours on days 1 and 2, and mitoxantrone, 10 mg/m2/d
on days 2 and 3; six patients), dexaBEAM (dexamethasone 24 mg/
d on days 1 to 7; carmustine, 60 mg/m’ on day 3; etoposide, 75 mgl
m2on day 4 to 7; cytosine arabinoside, 200 mg/m*on days 4 to 7; and
melphalan, 30 mg/m’ on day 3; two patients) or cyclophosphamide (4
g/m’, one patient; 7 g/m’, one patient). Patients with breast cancer
were treated with ifosfamide, 5 g/mz/d on day 1, and epirubicine,
three patients), whereas the patient with
100 mg/m2 on day 2 (E;
ovarian tumor received ifosfamide, 5 g/m’ on day 1; etoposide, 500
mglm’ on day 2; and cisplatin, 50 mg/m2 on day 2 (PEI-2). The
regimen for the patient with germ cell tumor consisted of cisplatin,
20 mg/m2/d; etoposide, 75 mg/m2/d; and ifosfamide, 1.2 g/m2/d, all
on days 1 to 5 (PEIJ). Subcutaneous administration of filgrastim
was started 24 hours after chemotherapy at a dose of 300 pg/d. In
two patients, the filgrastim-dose was increased to 1,200 pg/d when
during the recovery phase, at a white blood cell (WBC) count of
more than 5,000 X lo6& a distinct CD34+ cell population was not
detectable.
The patient characteristics are given in Tables 1 and 2. The nonhematologic toxicity in the 15 patients during mobilization therapy and
PBPC collection did not exceed grade I1 (World Health Organization
toxicity grading). Patients were treated under the ethical guidelines
of the Joint Committee on Clinical Investigation of the University
of Heidelberg. Informed consent was obtained from each patient.
Immunojfuorescence staining andjow cytometry. For immunofluorescence analysis, I X lo6 mononuclear cells from steady-state
BM, steady-state PB, LP samples, or 20 p L of whole blood obtained
during filgrastim-supported recovery were incubated for 30 minutes
at 4°C with the fluorescein isothiocyanate (FITC)-or phycoerythrin
(PE)-conjugated monoclonal antibodies (MoAbs) HPCA2 (CD34),
HLe-l (CD45), or an irrelevant isotype-matched control antibody
(all from Becton Dickinson, Heidelberg, Germany). The cells were
analyzed with a Becton Dickinson FACScan with a 2 W argon ion
laser as a light source. Excitation was at 488 nm. Fluorescence was
measured at 530 nm for FITC- and at 575 nm for PE-labeled MoAbs.
We used a forward scatter versus CD45 fluorescence dot plot to
discriminate between the smallest lymphohematopoietic cell population and erythrocytes or debris. The percentage of CD34+ cells relative to the percentage of CD45’ cells and the absolute number of
CD34’ cells were calculated as previously described.’
0.05 %
InBM,not more than 0.5% andinPBnotmorethan
nonspecific positive events were allowed in control samples. The
percentage of unspecific events was subtracted from positive events
in stained samples. Examples of steady-state BM, PB, and mobilized
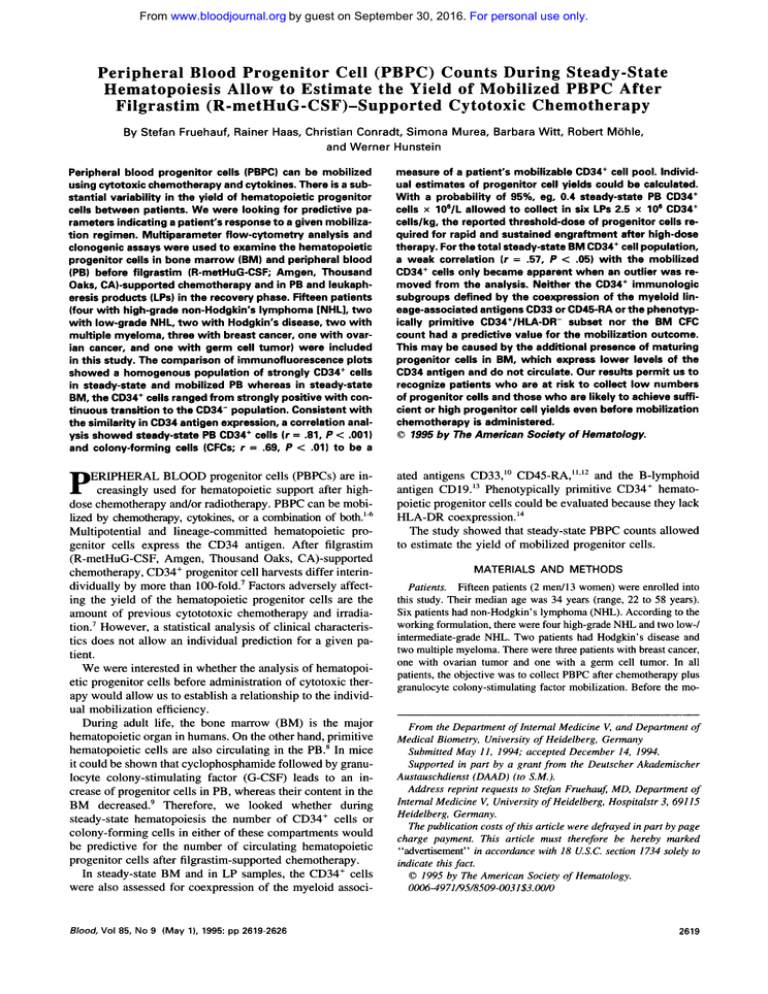
PB of one patient are given in Fig 1.
