Sample preparation Biopsy Procedure And
advertisement

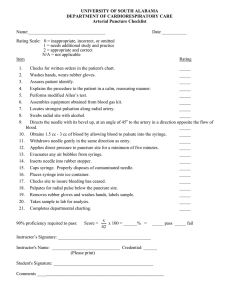
asktheexpert biopsy procedure and sample preparation BY SONIA CARBONE, B.SC, CT(ASC), CMIAC, SENIOR HOSPITAL SCIENTIST, & ANDREW FIELD, FRCPA, FIAC, DIP CYT (RCPA), DEPUTY DIRECTOR & SENIOR STAFF SPECIALIST, DEPARTMENT OF ANATOMICAL PATHOLOGY, ST. VINCENT’S HOSPITAL, NSW. Dear expert, We are performing quite a number of fine needle biopsies in our workplace but there is much debate on the correct procedure and methods of slide preparation. Can you help? At some point during a career in ultrasound every sonographer will come in contact with ultrasound guided biopsies. Fine needle biopsy (FNB) and core biopsy (CB) are the two types of biopsies often performed when sampling a region of interest. It is vital that correct procedures are followed and slide preparation is optimal so that the maximum information can be retrieved from sampled tissues. It is the aim of this article to detail these procedures. Fine needle biopsy FNB is a simple procedure that involves passing a thin needle through the skin to sample fluid or tissue from a cystic or solid mass [1]. The sample of cellular material is then deposited and smeared on glass slides then fixed by air-drying or immediate placement in alcohol. It is then sent to a pathology laboratory for staining with clinical, radiological and other laboratory data. This pre-operative workup may also include core biopsy. However, FNB in some situations can substitute for conventional surgical histopathology, particularly when ancillary studies on FNB include FNB of lung, pancreatic and Equipment thyroid carcinomas, metastatic lesions Figure 1 demonstrates the set-up required prior to beginning the procedure. The equipment required includes: in lymph nodes, high-grade lymphomas with flow cytometry and cytogenetics, carcinoma of the breast, when there is correlation with imaging findings, and • Frosted ended slides. patients with recurrent tumours or who are • Empty slide containers for air-dried slides. inoperable. The diagnostic sensitivity and specificity of FNB depends on several factors including: • The site and type of lesion. • The experience of the operator performing the biopsy. • The quality of the specimen preparation. subsequent analysis under a microscope. • The diagnostic skills of the cytopathologist. a sample and produce on the microscopic slide stained material that is a reliable reflection of the disease process. Today, FNB is regarded as a minimally invasive, cost-effective technique with diagnostic accuracy in the range of 90% to 99% [2]. FNB is usually a component of the pre-operative and pre-treatment study of pathological processes in combination 14 issue 3, 2007 Fine needle biopsy technique material are available. Such situations using Giemsa or Papanicolaou stains and The fundamental requirement is to obtain cases, the cutting action of the needle and the inherent pressure within the tissue of the lesion will produce material in the needle hub without any aspiration. The commonly used term fine needle aspiration biopsy (FNAB) is in some ways a misnomer, because it is the cutting action of the needle, moved many times rapidly into and out of the lesion, that produces material in the needle to be deposited on the slide, rather than ‘aspiration’, which tends to enhance blood contamination of the specimen. In many • Slide containers containing 95% alcohol or modified Carnoy’s fixative. • RPMI transport medium/Hanks salt solution in a container. • Request form. • 23/25 gauge (G) needles. • 10ml syringes. Fig 1. The set up of equipment prior to FNB. soundeffects biopsy procedure and sample preparation Modified Carnoy’s fixative contains 5% acetic acid, which lyses red blood cells, needle, local anaesthetic is not usually required. which can obscure cellular detail in alcohol fixed slides. The slides can remain in this The procedure fixative for up to 48 hours, but for longer All ultrasound gel should be wiped away from the area as this will be aspirated into the needle, deposited onto the slide and will obscure cellular material rendering the sample uninterpretable (figs 2 and 3). The skin should be wiped with an antiseptic, such as an alcohol swab. transport 95% alcohol is preferred. Larger gauge needles, such as 18, 20 or 22, should NOT be used. Using a larger gauge does not increase yield in bloody or hard sclerotic lesions where a 23, 25 or even 26 gauge needle is recommended. Spray