Day-PIV of Blood Pump, Time Varying
advertisement

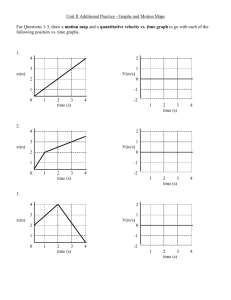
PIV Measurements of Flow in a Centrifugal Blood Pump: Time-Varying Flow Steven W. Day1 e-mail: sday@alumni.virginia.edu James C. McDaniel The University of Virginia, Charlottesville, VA 22903 Measurements of the time-varying flow in a centrifugal blood pump operating as a left ventricular assist device (LVAD) are presented. This includes changes in both the pump flow rate as a function of the left ventricle contraction and the interaction of the rotating impeller and fixed exit volute. When operating with a pulsing ventricle, the flow rate through the LVAD varies from 0 – 11 L / min during each cycle of the heartbeat. Phaseaveraged measurements of mean velocity and some turbulence statistics within several regions of the pump, including the inlet, blade passage, exit volute, and diffuser, are reported at 20 phases of the cardiac cycle. The transient flow fields are compared to the constant flow rate condition that was reported previously in order to investigate the transient effects within the pump. It is shown that the quasi-steady assumption is a fair treatment of the time varying flow field in all regions of this representative pump, which greatly simplifies the comprehension and modeling of this flow field. The measurements are further interpreted to identify the effects that the transient nature of the flow field will have on blood damage. Although regions of recirculation and stagnant flow exist at some phases of the cardiac cycle, there is no location where flow is stagnant during the entire heartbeat. 关DOI: 10.1115/1.1865190兴 Introduction Left ventricular assist devices 共LVADs兲 have proven clinical efficacy, but there are currently no devices capable of providing long-term 共10 or more years兲 of support. The newest generation VADs are magnetically suspended rotary blood pumps and have the potential to replace diaphragm pumps. They offer the advantages of requiring significantly fewer moving parts, no contacting moving surfaces, no flexible materials, and no valves. All of these increase the mechanical life of the device and decrease the potential blood damage caused by the pump. The fluid dynamics within the pump both contribute to damage caused to the blood that it is pumping and determine the pump performance and efficiency. An understanding and ability to predict the flow within these devices is critical. In addition to the three-dimensional geometry of the pump, transient effects complicate the flow. Transient effects include both the interaction of the blades with the fixed geometry of the pump and the time-varying flow rate due to pulsing of the native left ventricle. Although the pump operates at a constant rotational speed, the flow rate varies as a result of the ventricle contraction changing the pump inlet pressure. When implanted, the flow rate varies from the high-flow to low-flow condition during each heartbeat, so that the changes in flow rate from low to high occur in a short period of time 共⬃0.25 s兲. The fact that the flow through the pump is pulsed may have some physiological advantages 共because blood flow delivered form the heart is normally pulsed兲, but it also leads to a very complicated time-dependent flow within the pump. The use of particle-based optical techniques for studying fluid dynamics of blood pumps is common. These majority of fluid dynamics studies of rotary pumps present qualitative 关1–4兴 or quantitative 关5–8兴 measurements of the flow within one or more regions of the pump at one operating flow rate. The transient effects of the interaction of the rotating impeller 1 Corresponding author. Current address: Section of Evolution & Ecology, University of California, One Shields Avenue, Davis, CA 95616 Contributed by the Bioengineering Division for publication In the JOURNAL OF BIOMECHANICAL ENGINEERING. Manuscript received October 7, 2003. Final manuscript received September 20, 2004. Associate Editor: C. Ross Ethier. 