To increase the sensitivity of progenitor cell detection in steadystate PB, a gated acquisition on CD34’ cells was performed. First,
10,OOO cells were acquired ungated. UsingtheLysis-I1 software
(Becton Dickinson) a gate was set that included the CD34’ cells.
The same sample was run again and 76 2 10 CD34’ cells (mean
2 SEM; values corrected for unspecific events) were acquired into
this gate. The total number of cells in which the CD34’ cells were
Table 2. Patient Characteristics II.Mobilization Features
Patient
No.
1
2
3
4
5
6
7
8
9
10
11
12
13
14
15
Mobilization
Regimen
HAM
HAM
HAM
HAM
HAM
HAM
DexaBEAM
DexaBEAM
CY-4
CY-7
IE
IE
IE
PEI-2
PEL5
Maximum
FilgrastimDose (pgld)
300
300
1,200
300
300
300
1,200
300
300
300
300
300
300
300
300
CD34’ Cellslkg
Harvested
(total)
14.0
3.0
2.7
5.5
3.6
18.4
2.0
0.3
3.2
2.9
7.7
5.5
7.6
5.9
3.7
x lo6
x lo6
x lo6
x 106
x IO6
X
lo6
x 106
x lo6
x lo6
x lo6
x 106
x lo6
X
lo6
x 106
x 106
~
Abbreviation: CY, cyclophospamide (4 d m 2 or 7 dm2).
No. of
LPs
2
4
7
3
3
2
6
2
2
6
2
2
3
5
2
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
2621
ESTIMATE OF PBPC YIELDBEFORE MOBILIZATION
Peripheral Blood
Mobilized
Day 0
Bone Marrow
Day 0
n
0
CD34
0
Side-Scatter C naracteristics
Fig 1. Representative immunofluorescence analysis of CD34 antigen expression in steady-state (day 0 ) BM, PB, and mobilized PBafter
filgrastim-supportedchemotherapy. For assessment of circulating CD34' cells in steady-state hematopoiesis, 123 CD34' cells were acquired
in a life gate from a total population of 171,000 mononuclear cells stained with the HPCA2-PE antibody. From the premobilization, BM and
mobilized PE 10,000 events stained with the HPCA2-FITC antibody were acquired ungated. As opposed to BM, PE contained a homogenous
population of CD34bdoh' cells.
The threefold difference in CD34 fluorescenceintensity between the PE samplesmay be attributed to thedifferent
staining intensity of the PE-conjugated (steady-state PB) and the FITC-conjugated HPCA2-antibody (mobilized PB)."
contained was recorded. From a sample stained withan isotypespecific control antibody the same total number of cells was acquired
using the same gate. The gated CD34 stained and control samples
where then displayed in a forward- versus side-scatter dot plot. A
second gate was drawn to encompass the CD34' cell population,
which displayed a low to intermediate side scatter, thus falling into
the blastnymphocyte region as reported byothers."."'
Unspecific
events of the control sample falling into this region were subtracted
to obtain the corrected CD34' cell number; the CD34' cell frequency was calculated by dividing by the total number of acquired
events. As above, the percentage of CD34' cells relative tothe
percentage ofCD45' cells in the ungated sample was calculated.
The resulting percentage ofCD34' cells was multiplied withthe
mononuclear cell concentration to obtain the steady-state PB CD34'
cell count per liter mononuclear cells. In the analysis presented here,
132.000 -c 18.653 events per gated steady-state PB CD34' cell
sample were measured. The expected coefficients of variation (CV)"
were 13% 5 I%. In an independent series of three steady-state PB
samples stained for CD34' cells, the measured CV of 13% t 6%
was matched by the expected CV of 12% t 3%. This was considered
sufficiently accurate for CD34' cell determinations from steadystate PB.IX
For dual immunofluorescence analysis, I X IO6 cells from BM
or LP samples were incubated for 30 minutes at 4°C with the FITCconjugated MoAb HPCA2 (CD34) and one of the following PEconjugated MoAbs: My-9 (CD33). Leu-l2 (CD19). or HLA-DR.
