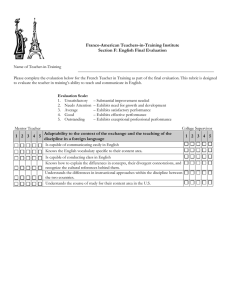
advertisement

Ovarian borderline tumors of MRI: Imaging findings and radiologic-pathologic correlation Poster No.: C-317 Congress: ECR 2009 Type: Educational Exhibit Topic: Genitourinary Authors: R. N. Matsubayashi , Y. Matsuo , T. Nakazono , Y. Okajima , T. 1 1 1 2 2 3 2 3 Muranaka ; Fukuoka/JP, Tokyo/JP, Saga/JP Keywords: Ovary, Imaging findings, borderline tumor DOI: 10.1594/ecr2009/C-317 Any information contained in this pdf file is automatically generated from digital material submitted to EPOS by third parties in the form of scientific presentations. References to any names, marks, products, or services of third parties or hypertext links to thirdparty sites or information are provided solely as a convenience to you and do not in any way constitute or imply ECR's endorsement, sponsorship or recommendation of the third party, information, product or service. ECR is not responsible for the content of these pages and does not make any representations regarding the content or accuracy of material in this file. As per copyright regulations, any unauthorised use of the material or parts thereof as well as commercial reproduction or multiple distribution by any traditional or electronically based reproduction/publication method ist strictly prohibited. You agree to defend, indemnify, and hold ECR harmless from and against any and all claims, damages, costs, and expenses, including attorneys' fees, arising from or related to your use of these pages. Please note: Links to movies, ppt slideshows and any other multimedia files are not available in the pdf version of presentations. www.myESR.org Page 1 of 48 Learning objectives Learning Objectives n To illustrate the MR imaging features of ovarian borderline tumors. n To learn the essential diagnostic clues based on the histologic features of borderline tumors. Background Background n Ovarian tumors are classified as benign, borderline, and malignant. n Borderline tumors have a relatively good prognosis and originate in younger patients compared with malignant tumors, and it is important to diagnose them correctly to ensure adequate treatment. n We present the MR images of surface epithelial-stromal borderline tumors and correlate the findings with histologic features. Additionally, granulosa cell and carcinoid tumors are also shown. Imaging findings OR Procedure details Imaging findings Surface Epithelial Borderline Tumors 1. Serous Borderline Tumor (SBT) n Definition: An ovarian tumor of low malignant potential exhibiting an atypical epithelial proliferation of serous type cells greater than that seen in their benign counterparts but without destructive stromal invasion. n Epidemiology: Patients with SBT are approximately 10-15 years younger than those with serous carcinoma. About 30-50% of SBT are bilateral. n Macroscopy: May be cystic with a variable number of excrescences, form a solid purely surface papillary growth or have a combination of these appearances. SBTs Page 2 of 48 generally lack areas of necrosis and hemorrhage. The cysts usually contain serous fluid, but can occasionally be mucinous. Serous surface borderline tumor is the variant; polypoid excrescences formed by fine papillae with features of SBT occupy the outer surface of the ovary. n Histopathology: The hallmarks of SBT that distinguish it from a cystadenoma are the presence of epithelial hyperplasia forming papillae, micropapillae associated with "detached" or "floating" cell clusters and mild to moderate nuclear atypia. The epithelial hyperplasia exhibits "hierarchical branching". There is no destructive stromal invasion. n The micropapillary type (5-10%) more frequently involves the ovarian surface. Fig.: Serous borderline cystic tumor exhibiting polypoid excrescences in the cyst. Page 3 of 48 Fig.: On T2-weighted images (T2WI), the excrescence exhibited a "broccoli"-like appearance, and had low signal-intensity (SI) stalk with delicate branching. This reflects the histologic hierarchical branching. Page 4 of 48 Fig.: Histologically, the stroma exhibits dense collagen and hyalinization (a), and severe edematous change in the surface (b). Macroscopically, this edematous region appears as many cyst-like nodules (arrows). Page 5 of 48 Fig.: A serous tumor can be confined to the right ovarian surface (arrows), and typical cystic mass with excrescences in the contralateral ovary. Serous tumors are often bilateral with different growth pattern and grade. Imaging Findings of SBT: n Serous borderline cystic tumor exhibiting polypoid excrescences in the cyst. n On T2-weighted images (T2WI), the excrescence shows a "broccoli"-like appearance, and has low signal-intensity (SI) stalk with delicate branching. This reflects the histologic "hierarchical branching". 