254 / Vol. 127, APRIL 2005 and fixed volute, so called rotor-stator interactions, have been reported by Tsukiya et al., who used particle image velocimetry 共PIV兲 to measure the variations in the velocity field within the blade passage of a scaled model pump as a function of the position of the passage relative to the volute cutwater 关9兴. Flow structures that existed within the blade passage were largely a function of position relative to the cutwater. Efforts to investigate the flow field over a range of flow rates have increased with awareness that the flow rate through the pump will vary during the heartbeat, even while the pump is operating at constant rotational speed. Qualitative flow visualization by Wu et al. within both an axial and a centrifugal pump at design and off-design conditions showed that the flow field exhibits undesirable flow structures at both higher and lower than design flow rates 关10兴. Manning and Miller characterized the flow within the outlet cannula of a pump over a range of flow rates ranging from ⬃1.5 to 10.5 L / min 关11兴. Apel et al. presented measurements of the angle of fluid at the exit of an axial pump over a range of flow rates 共1 – 4.5 L / min兲 in order to validate computational models through this pump 关4兴. The authors are not aware of any studies that have characterized the flow field in a rotary pump during pulsatile flow rate conditions. All reported measurements of the flow through pulsatile diaphragm-type pump are necessarily for time-varying flow, due principally to the fact that these devices generate a pulsed flow even when operating against constant resistance. Orime et al. presented particle streak patterns to reveal flow patterns and some measurements of mean speed in a total artificial heart over the cycle of heart beat by making measurements at approximately 20 times during the cycle 关12兴. Additionally, quantitative studies, using laser Doppler velocimetry 共LDV兲 关13,14兴 and PIV 关15兴 have been used to measure characteristics of pulsatile flow through diaphragm-type pumps. The synchronization of measurements to the cycle of periodic phenomenon is known as phase-averaging. This method has been applied to the determination of mean flow and turbulent stresses within blood pumps based on LDV measurements 关13兴. The methods are used extensively in the treatment of rotor-stator interactions on large-scale machines, and discussions on the accuracy of methods can be found in 关16,17兴. Copyright © 2005 by ASME Transactions of the ASME Fig. 1 Cut-away view of the pump showing the location of the three measurement planes within the pump: IE-inlet elbow, BPBlade passage, CW-Cut-water. While some of these studies of rotary blood pumps have characterized the flow field over a range of steady flow rates, none have presented measurements of the flow field during pulsatile conditions that would enable the evaluation of the effect of transient variations in flow rate. In the current study, particle image velocimetry 共PIV兲 was used to characterize the flow within a centrifugal LVAD under a time-varying flow rate that is representative of the conditions when implanted. Additionally, the study includes a prediction of the effects that specific flow features will have on blood damage. This work addresses the effects of a timevarying flow field due to these rapid changes in flow rate through the pump, by using PIV to make quantitative measurements of the mean velocity and stress fields within the pump. Measurements reported elsewhere characterize the flow field over the range of steady flow rates at which this particular pump is expected to operate 关18兴. In order to characterize the influence of the transient flow rate, measurements of the internal flow field were made while the pump operated within a mock circulatory system, which included a model of a beating left ventricle. Additionally, comparisons of the transient flow field to the steady flow field are presented in an effort to characterize the time-dependent effects on the flow field. Methods Experimental Apparatus. Particle image velocimetry 共PIV兲 is a technique that measures the instantaneous velocity field within an illuminated plane of the fluid field using light scattered from particles seeded into the fluid 关19兴. The light scattered from these particles is collected and imaged using a camera at two separate times so that the displacement of the particles can be measured. PIV measures the instantaneous two-dimensional field illuminated by the laser sheet and is therefore well suited for investigating transient phenomena. Details on the PIV system, seed particles, test fluid, and software 关20兴 used during these experiments have been reported elsewhere 关18,21兴. In order to accomplish PIV measurements within the LVAD, a prototype pump that allows for optical access into nearly all interior regions of the pump was designed and built, as described elsewhere 关18,21兴. A cutaway view of the pump showing locations of the measurement planes is shown in