PE-conjugated HPCA2wasused for double staining with CD45RA.Withthe exception of CD33 (RDI, Coulter Clone, Hialeah.
FL), all antibodies were obtained fromBecton Dickinson. CD34
subset analysis was performed on cells acquired in a fluorescence
versus side-scatter gate. From BM and LP samples, 234 5 33 (mean
5 SEM) and274 5 31 CD34' cells were acquired. respectively.
The proportion of false-positive events in the double-staining was
1.02% t 0.16% of CD34' cells in BM and 0.92% t 0.24%of
CD34' cells in LP samples.
Clonogenic assays for hematopoietic progenitor cells. The concentration of hematopoietic progenitor cells in each BM sample, PB
sample, and LP product was assessed using a semisolid clonogenic
culture assay (Stem Cell Technologies Inc, Vancouver, Canada).
The culture medium consisted of 30% fetal calf serum, 10% medium
conditioned by phytohemagglutinin-stimulated leukocytes, I IU recombinant human erythropoietin, 5 X 10.' M 2-mercaptoethanol,
and 0.9% methylcellulose. BM cells (1.5 X IO'), premobilization
PB mononuclear cells (S X Id),or S X IO4 LP cells were plated
in duplicate and incubated at 37°C and 5% COz in humidified atmosphere. After 14 days, colonies were scored using an inverted microscope.
Collection of PBPC and cpwpresen~ation. Harvesting was performed with a Fenwal CS 3000 (Baxter Deutschland GmbH, Munich.
Germany) using a small volume collection chamber. PB CD34' cell
measurements were started after a WBC count greater than 1 , 0 0 0
X I0'L was reached. The first leukapheresis was started when more
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
FRUEHAUF ET AL
Individual estimations of progenitor cell harvests for a stated PB
CD34' cell count were calculated with the Statistical Analysis System software (SAS Institute Inc, Cary, NC).
1000
n.a.
1.m.
0
**
6
2
RESULTS
LOO
*
"
+
d
02
a
10
0
I
10
100
Bone Marrow Day
IO
1
0
0
1.0
0.1
Colony-Forming Call. x 10 91
Peripheral Blood Day
0
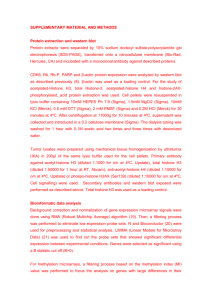
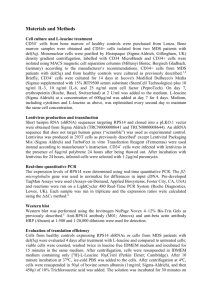
Fig 2. Premobilization BM CD34+ cell and colony counts did not
have a predictive value for the peak CD34' cell count in mobilized
PB (A) (n.s., not significant). However, steady-state PB CD34' cells ( r
= .El, P < .OOl) and colony-forming cells ( r = .69, P < .01) showed
a close relationship to the number of CD34* progenitor cells mobilized (B).
than 10 X 106LCD34' cells were measured in the mobilized PB
or when less than 10 X IO6& CD34+ cells were measured for at least
2 days and a small CD34' cell population could be discriminated by
fluorescence-activated cell sorting (FACS). The first leukapheresis
product was collected after a median of 17 days (range, 10 to 30
days) from the start of chemotherapy.
For each LP, 10 L blood were processed at a flow rate of 50 to
70 mL/min. The apheresis product of 50 mL cell suspension was
mixed with the same volume of minimal essential medium containing 20% dimethylsulfoxide (Merck, Darmstadt, Germany). The
final 100 mL cell suspension was transferred into freezing bags
(Delmed Inc, New Brunswick, NJ) and frozen to -100°Cwith a
computer-controlled cryopreservation device (Cryoson BV-6; Clyoson Deutschland GmbH, Germany). The frozen cells were transferred into the liquid phase of nitrogen and stored at - 196°C.
Statistical analysis. The relationship between different hematologic parameters of the BM, PB, and LP products was estimated by
regression and correlation analysis. To achieve approximately normal (bivariate) distribution, the data were log transformed. Log data
were then used for the analysis. To assess for statistical significance,
the Student's t-test was applied (null hypothesis: no correlation).
Significance levels of P 5 .OS, P 5 .01, or P 5 ,001 were chosen.
CD34 antigen expression on steady-state BM and PB hematopoietic progenitor cells. BM aspirates of patients contained a median of 1.33% CD34+ cells with a range of 0.17%
to 2.93%. This reflects a 17-fold inter-individual difference.
The corresponding median concentration was 3l .49 CD34+
cells X 10%. (0.72 to 169.44 X 10%).In
contrast, the
median proportion of CD34+ cells in PB was approximately
100-fold smaller compared withBM (median, 0.05%;range,
0.03% to 0.12%). Accordingly, 0.46 CD34+ cells X 106/L
(0.14 to 1.86 X 10%) were measured. Neither proportions
nor absolute numbers of BM and PB CD34' cells correlated.