2. Mucinous borderline tumor (MBT), intestinal-type n Definition: Ovarian tumors of low malignant potential exhibiting an epithelial proliferation of mucinous type cells greater than that seen in their benign counterparts but without evidence of stromal invasion. The epithelial component resembles intestinal epithelium and almost always contains goblet cells. n Epidemiology: The intestinal-type account for 85-90% of mucinous borderline tumors. Page 6 of 48 n Macroscopy: The tumors are bilateral in approximately 5% of cases and usually large, multilocular and rarely unilocular cystic masses containing watery or viscous mucoid material. Velvety excrescences may line the cysts. Hemorrhage, necrosis, solid and papillary areas are occasionally seen. n Histopathology: Areas resembling mucinous cystadenomas are common. In the borderline areas, the cells lining the cysts are stratified (usually to no more than 3 layers). n Borderline tumors tend to have a larger number of loculi than adenomas (Okamoto, et al. 2007). Fig.: A large, multilocular cystic mass exhibits a typical, "stained-glass" appearance. In particular, the central part exhibits many tiny loculi with thickening of the walls. This part shows a high SI on DWI. Page 7 of 48 Fig.: The slightly thickened walls of the central part show enhancement on Gd-T1WI Page 8 of 48 Fig.: Pathologically, the thickened walls show many glands lined by intestinal-type epithelia that exhibit nuclear stratification and goblet cells are noted. Page 9 of 48 Fig.: Mucinous cystic tumor with a mural nodule (arrows). This part exhibits slight to very low SI and homogenous enhancement. This part is an adenofibroma (It is not a typical "black sponge", but a report showed that typical findings are found in only 43% of the tumors (Jung et al. 2006)). Imaging Findings of MBT: n MBT exhibits a multilocular cystic mass (stained-glass appearance) with partially thickened walls. n On contrast-enhanced MR imaging, the wall exhibits enhancement. n Borderline tumors tend to have a larger number of loculi than adenomas. 3. Mullerian mucinous borderline tumor, MMBT (mucinous borderline tumor, endocervical-like) n MMBT was first described in 1988 by Rutgers and Scully. n Definition: Borderline tumors of low malignant potential exhibiting an epithelial proliferation of mucinous type cells greater than that observed in their benign Page 10 of 48 counterparts but without destructive stromal invasion. The mucinous epithelial cells resemble endocervical epithelium. n Epidemiology: 10-15% of MBT. The average patient's age is 34 years. n Macroscopy: MMBT are bilateral in approximately 40% of cases. MMBT are more often unilocular with intracystic papillae. The papillae that architecturally resemble those of SBT. n Histopathology: They differ from intestinal-type tumors in that the intracystic growth is composed of bulbous papillae similar to those of SBT. n 30% of the cases show endometriosis. 20% of the cases show endometriosis in the ipsilateral ovary, and these endometrioses undergo transition to the neoplastic epithelium. Fig.: An MMBT exhibits polypoid papilla in the endometriotic cyst. The papilla exhibits very high SI with delicate branching core on T2WI (cotton ball-like) and weak enhancement on dynamic contrast study. Page 11 of 48 Fig.: This MMBT exhibits a large papilla in the endometriotic cyst. The papilla exhibits very high SI on T2WI with low SI core, and weak enhancement on dynamic contrast study. Histologically, branching edematous papillae lined by endocervical type mucinous cells are revealed. 4. Mullerian mixed-epithelial borderline tumor, MEBT (Borderline mixed epithelial tumor) n MEBT was first well characterized in 1988 by Rutgers and Scully. n Definition: Borderline tumor composed of an admixture of two or more of the following cell types: endocervical-like mucinous, ciliated serous, endometrioid, and squamous. The second or second and third cell types must comprise alone or together at least 10% of the neoplastic lining. n Epidemiology: MEBT account for 5% of borderline tumors. The average patient's age is 35 years. MEBT are more often seen in premenoposal woman. n Macroscopy: MEBT are bilateral in approximately 22% of cases. MEBT are more often unilocular with intracystic papillae. The papillae architecturally resemble those of SBT. Page 12 of 48 n Histopathology: They exhibit papillae with detached cell clusters reminiscent of SBT, but they generally contain a mixture of endocervical-like cells and indifferent eosinophilic epithelium. n 53% of the cases exhibit endometriosis. 