Fig. 1. The pump is part of a mock circulatory loop that includes a left ventricular simulator 共to model the beating native left ventricle兲, an adjustable valve 共to control the systemic resistance兲, and two air-filled compliance chambers 共in which the compressibility of air models the elasticity of blood vessels兲, and is shown schematically in Fig. 2. The loop Journal of Biomechanical Engineering Fig. 2 Schematic of flow loop showing pulsed ventricle simulator „PVS…, Left Ventricular Assist device under investigation „LVAD…, arterial compliance „AC…, venous compliance „VC…, and valve for systemic resistance „R…. Measurements of flow rate include flow through aortic valve „AoQ… and flow through LVAD „VADQ…. Locations of pressure measurements are aortic pressure „AoP…, ventricular „LVP…, and atrial „LAP…. is instrumented with two flow meters 共Transonic, Ithaca, NY兲 and three pressure transducers 共Validyne, Northridge, CA兲 to monitor the transient behavior of the ventricular simulator and LVAD under simulated physiologic conditions. The values of resistance and compliance, as well as the pulse rate and strength of the ventricle simulator, are adjustable so that the pump may be tested for a range of physiologic conditions. Modeled conditions are confirmed to be physiologically relevant by comparing them to data on the behavior and performance of the human circulatory system 关22,23兴. A cannula is connected from the apex of the left ventricle to the inlet elbow of the pump. When making measurements in the inlet elbow, an additional length of straight tubing is added to the cannula before entering the inlet elbow in order to ensure the same entrance length as was used for the constant flow rate experiments. During pulsatile flow experiments, a LabView® program was used to display and record transient data, including LVAD flow rate, ventricle flow rate, left ventricular pressure, aortic pressure, venous pressure, working fluid temperature, rotational speed, and the axial force on impeller. LabView was also used to control the motor speed via a simple closed-loop feedback controller that maintains the pump operating speed to within 20 rpm of the requested shaft speed, ⬃ ± 1%. The synchronization of the PIV system to the heartbeat and to the rotating shaft was accomplished by electrical triggers from both the shaft and left ventricle simulator. Both were fed through the digital delay generators and a logical “and” circuit was implemented in hardware to ensure that the measurement was synchronized to both the heartbeat and blade passage. For each measurement, 200 images were acquired at each phase of the heartbeat and processed to arrive at the statistical quantities of the velocity field that are presented here. Mean and Turbulence Statistics. According to the Reynolds decomposition, the instantaneous velocity ũ is though to be composed of a steady mean velocity U summed with a fluctuating velocity u. All fluctuations, including those from turbulence and from large-scale nonrandom phenomena, contribute to u. The magnitude of the mean U and standard deviation u⬘ of the instantaneous velocity ũ are statistical descriptions of the flow and can be found from a set of instantaneous velocity measurements, each made at discrete times, by ensemble averaging 关24兴. Reynolds normal and shear stresses are also determined from this series of instantaneous measurements. Principal stress analysis, as outlined by Baldwin 关25兴 was used to calculate the maximum Reynolds stress based on measurements in the measurement reference APRIL 2005, Vol. 127 / 255 Fig. 3 Measured physiological pressures and flow rates for a rotary LVAD over two heartbeats. Pump speed is constant at 2100 rpm. frame. In the case of a periodic flow, velocity variations are no longer due exclusively to random fluctuations, but also to the periodicity of the mean flow. In a blood pump, these periodic variations are due to the pulsed flow rate through the pump and, in some regions, to interactions between the rotating and stationary parts of the pump. When this is the case the instantaneous velocity can be decomposed into components according to ũ = U + u + ublade + upulse 共1兲 where the variations in instantaneous velocity include the variations due to blade passage ublade and to the heartbeat upulse in addition to statistically random variations u. Because the blade passage and pulse cycle can be considered periodic, requiring that the nonrandom quantities of the flow field are repeatable from