When only patients without BM infiltration or only patients
without prior irradiation were analyzed, this did not improve.
To further analyze the difference between BMandPB
CD34' cells, the level of CD34 expression was compared.
CD34+ cells from BM showed a relatively widerange of
antigen density, with gradual transition from bright to dim
(Fig 1). In contrast, circulating CD34+ cells had a distinctly
high expression of the CD34+ antigen, which distinguished
them clearly from cells not expressing the antigen.
The immunologic data were complemented by the colonyassay results. In BM, the cloning efficiency for CFU-GM
was 568/106 (430/106- 3,333/106) mononuclearcells (MNC)
and for BFU-E 1887/106 cells (897/106 - 3,333/106). In PB
14 CFU-GM colonies/106 MNC(2/106 - 39/10')and142
BFU-Fi/106 plated cells (63/106 - 525/106) were observed.
Different from BM, a strong correlation of CD34' cells and
colonies was observed insteady-state PB ( r = .90, P < ,001).
In comparison, a correlation of CD34' cells and colonies was
also found in leukapheresis products ( r = .76, P < .05, n
= 10). However, here colony data of five patients are not
available, because the high plating efficiency did not allow
to count or discriminate single colonies.
Correlation analysis of steady-state progenitorcell values
and mobilization outcome. As parameter for the mobilization potential, we used the individual peak PB CD34+ cell
counts out of a series of 76 measurements (median, 3 per
patient; range, 1 to 14). The peak values of CD34' cells in
the 15 patients spread from 6.42 to 505.68 CD34'
cells X
10% (median, 43.7 X 10%).MobilizedPBcontained
a
homogenous population of CD34b"gh'cells that was similar
to steady-state PB, but not steady-state BM, which showed
a continuous transition from CD34b"gh' toCD34d'mcells (Fig
1). Whenall steady-state BM CD34+ cell values were plotted
against the corresponding peak CD34+ cell counts, no statistically significant correlation was found ( r = .25, P > .05,
Fig 2A). When the outlier patient no. 8, who had a steadystate BMCD34' cell count of 169.4 X 10%and a peak
CD34' cell count of 6.42 X lo%, was removed from the
analysis a weak correlation ( r = .57, P < .05) became apparent. If steady-state BM colony counts wereused for the
calculation instead of CD34' cell counts, this was not seen
( r = .24, P > .05). Consistent with the similarities in CD34
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
2623
ESTIMATE OF PBPC YIELD BEFORE MOBILIZATION
10
I
p = O.Ool
/
average yield
1
0.1
I
0.1
1.0
CD34+ Cells x 106/1
Peripheral Blood Day 0
Fig 3. Based on the steady-state CD34+ cell count,it was possible
to estimate the number of CD34+ calls in the PBPC harvest even
before mobilization chemotherapy was administered. At the stated
steady-stateP8 CD34+cell count of 0.4x 10'IL. an average yield of 1.4
x 10' CD34' cellslkg body weight can be expected per Ieukapheresis
product, whereas the minimum yield at a 95% level of confidence is
0.43 x 10' CD34+ cells/kg body weight. Steady-state PB CD34* cell
counts are plotted against the mean CD34' cell content per leukapharesis product of every patient.
antigen expression, the steady-state PB CD34+ cell count
correlated strongly ( r = .81, P < .001, Fig 2B) with the
peak PB CD34+ cell value as did the steady-state PB colony
count ( r = .69, P < .01).
It is worth noting that the strong correlation was observed
in a heterogenous group of patients receiving different cytotoxic mobilization regimens. A statistically significant relation between prior cytotoxic therapy or BM involvement and
the degree of progenitor cell mobilization was not found
here. However, an inverse correlation between prior cytotoxic therapy and the mobilization yield could be observed
if a larger, more homogenous patient group was analyzed.'
Steady-state PB CD34+ cell counts allow us to estimate
the progenitor cell yield. For individual estimations, a specific steady-state PB CD34' cell count needs to ensure with
95% probability a certain minimum progenitor cell yield
(Fig 3). This takes into account the scatter around the regression line, ie, the average yield. To estimate these mobilization yields, calculations were based on the average CD34+
cell contents per leukapheresis product that were calculated
from the number of leukaphereses and the total CD34' cells
harvested (Table 2). As expected, a strong correlation ( r =
.77, P = .001) was found between the steady-state PB CD34'
cell counts and the corresponding average CD34' cell contents per leukapheresis product. The lower 95% confidence
line for the individual yield can in turn be used to estimate
the number of leukaphereses required for a certain target
CD34+ cell harvest. As an example, in Table 3 a target
quantity of 2.5 X lo6 CD34' cells/kg body weight, the reported "threshold dose" for rapid and sustained engraftment
after myeloablative therapy7 was chosen. For example, at
0.4 X lo6 steady-state PB CD34+ cells/L, six leukaphereses
will be necessary to collect a sufficient harvest. With this
estimation, we wouldhave been able to reassure four patients
(steady-state PB CD34+ cell counts: patient no. 1, 0.69 X
10%; no. 2, 0.46 X 10%; no. 6, 1.86 X 106/L; no. 9, 0.67
X 10%) in whom we expected low progenitor cell harvests
because of a clinical history of four or more cycles of prior
chemotherapy (Table 1) to have a 95% chance of collecting
sufficient progenitor cells in a clinically acceptable number
of six leukapheresis products before the start of mobilization
therapy.