fixative is not recommended for alcohol fixation. Fig 4. Cameco syringe pistol, 25G needle and syringe. Adapted from [3]. Preliminary preparation • With a lead pencil, label the frosted end of the slides to be used with the patient's name, date, date of birth and site of biopsy. • Label the container of RPMI transport medium with the same details. • If more than one site is to be biopsied, label slides and containers specimen 1, 2, etc., and with the appropriate site of the biopsy. Fig 2. Microscopic material obscured by ultrasound gel. • Read the request form to see what tests the doctor has requested. These may include microbiology, flow cytometry, cytogenetics or cell block. If these ancillary tests are requested it is best practice to dedicate a separate, additional pass to each test. Fig 5a. Sampling with aspiration. A needle is attached to a syringe. The plunger is retracted by hand to create negative pressure to allow aspiration of material into the hub of the needle. Adapted from [4]. The puncture Good quality fine needle biopsies are obtained when the cellular material obtained is retained within the needle. It is important to avoid aspirating the material into the syringe and, if possible, avoid diluting the aspirate with blood or fluid. If the lesion is cystic, the cyst should be drained using aspiration, and any residual lesion re-biopsied. At the first appearance of any sample in the hub of the needle (at the junction of the syringe and needle) the biopsy is stopped and if aspiration is being utilised, the syringe plunger is released allowing the pressure in the syringe to equalise with the lesion pressure. It is important to preserve the quality of the material obtained by making the smears immediately after completing the puncture. Because of the rapidity of the procedure and thin calibre of the soundeffects Fig 3. Microscopic visible material of a small cell carcinoma. Step 1. Insert the needle through the skin into the centre of the lesion. The operator with experience will feel the difference between the firmness of the tissue and the lesion being sampled; for example, the needle passing through the capsule of a lymph node, into the soft lymphoid tissue, or the firm ‘gripping’ texture of a fibroadenoma. The syringe can be held in a syringe holder or ‘gun’ which allows negative pressure to be obtained within the syringe (fig 4), or the needle can be attached to a syringe, either directly or with plastic tubing, and held by the operator or an assistant. If using a needle attached to the syringe within a syringe holder, ensure the syringe plunger is fully compressed before starting the procedure. Fig 5b. The plunger is retracted with the use of a Cameco syringe pistol. Adapted from [4]. issue 3, 2007 15 biopsy procedure and sample preparation (a) (b) (e) (c) (d) (f) (g) Fig 6. Summary of fine needle biopsy proce� forth in the lesion, directing it at different ar� is then r� Step 2. When the needle is passed into the lesion, it is rapidly agitated forwards and backwards in the one plane. This rapid movement may produce 50 to 100 passages into the lesion in less than 60 seconds. If there is no material in the hub of the needle, the plunger of the syringe is then retracted, creating negative pressure for aspiration (figs 5a & b). If fluid appears in the hub of the needle immediately the needle is placed into the lesion, the cystic component can be drained. Step 3. To sample the lesion more fully, the angle of the needle can be altered, but only when the needle has been withdrawn to the edge of the lesion. It can then be directed into a different region of the lesion. Negative pressure can be applied in the syringe as appropriate by keeping the plunger retracted. This phase is completed when material, fluid or blood appears in the hub of the needle. Step 4. When material appears in the hub of the needle, the pressure in the syringe is allowed to equalise by gently releasing the plunger of the syringe, before the needle is withdrawn from the lesion and skin. Never withdraw the needle from the lesion when any negative pressure remains in 16 issue 3, 2007 dapted from [3]. the syringe, because the sample in the needle will be sucked into the barrel of the syringe, where it cannot be retrieved onto the slides. If material is sucked into the syringe, this can be recovered by rinsing with RPMI medium, and then cell block preparation. A summary of the needle biopsy procedure is shown in figure 6. Slide preparation Fig 