cycle to cycle, they can be treated in a more exact way. The periodic velocity fields can be represented by ũ共b, p兲 = U共b, p兲 + u共b, p兲 共2兲 The instantaneous flow conditions ũ are still thought of as the summation of a periodically oscillating mean flow U and fluctuations u. However, the velocities no longer represent time-averaged quantities, but rather characterize the velocity measured at one distinct phase of the periodic phenomena. All are functions of the phase of blade passage b and pulse p. U共b , p兲 is not a steady mean flow, but rather a mean flow which varies periodically as a function of the blade passage and heartbeat. While U共b , p兲 is the same for a given phase of heartbeat and blade position, the instantaneous velocity field ũ共b , p兲 is not necessarily the same because this includes the contribution of the random fluctuations u共b , p兲. The phase-averaged statistics are calculated according to the same equations, but all of the instantaneous measurements ũ共b , p兲 are made at the same phase of both the blade passage or the heartbeat. Equations 共1兲 and 共2兲 may be related by realizing that ublade is the rms of U共b , p=const兲 for b = 0 to 2 over a full cycle of blade phases. Similarly, upulse represents the magnitude of variations of mean velocity during one pulse cycle rms 兵U共b=const , p兲 for p = 0 to 2其. Additional reference on phaseaveraging techniques using PIV data may be found in Zhang et al. 关17兴, Sinha et al. 关26兴, Wernert and Favier 关16兴, and Wernet 关24兴. Blade-to-Blade Variations. The velocity within the blade passage of a centrifugal pump is not uniform. Generally, the velocity at the exit of the blade passage is highest near the suction side 共the blade face away from the direction of rotation兲 of the blade and lowest near the pressure side 共toward the direction of rotation兲 of the blade 关27兴. Because of this some periodicity is expected as the result of interactions between the rotating and stationary parts of the pump, even at a steady flow rate 关28兴. According to Eq. 共1兲, 256 / Vol. 127, APRIL 2005 the magnitude of the velocity fluctuations caused by the passing of the blade is quantified by comparing measurements in which the data acquisition is not synchronized to the position of the impeller, “free-running mode,” and measurement for which the acquisition is synchronized with rotational position to insure phase-averaged measurements at one specific phase of the blade passing event, “passing-blade mode.” For the purposes of investigating blade-toblade variations, the flow rate through the pump is held constant to eliminate further variations due to flow rate. Statistical treatment of free-running measurements 共no consideration of blade phase兲 includes influences of the both random variations u and variations due to blade passage. Because the blade passage is periodic, fluctuations due to blade passage can be treated as functions of the phase of blade passage, rather than as a random phenomenon, as was shown in Eqs. 共1兲 and 共2兲. Measurements for 20 phases of blade position are reported for several constant flow rates. The variations due to the passing blade are removed because all images are acquired at one particular phase of the blade passage. The rms of the fluctuating velocity u⬘共b兲 is a measure of the magnitude of u共b兲. The mean of the instantaneous fields is U共b兲, where b is the phase of the impeller. Selection of Operating Condition. A single set of operating conditions for testing pulsatile flow was established based on the measurements of the global pump performance over a range of physiologic conditions. The time variations of ventricular and aortic pressures and flow rates through the LVAD and aortic valve are shown in Fig. 3. The ventricle simulator was beating at 60 beats/ min with a systolic duration of 0.40 s and a diastolic duration of 0.60 s. The strength of the ventricle’s contraction was set so that the left ventricular pressure varied from 10 to 90 mmHg, which is sufficiently high that the aortic valve opens with each pulse. The systemic resistance remained constant, and the LVAD rotational speed was adjusted to achieve a 6 – 7 L / min combined flow rate through the LVAD and the native aorta. This occurred at a speed of 2100 rpm. Under these conditions, the flow rate through the LVAD varies from approximately 1 L / min during diastole to 11 L / min during systole for a mean LVAD flow of 6 L / min. The combined flow rate of the heart and the assist pump is about 7 L / min at a mean aortic pressure