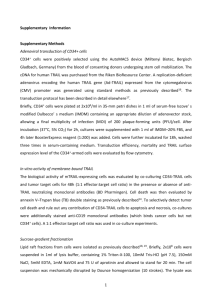
CD34' cell subsets do not improve the predictive value
of steady-state BM. As shown for the wholeBM CD34+
cell population before, neither of the absolute numbers of
myeloid-associated CD34+/CD33+,CD34+/CD45-RA+,early
B-lymphoid CD34+/CD19' nor the phenotypically primitive
CD34+/HLA-DR- cells had a predictive value for the peak
CD34' cell count or the PBPC harvest. This did not change
when the outlier patient no. 8 was removed from the analysis.
A comparison of the proportional distribution of the different
CD34+ subgroups between steady-state BM and LP products
(Fig 4)showed a significantly smaller proportion of CD34+/
CD33' cells in steady-state BM than in LP ( P < .05).For
CD34+/CD19+B-lymphoid progenitors the reverse was seen
( P < .05). The number of CD34+/CD45-RA+cells that represent committed myeloid progenitor cells and B-lymphoid
progenitors'* tended to be higher in BM than inLP. The
proportion of phenotypically immature CD34+/HLA-DRcells within the total CD34+ cell population was not different
between BM and LP.
DISCUSSION
This study was performed to look for predictive parameters of hematopoietic progenitor cell mobilization into the
PB. Progenitor cells can be assessed immunologically by
staining for the CD34 antigen or functionally using colonyassays. CD34' cells comprise hematopoietic progenitor cells
at various developmental stages with different capacity of
self-renewal and differentiation that can be assessed in BM
and PB in steady-state hematop~iesis.~~'~~'~~'~
The immunologic assessment of CD34+ cells was introduced by Siena et
alZ0to monitor progenitor cell harvesting. The relevance of
CD34' cells for PB progenitor cell transplantation has re-
Table 3. Number of Circulating CD34' Cells in Steady-State
Hematopoiesisand Number of PBPC Collections Requiradto
Collect Sufficient CD34' Cells for Rapid and Sustained
ReconstitutionAfter Myeloablative Therapy
~~
Steady-State PB CD34+ Cells x 10B/L
No. of PBPC Collections
0.2
0.4
0.6
0.8
1.o
2.0
As reported by Haas et al: 2.5 x 106/kg body weight.'
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
2624
FRUEHAUFET AL
CD34+/CD33+
;i; 100
V
f 80
m
e
1
D
d
7
100V
80 -
60
60
-
40
40
-
c
c,
a
: 20
2o
0
h
a " 0
I
BM
D
e
m
Q
V
c
4
60
3
40
2
0
+.,
fl
20
1
o
0
h
E
BM
1 /
LP
d
+
d
CD34+/CD45-RA+
LP
!
cently been shown.'-6 As we and other groups have shown,
if after myeloablative therapy, less than 20 X lo4 CFU-GM/
kg" or 2.0 to 2.5 X lo6 PB CD34+ cells/kg7 are autotransplanted, this will result in delayed engraftment.
Where do mobilized CD34+ cells originate? Investigations
in mice using chemotherapy plus G-CSF for mobilization
showed an increase of multipotential and lineage-committed
hematopoietic progenitor cells in the PB and spleen that was
accompanied by a marked loss of these cells in the BM.9 In
another murine study using interleukin-722that showed a
similar effect on progenitor cell mobilization as reported
with G-CSF, the depletion of BM by administration of "Sr,
which led to a greater than 99% reduction in BM myeloid
progenitors abrogated mobilization of multipotential and lineage-committed hematopoietic cells to peripheral sites.
During steady-state hematopoiesis, PB progenitor cells
showed a strong correlation ( r = 3 1 , P < .001) to the
mobilized CD34+ cells and allowed us to estimate the minimum CD34+ cell yieldin a PBPC harvest, whereas for
steady-state BM progenitor cells, a weak correlation to the
mobilized PB CD34+ cells was only found when an outlier
was removed. The predictive quality of premobilization PB
progenitor cell counts has also been noted when after mobilization chemotherapy granulocyte-macrophage CSF was
given instead of G-CSF."