33% of the cases exhibit endometriosis in the ipsilateral ovary. Fig.: An MEBT exhibits polypoid papilla in the endometriotic cyst. This papilla exhibits very high SI in the periphery with low SI core on T2WI. These features resemble those of MMBT. Weak enhancement of this papilla in the periphery is observed on dynamic contrast-enhanced study. Page 13 of 48 Fig.: This MEBT exhibits polypoid papilla in the endometriotic cyst, and these imaging features are similar to MEBT-1; however, the surface of the lesion exhibits high SI on T1WI. Histologically, this portion reflects clots on the surface of the lesion (There is no contrast-enhanced image). Page 14 of 48 Fig.: The papilla exhibits high intensity on T2WI with a low intensity core. Histologically, a severely edematous branching papillae with fibrous core is noted. The high intensity on T2WI may reflect the edematous stroma. Page 15 of 48 Fig.: Histologically, they exhibit finely branching complex papillae with detached cell clusters reminiscent of SBT, but they generally contain a mixture of endocervical-like cells (mucinous, serous and endometrioid) and indifferent eosinophilic epithelium. Imaging findings of MMBT/MEBT n MMBT/MEBT exhibit polypoid papilla in the endometriotic cysts. The papilla exhibits very high SI with delicate branching core on T2WI (cotton ball-like) and weak enhancement on dynamic contrast-enhanced study. n The high SI on T2WI may reflect the edematous stroma. n The imaging findings of MMBT and MEBT are resemble. 5. Endometrioid Borderline Tumor n Definition: An ovarian tumor of low malignant potential composed of atypical or histologically malignant endometrioid type glands or cysts, often set in a dense fibrous stroma with absence of stromal invasion. n Epidemiology: Rare (they account for 3-18% of malignant ovarian neoplasms) Page 16 of 48 n More than 15-50% have endometriosis in the ipsilateral ovary. Often unilateral. n Histopathology: Adenofibromatous (common) Villoglandular or papillary Combination of villoglandular and adenofibromatous Fig.: A large solid mass in the endometriotic cyst is observed. The mass primarily exhibits intermediate homogenous SI on both T1 and T2WI, but the central portion exhibits high SI on both T1 and T2WI. Page 17 of 48 Fig.: The mass exhibits gradual enhancement on dynamic study. On early image, reticular linear enhancement is seen. The central portion exhibits no enhancement. Page 18 of 48 Fig.: Histologically, atypical or malignant endometrioid type glands set in a dense fibrous stroma with absence of stromal invasion. The central portion contains hematoma. 6. Borderline Brenner Tumor n Definition: An ovarian transitional cell tumor of low malignant potential with atypical or malignant features of the epithelium but lacking obvious stromal invasion. n Epidemiology: Only 3-5% of Brenner tumors. They are confined to the ovary and, with rare exceptions, have been unilateral. The average patient's age is 59 years. n Brenner tumors are associated with another tumor type, usually mucinous cystadenoma (25%). n Macroscopy: Typically large (median; 16-20cm). They usually have a solid component resembling benign Brenner tumor as well as a cystic component containing a papillary or polypoid mass. Page 19 of 48 n Histopathology: Borderline Brenner tumors exhibit a greater degree of architectural complexity than benign Brenner tumors. Typically, a benign Brenner tumor component is also present. n Imaging Findings: Higher SI than benign counter part on T2WI (Takeuchi, et al. 2008). Fig.: A solid and cystic mass is shown. The solid portion exhibits calcification on CT. On T2WI, the upper part of the solid portion exhibits intermediate SI (arrows) and the lower part exhibits very low SI. Typical benign Brenner tumors exhibit very low SI on T2WI. Page 20 of 48 Fig.: The solid portion exhibits gradual enhancement on dynamic study. Diagnostic clues of surface epithelial borderline tumors n Prominent papillary projection