of 95 mmHg and atrial pressure of 10 mmHg 共Fig. 3兲. The rotational speed remained at 2100 rpm and all other variables remained the same for all of the experiments presented herein. It is realized that the actual values of left ventricle pressure, peripheral resistance, and compliance are highly variable from patient to patient and will change within any single patient. While the nominal conditions used here are completely realistic, they correspond to a ventricle with a significant pulse pressure when on ventricular assist. Nonetheless, for the purposes of prescribing Transactions of the ASME some realistic conditions to the pump in order to investigate the internal fluid dynamics, this is an ideal test case for measurements of pulsed flow because the variations in flow rate through the pump 共from 1 to 11 L / min during each heart beat with a mean of 6 L / min兲 are extreme for this situation. This represents an upper limit of the variations in flow rate and can, therefore, be used to bound the effect of transient flow rate. A reference phase, = 0 is assigned to a measurement near the end of diastole, 0.15 seconds before the contraction of the ventricle and corresponding increase in LVAD flow rate begin. Phaseaveraged measurements were made at 20 phases 共every 0.05 s兲 of the heartbeat, and are illustrated by symbols in Fig. 3. The selected phases are chosen to show portions of the pulse during which transient effects are most prominent. Unsteady versus Quasi-Steady Flow. One method to characterize the transient effects within a flow is to compare the instantaneous or phase-averaged velocity and shear field to that of steady flow at the same flow rate. If the frequency of oscillation is significantly low, then the fluid behaves quasi-steadily. This is to say that the instantaneous velocity and shear fields are essentially identical to those of steady flow at the instantaneous flow rate. However, at a certain frequency of oscillation, the high acceleration forces become significant and the instantaneous fluid field differs from the steady case. Although theoretical estimates of this critical frequency are available for simple geometries, the application of this theory to the heart pump is complicated by both the geometry and the fact that turbulent momentum transfer dominates over molecular viscosity in most regions of the pump. Because of these complications, a direct comparison of the phase-averaged and steady-state flow fields is used here. Within each configuration, measurements of the instantaneous flow field for pulsatile flow are compared with steady flow measurements at the same or similar flow rates to determine the validity of the quasi-steady assumption. Fig. 4 Phase averaged speed in the inlet elbow at 8 phases with phase, , and flow rate, Q, indicated for each. Results Time-Varying Flow Rate. Contour plots of mean velocity within the inlet elbow are shown in Fig. 4 at phases 0 to 16 / 10. Four of them 共 = 0 , 2 / 10, 4 / 10, 6 / 10兲 cover the sudden increase in flow rate during the beginning of systole, and four of them 共 = , 12 / 10, 14 / 10, 16 / 10兲 cover the transition from systole to diastole. The strong contraction of the ventricle begins just after 2 / 10 共flow rate, Q, ⬃1 L / min兲 and changes to 11 L / min in 0.2 s. Similarly, between phases of and 14 / 10, the flow rate drops from 10.5 to 1 L / min during 0.2 s. There are obvious recirculation patterns within the inlet elbow at the low flow condition. These recirculation regions form at the beginning of diastole and continue until the heart contracts 共13 / 10– 3 / 10兲. Profiles of mean velocity and rms as a function of z position are shown in Fig. 5 to illustrate the time evolution during the acceleration phase. The position of the profile is y = −0.022 m, which is very near the inlet of the elbow. The same charts show the velocity and rms profiles for steady flow at 11 L / min as a dashed line, for comparison to the pulsed flow cases. The profile of speed quickly reestablishes itself during the contraction after the sudden acceleration of flow. As compared to the steady case, the shape of the velocity profile is significantly flattened at 4 / 10– 5 / 10 and slightly so at 6 / 10, but is essentially identical to the steady flow case by 7 / 10. The velocity profile is completely established between 0.15 s 共3 / 10兲 and 0.2 s 共4 / 10兲 after the sudden acceleration begins and is never very different from the steady flow profile. The rms of velocity, however, does not