The number of colony-forming cells in steady-state PB
was reported tobe approximately 0.23 X 106/L,xwhich is
consistent with our data. A sensitive and reproducible
method ofCD34'
cell determination facilitates the rapid
quantitation of this small cell population. The biologic relevance of the measured CD34' cell proportions is validated
~
BM
LP
BM
LP
n.8.
Fig
4.
Premobiliration
BM
and LP CD34' cell subsets differ
intheircomposition.BMcontainsasignificantly lower proportion of myeioid-associated
CD34+/CD33+cells and a signifiof
cantly
higher
proportion
CD34'1CD19'
B-lymphoid
progenitor cells ( P < .05 each).
CD34+/CD45-RA+ cells, which
represent
committed
myeloid
B-lymphoid
and progenitor
dk'z
tended to be morefrequent inBM than in LP. The phenotypically
primitive
CD34+/
HLD-DR- population
did
not
show a preferential distribution
BM or
ineithercompartment,
LP.
by the strong correlation with cloning efficiencies also reported by others.I5 Furthermore, the predictive value of
CD34+ cell counts to the mobilized CD34+ cell numbers
was higher than if the estimation was based on colony formation. On the other hand, as described previously24BM CD34'
cells during steady-state hematopoiesis did not show a relation to the colony formation in BM. This may partially be
explained by the variable proportion of nonclonogenic
CD34+/CD19+B-lymphoid progenitors in BM (0.1%to 61%
of CD34' cells; Fig 4) that do not normally ~ i r c u l a t e . ~ ~
Why does the steady-state PB progenitor cell count have a
higher predictive value than BM? We assume that circulating
progenitor cells may be a subgroup of progenitors from those
found inthe marrow. When progenitor cells differentiate,
they gradually loose the CD34' antigen,26which maybe
associated with a loss of the ability to circulate in the PB.
This hypothesis is supported by the finding that circulating
steady-state and mobilized CD34' cells have a highand
distinct expression of the CD34 antigen, whereas BM CD34'
cells display a broad range of antigen density, ranging from
strongly positive with continuous transition to CD34 negativity. This line is followed by a report of Delia et aIz7on the
reciprocal regulation of adhesion molecules and the CD34'
antigen on vascular endothelial cells, suggesting that CD34
may have a negative modulating role on adhesion functions.
A predictive value for steady-state BM CD34' cell subsets
could not be shown. This was expected for the lineagecommitted myelomonocytic CD34+/CD33"" and CD34'1
CD45-RAt'* as well as the B-lymphoid CD34'/CD19'"
precursor populations, which all may contain CD34dimcells.
The CD34+/HLA-DRF subset was considered to be pheno-
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
ESTIMATE OF PBPCYIELD
BEFORE MOBILIZATION
typically primiti~e.'~However, recent reports showed
CD34+/HLA-DR- cells to be heterogenous in proliferative
capacity:8 whereas only the progeny of CD34+/CD38- cells
could give rise to each of the hematopoietic lineages."
Therefore, the lacking correlation between BM CD34+/
HLA-DR- cells and the number of mobilized PB CD34+
cells may not allow conclusions about the role of the most
primitive BM hematopoietic cells in progenitor cell mobilization. Further antigens that need to be studied are CDw90
(Thy-l), which is present on CD34br'ght
but not CD34dimcells
in BM,30 and the CD49d (very late antigen 4 [VLA-4])subpopulation in BM as most circulating CD34' cells are
CD49d-.3'
The data presented show that the minimum progenitor cell
yield can be reliably estimated before chemotherapy plus
G-CSF are started. Patients being at risk of not achieving
sufficient CD34+ cell numbers for a sufficient autotransplant
may thus be recognized. It is also possible to detect patients
who are likely to achieve high progenitor cell yields and
who may thus be eligible for ex vivo techniques that go
along with an expected loss of progenitor cells such as CD34
selection or purging.
ACKNOWLEDGMENT
We thank Professor D.W. van Bekkum (TNO-Institute, Rijswijk,
The Netherlands) for critical reading of the manuscript and helpful
suggestions. We thank Margit Pforsich, Kirsten Flentje, Evi Holdermann, and Magdalena Volk for their excellent technical assistance;
the expertise in their work and high reproducibility of assays were
the basis for establishing the predictive values reported here.
REFERENCES
1. Gianni AM, Siena S , Bregni M, Tarella C, Stem AC, Pileri A,
Bonadonna G: Granulocyte-macrophage colony-stimulating factor to
harvest circulating haematopoietic stem cells for autotransplantation.
