contribution of collagen network and fixed charge to the confined
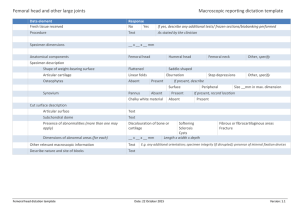
advertisement

CONTRIBUTION OF COLLAGEN NETWORK AND FIXED CHARGE TO THE CONFINED COMPRESSION MODULUS OF ARTICULAR CARTILAGE *Chen, S S (A-NIH); +*Sah, R L (A-NASA, NIH, NSF) +*Department of Bioengineering, UC-San Diego. 9500 Gilman Dr., MC 0412, La Jolla, CA 92093-0412, 858-534-0412, Fax: 858-534-6896, rsah@ucsd.edu INTRODUCTION A variety of studies of articular cartilage indicate that the fixed charge (FC), contributed by anionic glycosaminoglycan (GAG) constituents, contributes primarily to the swelling and compressive properties, while the collagen network (CN) provides cohesive properties (resisting the FC swelling pressure) and strength in tension.7,8 The balance of forces between the FC and CN is believed to be central to the properties of articular cartilage, with increased tissue hydration in osteoarthritis attributed to the weakening of the CN.7,8 Quantitative experimentation and theoretical analysis of isotropic osmotic compression has allowed assessment of the biomechanical properties of the CN.1 Tissue-level biomechanical (confined compression) and biochemical data is now available for articular cartilage. Also, correlative studies have recently implicated both FC and CN as contributors to the confined compression modulus (HA0);11 however, the exact contribution of molecular components to HA0 remains unclear. The present study tested the hypothesis that both FC and CN contribute to the HA0 of articular cartilage. Theoretical and experimental analysis of bovine and human cartilage in confined compression were performed to assess the swelling stress of FC (πFC), the stress on CN (σCN), and the contributions to HA0 of FC and CN (i.e., HA0FC and HA0CN). METHODS Confined Compression Experiments: Stress-strain data from previous experiments on macroscopically normal articular cartilage was analyzed. These included studies on cartilage from (1) fetal, calf, and adult bovines from the femoral condyle and groove (1.0 mm thick),11 (2) femoral condyle cartilage from young (20-40 yo) and aged (60-80 yo) humans (full thickness), and aged (>60 yo) human femoral head cartilage (~1.5 mm thick).3 The HA0 of the 1.0 mm thick articular layers, and the depth-varying HA0 of aged femoral heads in four successive 125 µm layers (layer I-IV) from the articular surface and on additional four 250 µm layers (layer V-VIII)3 was calculated using a finite deformation model.5 Samples were also analyzed biochemically for FC9 or GAG4 (FC [mEq] = 3.98 [mEq/g] * GAG [g]), and also collagen.10 “Balance of Stress” Theory in Confined Compression: The extracellular matrix was assumed to be composed of extrafibrillar (EF) and intrafibrillar (IF) compartments.1 Since the PG are excluded from the IF spaces within the collagen, fixed charge density was calculated based on the EF water, FCDEF. The dependence of πFC on FCDEF and of collagen hydration, HCN (IF water content/g of dry collagen), on πFC were from Basser.1 At equilibrium, the balance of stresses during confined compression is: applied FC CN (1) σ = π +σ At each uncompressed and compressed state (-ε=0–0.3), πFC was calculated from the measured collagen, FC (or GAG), and water contents. Then σCN was calculated from equation (1). HA0FC was calculated by fitting the πFC vs. ε data.4 HA0CN was calculated as HA0-HA0FC. Statistical Analysis: Multivariate ANOVA and the Tukey post hoc test were used. Data are shown as mean±SE. RESULTS The distribution of σapplied between πFC and σCN with increasing compressive strain showed distinct patterns during bovine development (Fig. 1A-C) and different human joints and aging (Fig. 1E-F). In free-swelling cartilage (ε=0), the tensile stress on CN (–σCN) was slightly lower (by ~23%) in the fetus than the calf or adult bovine (p<0.001) but not different with aging and for hip and knee human cartilage (p=0.08). With increasing compression of bovine cartilage, πFC increased; however, the tension on the CN remained nearly unchanged in the fetal tissue, while it decreased in both calf and adult tissue. With compression of human cartilage, πFC increased in all tissues, but the effect on tension on the CN was distinct. In both young and aged femoral condyle, the –σCN decreased but remained tensile; however, in the aged femoral head samples, it became zero at ~10% strain and began to sustain compressive stress. The relative contributions of FC and CN to HA0 varied markedly for the superficial 1.0 mm layer of articular cartilage. HA0, HA0FC, and HA0CN were each significantly lower for fetal cartilage than calf or adult bovine cartilage (Fig. 2A, p<0.05). The contribution of FCEF to HA0, i.e. HA0FC / HA0, decreased from fetal (100%) to adult (58%) (p<0.01). In human cartilage, HA0, HA0FC, 0426 and HA0CN were not different between young and aged femoral condyle samples (p=0.4-0.7), but were lower in aged femoral condyle samples than in the aged femoral head samples (Fig. 2B) (p<0.05). HA0FC / HA0 also varied, being high ( 64% and 74% respectively) in young and aged femoral condyle, and low (44 %) in the aged femoral head. In addition, HA0, HA0FC, and HA0CN increased significantly with depth in aged femoral head samples (p<0.001). However, HA0FC / HA0, remained at ~20% in each layer (Fig. 3). DISCUSSION The present study delineates, for the first time, the contribution of the FC and CN constituents to the confined compression modulus of articular cartilage. Factors that affect the results, determined from experimental studies and a theoretical model, include the dependence of πFC and HCN on FCDEF. However, slight variations in the assumed relationships 1 do not markedly affect the findings described here (data now shown). Other relationships for GAG-induced swelling and osmotic effects on collagen could also be investigated (e.g., in Buschmann2 and Lai6). The molecular basis for the substantial HA0CN remains to be delineated. Since the model does account for the space-filling effect of collagen, modulating the EF volume in which the FC resides, the results imply that the CN directly contributes to the compressive properties of cartilage. It is possible that molecules modifying CN structure, such as crosslinks or collagen-binding small proteoglycans, as well as collagen fibril orientation, may underlie such CN properties. REFERENCES 1 Basser+, Arch Biochem Biophys 351:207, 1998. 2 Buschmann+, J Biomech Engng 117:179, 1995. 3 Chen+, Trans Orthop Res Soc 24:643, 1999. 4 Farndale+, Biochim Biophys Acta 883:173, 1986. 5 Kwan+, J Biomechanics 23:145, 1990. 6 Lai+, J Biomech Engng 113:245, 1991. 7 Maroudas, Nature 260:808, 1976. 8 Maroudas, Sem Arthritis Rheum 11:36, 1981. 9 Maroudas+, Biochim Biophys Acta 215:214, 1970. 10 Stegemann+, Clin Chim Acta 18:267, 1967. 11 Williamson+, Int Cart Repair Soc 3, 2000. Poster Session - Cartilage Mechanics - Hall E 47th Annual Meeting, Orthopaedic Research Society, February 25 - 28, 2001, San Francisco, California