exhibit as rapid a response to the sudden change in flow rate. The rms of velocity does not approach the steady-state profile until approximately 9 / 10. Journal of Biomechanical Engineering At 7 / 10, the flow rate is high 共⬎8 L / min兲, but levels of rms are everywhere lower than 0.05 m / s. This is about one-third of the steady-state values reported at 9 L / min. Profiles of mean and rms of velocity are also shown in this same section during the deceleration of flow at the end of systole in Fig. 5. Between 13 / 10 and 15 / 10, the flow along the outer curvature of the elbow reverses direction even though the pump flow rate is positive, creating a recirculation region 共Fig. 5兲. This recirculation region persists throughout diastole, is not present during steady flow conditions at 1 L / min and is the most pronounced transient effect within the pump. Contour plots of the mean velocity are shown at the same phases of the heartbeat within the blade passage in Fig. 6. The flow within the blade passage at all flow rates is nearly identical to the steady flow case at the same flow rate. This is demonstrated in Fig. 7, which shows the mean velocity, rms, MRSS, and viscous shear at one phase in the heartbeat. The selected phase of 13 / 10 is immediately following the sudden deceleration in the flow, but the similarity between phase-averaged and steady flow cases is evident at all phases of the heartbeat. Contour plots of the mean velocity in the cutwater are in Fig. 8. The flowfield within the cutwater region responds very quickly to the sudden flow acceleration at the beginning of systole. Profiles 共at x = 0.02 m兲 of the mean speed and MRSS are shown for all measured phases in Fig. 9. Mean velocity, rms, MRSS, and viscous shear stress are nearly identical to the steady-state measurements at approximately the same flow rate, other than the fact that the size of the recirculation zone for the phase-averaged case is slightly larger than for steady case. At each phase, the steady profiles at the nearest steady flow rate are also shown as a dashed APRIL 2005, Vol. 127 / 257 Fig. 5 Time evolution of mean speed and rms of fluctuating velocity near the inlet of inlet elbow during the rapid acceleration of flow and through systole and then through deceleration and diastole compared to steady flow at 11 L / min line. The profiles of mean velocity show that the size of the recirculation region changes between phases 5 / 10 and 7 / 10, but is reestablished at 7 / 10. The recirculation region in the pulsatile case is more pronounced than for the steady flow case. The recirculation region continues during the deceleration of flow to 12 / 10, at which time the flow rate is 9 L / min. At 13 / 10, the flow rate has dropped to 4 L / min and the recirculation region does not exist, as it the case for steady flow. Blade-to-Blade Variations. A comparison of measurements of steady flow that are not synchronized 共top兲 and synchronized 共middle and bottom兲 to the phase of the blade passage is shown in Fig. 10. The top images show mean speed U and rms u⬘ = rms共u + ublade兲. The middle and lower images show mean velocity U共b兲 258 / Vol. 127, APRIL 2005 and rms u⬘共b兲 at two phases of the blade passage acquired by synchronizing the acquisition to a specific phase of the blade position. The first is at a reference phase b of zero degrees, when the impeller blade is just passing the cutwater tongue and the second when the cutwater is centered between two blades, b = 180. Passing blade measurements were made at 20 phases of the blade passage and for three different flow rates, 3, 6, and 9 L / min. Measurements here are shown only for two phases because they represent the extremes of the cyclical variations, which are generally small. Blade-to-blade variations of the mean velocity are evident within the 2 mm outside of the impeller outer diameter 共gray line in Fig. 10兲. Immediately downstream of the blade, the mean veTransactions of the ASME Fig. 7 Phase-averaged flowfield at 13 / 10 in the blade passage compared to steady-state measurement at approximately the same flow rate, 4.5 L / min Fig. 6 Mean Speed in the blade passage locity is 2.3 m / s, whereas it is 2.7 m / s for the majority of the blade passage. To an observer fixed relative to the housing and near the impeller exit, the velocity would vary as a function of blade passage. It can also be seen that there is very little difference between the three cases except within the regions near the outer diameter of the impeller. The