than their benign counterpart (especially SBT) n No invasive extension, ascites and lymphadenopathy n Relatively younger than cases with malignant tumor n Borderline Brenner tumor exhibits higher SI on T2WI Sexcord-Stromal Tumor 7. Granulosa cell tumor n Account for 1.5% (range, 0.6-3%) of all ovarian tumors. The tumor occurs in a wide age range. Page 21 of 48 n The tumors produce or store a variety of steroid hormones (most are estrogenic, but rarely androgenic activity may occur). The tumor can induce pseudoprecocious puberty, menstrual disorders and irregular uterine bleeding. n Two major subtypes are recognized: adult type (more than 95%) and juvenile type n Adult type exhibits admixture of cystic and solid areas. The tumor cells have a nuclear groove (juvenile type lacks of nuclear groove). n Imaging findings: multilocular or solid and cystic mass with hemorrhage. Fig.: Case 1. A large multilocular mass. This case is a postmenopausal woman, but a large uterus is noted (arrow).Case 2. Mainly, the mass exhibits low SI on both T1 and T2WI with cystic parts. High SI, which reflects the hemorrhage, is observed on T1WI. Germ Cell Tumor 8. Carcinoid Page 22 of 48 n These tumors contain neuroendocrine cells. extensive components of well-differentiated n They may occur in pure form or within a dermoid cyst, a mucinous cystic tumor or a Brenner tumor. n Subtypes: Insular, trabecular, mucinous and strumal. n Carcinoid syndrome occurs in 3.2-30% n Peptide YY production by the tumor cells causes severe constipation in trabecular carcinoids. n Carcinoids are immunoreactive to the neuroendocrine markers (chromogranin A, synaptophysin, Leu-7, grimelius stain) . Fig.: A large multilocular mass exhibits a solid portion. The solid portion exhibits relatively high SI on T1WI, low SI on T2WI and homogeneous enhancement on FS-GdT1WI.A fatty component is noted (arrow). Page 23 of 48 Fig.: The solid portion of this case exhibits low SI on T2WI and high SI on T2WI: We speculate that the stromal fibrosis, hemorrhage and neuroendocrine granules may affect the SI. Images for this section: Page 24 of 48 Fig. 1: Serous borderline cystic tumor exhibiting polypoid excrescences in the cyst. Page 25 of 48 Fig. 2: On T2-weighted images (T2WI), the excrescence exhibited a "broccoli"-like appearance, and had low signal-intensity (SI) stalk with delicate branching. This reflects the histologic hierarchical branching. Page 26 of 48 Fig. 3: Histologically, the stroma exhibits dense collagen and hyalinization (a), and severe edematous change in the surface (b). Macroscopically, this edematous region appears as many cyst-like nodules (arrows). Page 27 of 48 Fig. 4: A serous tumor can be confined to the right ovarian surface (arrows), and typical cystic mass with excrescences in the contralateral ovary. Serous tumors are often bilateral with different growth pattern and grade. Page 28 of 48 Fig. 5: A large, multilocular cystic mass exhibits a typical, "stained-glass" appearance. In particular, the central part exhibits many tiny loculi with thickening of the walls. This part shows a high SI on DWI. Page 29 of 48 Fig. 6: The slightly thickened walls of the central part show enhancement on Gd-T1WI Page 30 of 48 Fig. 7: Pathologically, the thickened walls show many glands lined by intestinal-type epithelia that exhibit nuclear stratification and goblet cells are noted. Page 31 of 48 Fig. 8: Mucinous cystic tumor with a mural nodule (arrows). This part exhibits slight to very low SI and homogenous enhancement. This part is an adenofibroma (It is not a typical "black sponge", but a report showed that typical findings are found in only 43% of the tumors (Jung et al. 2006)). Page 32 of 48 Fig. 9: An MMBT exhibits polypoid papilla in the endometriotic cyst. The papilla exhibits very high SI with delicate branching core on T2WI (cotton ball-like) and weak enhancement on dynamic contrast study. Page 33 of 48 Fig. 10: This MMBT exhibits a large papilla in the endometriotic cyst. The papilla exhibits very high SI on T2WI with low SI core, and weak enhancement on dynamic contrast study. Histologically, branching edematous papillae lined by endocervical type mucinous cells are revealed. Page 34 of 48 Fig. 11: An MEBT exhibits polypoid papilla in the endometriotic cyst. This papilla exhibits very high SI in the periphery with low SI core on T2WI. These features resemble those of MMBT. Weak enhancement of this papilla in the periphery