Lancet 2:580, 1989
2. Kessinger A, Armitage JO, Smith DM, Landmark JD, Bierman
PJ, Weisenburger DD: High-dose therapy and autologous peripheral
blood stem cell transplantation for patients with lymphoma. Blood
74:1260, 1989
3. To LB, Shepperd KM, Haylock DN, Dyson PG, Charles P,
Thorp DL, Dale BM, Dart GW, Roberts MM, Sage RE, Juttner CA:
Single high doses of cyclophosphamide enable the collection of high
numbers of hematopoietic stem cells from the peripheral blood. Exp
Hematol 18442, 1990
4. Sheridan WP, Begley CC, Juttner CA, Szer J, To LB, Maher
D, McGrath KM, Morstyn G, Fox RM: Effect of peripheral-blood
progenitor cells mobilized with filgrastim (G-CSF) on platelet recovery after high-dose chemotherapy. Lancet 339540, 1992
5. Brugger W, Bross K, Frisch J, Dem P, Weber B, Mertelsmann
R, Kanz L: Mobilization of peripheral blood progenitor cells by
sequential administration of interleukin-3 and granulocyte-macrophage colony-stimulating factor following polychemotherapy with
etoposide, ifosfamide, and cisplatin. Blood 79: 1193, 1992
6. Bensinger W, Singer J, Appelbaum F, Lilleby K, Longin K,
Rowley S , Clarke E, Clift R, Hansen J, Shields T, Storb R, Weaver C,
Weiden P, Buckner CD: Autologous transplantation with peripheral
blood mononuclear cells collected after administration of recombinant granulocyte colony-stimulating factor. Blood 81:3158, 1993
7. Haas R, Mohle R, Fruehauf S , Goldschmidt H, Witt B, Flentje
M, Wannenmacher M, Hunstein W: Patient characteristics associated
2625
with successful mobilizing and autografting of peripheral blood progenitor cells (PBPC) in malignant lymphoma. Blood 83:3787, 1994
8. Udomsakdi C, Lansdorp PM, Hogge DE, Reid DS, Eaves AC,
Eaves CJ: Characterization of primitive hematopoietic cells ir, normal human peripheral blood. Blood 80: 2513, 1992
9. Neben S , Marcus K, Mauch P: Mobilization of hematopoietic
stem and progenitor cell subpopulations from the marrow to the
blood of mice following cyclophosphamide andor granulocyte-colony-stimulating factor. Blood 81: 1960, 1993
10. Andrews RG, Singer J W , Bemstein ID: Precursors of colonyforming cells in humans can be distinguished from colony-forming
cells by expression of the CD33 and CD34 antigens and light scatter
properties. J Exp Med 169:1721, 1989
11. Lansdorp PM, Sutherland HJ, Eaves CJ: Selective expression
of CD45 isoforms on functional subpopulations of CD34+ hematopoietic cells from human bone marrow. J Exp Med 172:363, 1990
12. Fritsch G, Buchinger P, Printz D, Fink FM, Mann G, Peters
C, Wagner T, Adler A, Gadner H: Rapid discrimination of early
CD34+ myeloid progenitors using CD45-RA analysis. Blood
81:2301, 1993
13. Pontvert-Delucq S , Breton-Gorius J, Schmitt C, Baillou C,
Guichard J, Najman A, Lemoine FM: Characterization and functional analysis of adult human bone marrow subsets in relation to
B-lymphoid development. Blood 82:417, 1993
14. Sutherland HJ, Eaves CJ, Eaves AC, Dragowska W, Lansdorp
PM: Characterization and partial purification of human marrow cells
capable of initiating long-term hematopoiesis. Blood 74:1563, 1989
15. Serke S , Sauberlich S , Huhn D: Multiparameter flowcytometrical quantitation of circulating CD34+ cells: Correlation to
the quantitation of circulating haemopoietic progenitor cells by in
vitro colony-assay. Br J Haematol 77:453, 1991
16. Sutherland DR, Keating A, Nayar R, Anania S , Stewart AK:
Sensitive detection and enumeration of CD34+ cells in peripheral
and cord blood by flow cytometry. Exp Hematol 22:1003, 1994
17. Rumke CL: The statistically expected variability in differential leukocyte counting, in Koepke J(ed): Differential Leukocyte
Counting. Skokie, L,College of American Pathologists, 1978, p 39
18. Sauberlich S, Kirsch A, Serke S : Determination of CD34'
hemopoietic cells by multiparameter flow cytometry: Technical remarks, in Wunder E, Sovalat H, HCnon PR, Serke S (eds): Hematopoietic Stem Cells-The Mulhouse Manual. Dayton, OH, AlphaMed,
1994, p 45
19. Bender JG, Unverzagt KL, Walker DE, Lee W, Van Epps D,
Smith DH, Stewart CC, To LB: Identification and comparison of
CD3Cpositive cells and their subpopulations from normal peripheral
blood and bone marrow using multicolor flow cytometry. Blood
77:2591, 1991