mean velocity and rms of fluctuating velocity fields are nearly the same for the 0 and 180 deg blade phases. This can be written as Ui,j共b = 180兲 ⬇ Ui,j共b = 0兲. Additionally, they look nearly identical to the circumferentially averaged case shown at the top of the figure. This indicates that the effect of the blade passage is minimal, i.e., ublade is small. The limited effect of blade-to-blade passage was also seen for flow rates of 3 and 9 L / min. The separation at the volute tongue and resulting separation region present at 9 L / min is not affected by the blade passage. Another way to interpret the measurements is by observing the levels of rms for the circumferentially averaged and the phaseaveraged cases. Variations due to the blade passage contribute to the rms for the free-running measurements, but not to the rms of the phase-averaged measurements. The fact that the levels of rms of fluctuating velocity are very nearly the same, except immediately adjacent to the impeller, for the free-running and phaseaveraged measurements, demonstrates that the blade passing has very little effect on the velocity field in this region. This can be written as u + ublade ⬇ u共b兲, therefore, ublade ⬇ 0. Within 2 – 3 mm Journal of Biomechanical Engineering outside the impeller diameter, levels are slightly 共⬃0.05 m / s兲 higher for the free-running case than for the frozen-blade cases. This is because the variation of mean velocity as the blade passes contributes to the levels of rms only in the free-running case. The magnitude of ublade is less than 0.1 m / s immediately adjacent to the blade and approximately zero further from the blade. This is ⬍25% of the levels of rms caused by random fluctuations. Error Analysis. Statistical quantities estimated based on phaseaveraging assume that the flow is periodic and also constant during the acquisition period for every phase. Ideally, the magnitude of fluctuations and statistical quantities is affected by only random turbulent fluctuations of the fluid velocity. Realistically, two additional factors, cycle-to-cycle variations and finite duration of phase window contribute to the statistical describing the flow. In these experiments, the first of these factors corresponds to variations in the transient flow rate caused by the beating ventricle from one heartbeat to the next. The range of instantaneous flow rates at any given phase due to the cycle-to-cycle variation is a maximum of ±0.5 L / min with a standard deviation of 0.3 L / min 共3% of the maximum flow rate and 50% of the lowest flow rate兲. During pulsatile flow, the rms of phase-averaged velocity measurements at some locations 共inlet elbow centerline at 7 / 10 shown in Fig. 4兲 is as low as 3% of the maximum mean velocity, indicating that the combined effects of the cycle-to-cycle variations have an rms of less than 3% of the maximum measured values. Similarly, even if the flow rate is exactly periodic, the mean flowfield may not be exactly periodic. This is particularly evident APRIL 2005, Vol. 127 / 259 waiting for the first blade passage during the correct phase of the heartbeat, the effective phase-averaging window size is 0.0057 s 共blade-passing period at 2110 rpm兲, or 2 deg of the pulse cycle. During the sudden flow deceleration at the end of systole, the flow rate changes approximately 0.4 L / min during a 0.0057 s time period. If measurements are distributed randomly within this phase window, the rms of the variation of flow rate is ⬃0.1 L / min, which is about 1% of the maximum flow rate. Measurements presented for pulsatile flow within the blade passage are most affected by this at phases of 2 / 10 and 12 / 10, during the rapid acceleration and deceleration of the flow. A comparison of the flowfield at 12 / 10, shown in Fig. 11, reveals that the levels of rms are slightly 共⬃0.1 m / s or 3% of the mean velocity兲 higher in this case than for the steady flow case. This is in contrast to the case shown at 13 / 10, as was shown in Fig. 7, at which phase the levels of all statistics are identical to the corresponding steady flow case. Discussion and Conclusions Fig. 8 Phase averaged mean velocity field in the cut-water at 8 phases of pulsatile flow in the inlet elbow during pulsed flow. Two adjacent counterrotating vortices form during diastole near the center of the inlet elbow. The exact position of these vortices is not exactly the same during each heartbeat, so a fixed point within the elbow may be at a different position within a vortex