is observed on dynamic contrast-enhanced study. Page 35 of 48 Fig. 12: This MEBT exhibits polypoid papilla in the endometriotic cyst, and these imaging features are similar to MEBT-1; however, the surface of the lesion exhibits high SI on T1WI. Histologically, this portion reflects clots on the surface of the lesion (There is no contrast-enhanced image). Page 36 of 48 Fig. 13: The papilla exhibits high intensity on T2WI with a low intensity core. Histologically, a severely edematous branching papillae with fibrous core is noted. The high intensity on T2WI may reflect the edematous stroma. Page 37 of 48 Fig. 14: Histologically, they exhibit finely branching complex papillae with detached cell clusters reminiscent of SBT, but they generally contain a mixture of endocervical-like cells (mucinous, serous and endometrioid) and indifferent eosinophilic epithelium. Page 38 of 48 Fig. 15: A large solid mass in the endometriotic cyst is observed. The mass primarily exhibits intermediate homogenous SI on both T1 and T2WI, but the central portion exhibits high SI on both T1 and T2WI. Page 39 of 48 Fig. 16: The mass exhibits gradual enhancement on dynamic study. On early image, reticular linear enhancement is seen. The central portion exhibits no enhancement. Page 40 of 48 Fig. 17: Histologically, atypical or malignant endometrioid type glands set in a dense fibrous stroma with absence of stromal invasion. The central portion contains hematoma. Page 41 of 48 Fig. 18: A solid and cystic mass is shown. The solid portion exhibits calcification on CT. On T2WI, the upper part of the solid portion exhibits intermediate SI (arrows) and the lower part exhibits very low SI. Typical benign Brenner tumors exhibit very low SI on T2WI. Page 42 of 48 Fig. 19: The solid portion exhibits gradual enhancement on dynamic study. Page 43 of 48 Fig. 20: Case 1. A large multilocular mass. This case is a postmenopausal woman, but a large uterus is noted (arrow).Case 2. Mainly, the mass exhibits low SI on both T1 and T2WI with cystic parts. High SI, which reflects the hemorrhage, is observed on T1WI. Page 44 of 48 Fig. 21: A large multilocular mass exhibits a solid portion. The solid portion exhibits relatively high SI on T1WI, low SI on T2WI and homogeneous enhancement on FS-GdT1WI.A fatty component is noted (arrow). Page 45 of 48 Fig. 22: The solid portion of this case exhibits low SI on T2WI and high SI on T2WI: We speculate that the stromal fibrosis, hemorrhage and neuroendocrine granules may affect the SI. Page 46 of 48 Conclusion Conclusion n It is important to know the characteristics of ovarian borderline tumors to distinguish them from highly malignant tumors. n In particular, in cases of tumors associated with endometriosis, careful interpretation is recommended. Personal Information Roka Namoto Matsubayashi, MD, ph D. Department of Radiology and Co-Director of Breast Care Center National Hospital Organization Kyushu Medical Center 1-8-1 Jigyohama Chuo-ku Fukuoka 810-8563, Japan Tel: +81-92-852-0700 Fax: +81-92-847-8802 E-mail: rokan@qmed.hosp.go.jp or rokan@kyumed.jp References 1. Fattaneh Tavassoli and Peter Devilee (ed). World Health Organization Classification of Tumours. Pathology and Genetics Tumours of the Breast and Female Genital Organs. IARC Press. Lyon, 2003 2. Tanaka YO, Nishida M, Kurosaki Y, et al: Differential diagnosis of gynaecological ''stained glass'' tumors of MRI. Br J Radiol 72: 414-420,1999 3. Okamoto Y, Tanaka YO, Tsunoda H, et al: Malignant borderline mucinous cystic neoplasms have a larger number of loculi than mucinous cystadenoma: a retrospective study with MR. J Magn Reson Imaging 26:94-9, 2007 Page 47 of 48 4. Jung DC, Kim SH, Kim SH. MR imaging findings of ovarian cystadenofibroma and cystadenocarcinofibroma: clues for the differential diagnosis. Korean J Radiol 7:199-204, 2006 5. Sciarra JJ. Gynecology and obstetrics. In CC Bird, TW McElin, TA Victor (ed). Benign noeplasm of the ovary. JB Lippincott Co Philadelphia, p12, 1988 6. Disaia PJ. Ovarian neoplasms. In Scott JR, Philip LD, Hammond CB, Spellact WN (ed). Danforth's Obstetrics and Gynecology (7th edn). JB lippincott Co. Philadelphia, p998, 1994 7. Davis KP, Hartmann LK, Keeney GL, et al. Primary ovarian carcinoid tumors. Gynecogic Oncology 61:259-265, 1996 8. Zaloudek C, Norris HJ:Granulosa cell tumoe of the ovary in children. A clinical and pathologic study of 32 cases. Am J Surg Pathol 6:503-512, 1982 Page 48 of 48