7a. Smears should be prepared immediately after the needle has been withdrawn from the skin, to prevent clotting of the specimen, air-drying and to ensure good preservation of the cellular material obtained (figs 7a & b). After the needle has been withdrawn, the syringe is disconnected from the needle, filled with air and reconnected. To avoid needle stick injuries, the hand should commence on the syringe barrel, moving the fingers down to the needle hub, which is gripped and turned to release the needle. The needle is held almost at right angles to the slide and the material in the hub gently expelled (fig 8), care being taken to deposit it as a single drop 10mm from the frosted label edge, approximately at the junction of 2/5th to 3/5th of the slide length. Fig 7b. Figs 7a & b. Compares air-dried (a) to well-preserved microscopic cells (b) of apocrine cells seen in cystic lesions of the breast. soundeffects biopsy procedure and sample preparation Finally, the needle and syringe are rinsed with RPMI transport medium by partially filling the syringe with RPMI and expelling the solution gently back into its container (fig 11). Fig 8. The needle is held close to a right angle to the slide and material is deposited in a single drop. Gently lower another slide onto the bottom slide where the specimen has been deposited, then quickly but gently pull top and bottom slides apart as the drop spreads from the weight of the top slide (fig 9). Fig 9. Shows top slide being placed on the bottom slide. The material is gently spread from the weight of the top slide. Smears can then be: • Immediately immersed in alcohol fixative. The split second the smeared slides are separated, the bottom slide should be deposited in the alcohol fixative (fig 10) or; • Allowed to dry using a gentle warm air stream from a simple hair-dryer. Fig 12a. Shows a section from a cell block from a FNB lymph node stained with haematoxylin and eosin. Fig 11. Shows the needle and syringe being rinsed in RPMI medium. Further needling (a second or third pass) may now be performed using a new needle and the slide preparation procedure repeated. All specimen containers should have the lids screwed on correctly and the slides/specimen containers should be unambiguously labelled with the patient’s name, date, site of biopsy and the number of passes. Complete a request form including patient’s name, address, date of birth, exact site of biopsy, tests requested, referring doctor plus any relevant clinical information. The specimen should be sent immediately to the cytology laboratory for processing. Additional material collected at FNB Any additional material collected can be prepared in the following ways. Needle rinse Cellular material rinsed out of the syringe in the RPMI solution can be centrifuged, and used to make either cytospin slides or a cellblock, depending on the size of the pellet after centrifugation. Cytospin slides are stained using various stains to aid diagnosis, while a cell block is fixed in formalin, embedded in paraffin, cut into sections and stained with haematoxylin and eosin or with immunostaining (fig 12a). Fig 10. Shows one slide being placed immediately in alcohol fixative, while the other is allowed to air-dry. soundeffects Immunostaining is an extremely important ancillary tool for the definitive diagnosis of lesions. For example, carcinomas can be stained to elucidate the exact site of origin Fig 12b. Shows a section from the same cell block showing positive staining CAM 5.2 – keratin for metastatic carcinoma. of metastases in lymph nodes (fig 12b). Microbiology If clinically it is suspected that the lesion could be due to an infection a sample should be taken for microbiological analysis: • If purulent fluid is present, then place any excess fluid in a sterile yellow top container. • If there is little fluid obtained then place 10ml of sterile saline in a sterile yellow top container and then rinse the needle and syringe in this fluid in the same way as you would for a needle rinse. Flow cytometry If clinically you suspect a lymphoma, as in a FNB of a lymph node or para-aortic mass, then a sample for flow cytometry should be collected. This sample is best collected in RPMI medium in the same way as detailed above where the cellular material in the needle and syringe is rinsed in the solution and placed in a correctly labelled specimen container. Cytogenetics can also be performed on the sample. issue 3, 2007 17 biopsy procedure and sample preparation Note: RPMI medium or Hanks salt solution should be kept in the refrigerator and will turn a yellow colour when it has expired. Points to remember 1. Release the negative pressure in the syringe before withdrawing the needle from a lesion. Otherwise the collected cells will be pulled into the syringe causing air-drying artifacts and making it impossible to retrieve the material from the syringe for cytology. 