20. Siena S , Bregni M, Brando B, Belli N, Ravagnani F, Gandola
L, Stem AC, Lansdorp PM, Bonadonna G, Gianni AM: Flow cytometry for clinical estimation of circulating hematopoietic progenitors
for autologous transplantation in cancer patients. Blood 77:400,1991
21. Schwartzberg L, Birch R, Blanco R, Wittlin F, Muscat0 J,
Tauer K, Hazelton B, West W: Rapid and sustained hematopoietic
reconstitution by peripheral blood stem cell infusion alone following
high-dose chemotherapy. Bone Marrow Transplant 11:369, 1993
22. Grzegorzewski K, Komschlies KL, Mori M, Kaneda K, Usui
N, Faltynek CR, Keller JR, Ruscetti F W , Wiltrout RH: Administration of recombinant human interleukin-7 to mice induces the exportation of myeloid progenitor cells from the bone marrow to peripheral
sites. Blood 83:377, 1994
23. Delain M, Linassier C, Desbois I, Petitdidier C, PoumierGaschard P, Domenech J, Berger E, Lamagnere JP, Colombat P
Predictive factors of adequate blood stem cell collection following
combination chemotherapy and growth factor mobilization. 20th An-
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
2626
nual meeting ofthe European group for bone marrowtransplantation,
Harrogate, UK, March 13-17, 1994
24. Janssen WE, Farmelo MJ, Lee C, Smilee R, Kronish L, Elfenbein GJ: The CD34' cell fraction in bone marrow is not universally
predictive for CFU-GM. Exp Hematol 20:528, 1992
25. Fruehauf S, Haas R, Zeller WJ, Hunstein W: CD34 selection
for purging in multiple myeloma and analysis of CD34' B cell
precursors. Stem Cells 12:95, 1994
26. Terstappen L W " , Huang S, Safford M, Lansdorp PM, Loken MR: Sequential generations of hematopoietic colonies derived
from single nonlineage-committed CD34+CD38- progenitor cells.
Blood 77: 1218, 1991
27. Delia D, Lampugnani MC, Resnati M, Dejana E, Aiello A,
Fontanella E, Soligo D, Pierotti MA, Greaves MF: CD34 expression
is regulated reciprocally with adhesion molecules in vascular endothelial cells in vitro. Blood 81:1001, 1993
28. Muench MO, Cupp J, Polakoff J, Roncarolo MC: Expression of CD33, CD38, and HLA-DR on CD34+ human fetal liver
FRUEHAUF ET AL
progenitors with a high proliferativepotential. Blood 83:3170,
I994
29. Huang S, Terstappen LW: Lymphoid and myeloid differentiation of single human CD34+, HLA-DR+, CD38- hematopoietic stem
cells. Blood 83:1515, 1994
30. Craig W, Kay R, Cutler RL, Lansdorp PM: Expression of
Thy-l on human hematopoietic progenitor cells. J Exp Med
177:1331, 1993
31. Dercksen MW, Gerritsen WR,Dirkson MR, Schaarsbergen
W, Rodenhuis S, van der Wall E, Von dem Borne AEGK, Pinedo
HM, van der Schoot CE: L-Selectin present on CD34' cells is involved in platelet recovery after PBSC transplantation. Presented at
the First Meeting of the European Haematology Association. Br J
Haematol 87:94, 1994 (suppl 1, abstr)
32. Gee A P , Lamb LS: Preparation of samples for flow cytometric
analysis: Recommendations from the ISHAGE course in San JosC, in
Wunder E, Sovalat H, Hhon PR, Serke S (eds): Hematopoietic Stem
Cells-The Mulhouse Manual. Dayton, OH, AlphaMed, 1994, p 67
From www.bloodjournal.org by guest on September 30, 2016. For personal use only.
1995 85: 2619-2626
Peripheral blood progenitor cell (PBPC) counts during steady-state
hematopoiesis allow to estimate the yield of mobilized PBPC after
filgrastim (R-metHuG-CSF)-supported cytotoxic chemotherapy [see
comments]
S Fruehauf, R Haas, C Conradt, S Murea, B Witt, R Mohle and W Hunstein
Updated information and services can be found at:
http://www.bloodjournal.org/content/85/9/2619.full.html
Articles on similar topics can be found in the following Blood collections
Information about reproducing this article in parts or in its entirety may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#repub_requests
Information about ordering reprints may be found online at:
http://www.bloodjournal.org/site/misc/rights.xhtml#reprints
Information about subscriptions and ASH membership may be found online at:
http://www.bloodjournal.org/site/subscriptions/index.xhtml
Blood (print ISSN 0006-4971, online ISSN 1528-0020), is published weekly by the American
Society of Hematology, 2021 L St, NW, Suite 900, Washington DC 20036.
Copyright 2011 by The American Society of Hematology; all rights reserved.