2. Disconnect the needle from the syringe to retract the plunger, filling the syringe with air, reconnecting the needle and expelling the material onto the slides. Material will be lost in the syringe if this is not done, causing the same problem as in (1). 3. Do not allow the material to clot in the needle once it is withdrawn from the patient. Immediately expel the material onto the slides. The operator should not keep the needle in the patient for more than 60 seconds because the material will clot in the needle and, with each pass, this time limit should be even shorter. 4. Do not allow the material to air-dry prior to, during, or after making smears, unless purposely preparing air-dried slides. There should be minimal time delay between completion of the biopsy and preparation of the slides. Smears for alcohol fixation and Papanicolaou stained slides should be immediately placed in alcohol fixative. All air-dried slides should be completely dry before they are placed in a container and transported to the laboratory. 5. Slides and RPMI medium are not sterile; hence a new needle should be used for each pass, and each different site biopsied. 6. If cyst fluid is obtained in the syringe, the needle need not be disconnected to retract the plunger prior to making the smears. Smears may be made directly with a few drops of the fluid expelled gently onto the slide to form a droplet approximately 8mm in diameter. The remaining fluid should be sent to the laboratory in a labelled container for cytospin slide preparation and routine processing. 7. Do not rinse or lubricate the needle and syringe with any substance prior to biopsy. This may cause destruction of part or all the cellular material by osmotic cytolysis. 8. Send the specimen with a signed request form detailing the relevant patient information and clinical history. It is important to remember that the effectiveness of FNB is largely operator dependent and it is important to have all equipment ready to minimise any potential problems with specimen preparation. Because an FNB can only sample a region of a mass or lump, there is a risk that any abnormal cells may be missed and not detected through sampling error. Making three or four separate passes into a lesion can reduce this error. [2]. It is sometimes used instead of FNB, or visa versa, but the tests are complementary. FNB is less expensive and offers immediate staining and assessment. This creates the opportunity for triaging, extra FNB passes or core biopsy. FNB is generally less traumatic to the patient with less bruising. Core biopsy is a more invasive procedure than an FNB, as it involves making a small incision in the skin after local anaesthetic and a wider bore cutting needle. The samples of tissue taken during a core biopsy are collected into a specimen container filled with 10% buffered formalin and sent to the histology laboratory for processing. This processing generally takes 24 to 48 hours. Conclusion These guidelines have been developed from experience at St. Vincent’s Hospital and we hope you find them useful. It is vital to consult your current pathology service and it is important that you follow the guidelines of your provider. References 1. Virtual Medical Centre [homepage on the internet]. Summary of Fine Needle Aspiration Biopsy (FNA). [updated 2007 Feb 20; cited 2007 Jul 1]. Available from: http://www. virtualcancercentre.com/investigations. asp?sid=3. 2. University of Iowa Hospitals and Clinics. Fine Needle Aspiration Biopsy. [serial on the internet]. 2002 [cited 2007 Jul 1];3(2):[about 4 p.]. Available from: http://www.uihealthcare. com/news/currents/vol3issue2/ 05fineneedleaspiration.html. 3. Orell SR, Sterrett GF, Walters MN, Whittaker D. Manual and Atlas of Fine Needle Aspiration Cytology. 2nd ed. Edinburgh: Churchill Livingstone; Core biopsy Core biopsy is another method of tissue diagnosis; that is, a way of sampling the cells in a suspicious lump or mass 18 issue 3, 2007 1992. 4. Trott PA. Breast Cytopathology. A Diagnostic Atlas. London: Chapman & Hall Medical; 1996. soundeffects