during each hearbeat. The inclusion of these cycle-to-cycle variations in the statistical treatment of velocity leads to artificially high values of rms and Reynolds stresses. In this case, statistics, such as rms and MRSS, do not characterize small-scale random variations of the flow, but rather are artifacts of cycle-to-cycle variations in the flow. The second effect is caused by acquiring data over a finite duration of phase and statistically treating this as though it were all acquired at the identical phase. This is often done in phaseaveraged measurements to increase the amount of data obtained. The length of this phase duration is known as the phase-averaging window size and is typically anywhere from 0.2 to 10 deg in published experiments. The effects of this on statistical treatment of phase-averaged measurements are discussed in detail in Zhang et al. 关17兴. For experiments within the inlet elbow and cutwater, image acquisition was synchronized to only the heartbeat and images were acquired at a precise phase of the heartbeat to within less than 10−10 s 共the jitter of the laser兲. In this case, only cycle-tocycle variations contributed to derived statistics. For measurements in the blade passage, the measurement is synchronized to both the heartbeat and passing blade. A finite-sized window of pulse phase is used to ensure that both these events occur during every cycle of the heartbeat in order to keep the data acquisition rate sufficiently high 共1 Hz兲 and to keep the laser running. By 260 / Vol. 127, APRIL 2005 With the exception of the inlet elbow at low flow rates and cutwater recirculation region at high flow rates, the pulsatility of the flow has a minimal effect on the flow field. In all regions that were investigated, the flow field during and immediately after sudden accelerations and decelerations was compared to a steady flow case at the same or a similar flow rate. Little difference was detected in either the mean flow or turbulent statistics, indicating that the quasi-steady assumption is valid in this pump. Differences between the steady and unsteady cases are most pronounced in the inlet region and the cutwater recirculation zone. This can be expected because these are both regions with large boundary layers, relatively low momentum 共due to slow speeds兲 and low effective viscosity 共due to low turbulence intensities兲. At a mean velocity of 1 m / s, fluid will travel ⬃300 mm during the time between 3 / 10 and 9 / 10. This is slightly greater than the length of the inlet cannula. If the fluctuations in flow that contribute to rms in the inlet elbow 共discussed elsewhere 关18兴兲 are the result of entrance effects from the ventricle into the inlet cannula, it follows that the fluctuations are not apparent in the inlet elbow until enough time has elapsed during systole that fluid has traveled from the entrance of the inlet cannula into the inlet elbow. This could explain the phase delay of the rms profile as compared to profiles of mean speed. Although measured velocity and shear fields were slightly different from the steady cases during the sudden accelerations and decelerations at the beginning and end of systole, they are essentially identical to the steady flow case during the high flow and low flow conditions that constitute the majority of the pulse cycle. This indicates that unsteady terms are not significant in the flow field, so that the quasi-steady assumption is valid at this pulse rate. It would be expected that unsteady terms become more significant at increased pulse rate and decreasingly important at slower pulse rates. Measurements and computations of the steady flow field at the corresponding flow rate are a good representation of the flow field at any phase of the heartbeat. The current study addresses the flow within a magnetically suspended VAD using a prototype with an impeller suspended on a shaft. The potential significance of this is that the shaft-mounted impeller is rigidly suspended, whereas the position of a magnetically suspended impeller is a function of the forces exerted on the impeller. During the pulse cycle, variations in the flow rate will affect the fluid forces exerted on the impeller and therefore the exact position of the impeller as controlled by the magnetic suspension. The precise effect that this variation on geometry would have on the time-varying flow field is not known. In the magnetically suspended prototypes of this pump variations in impeller position are never more than 0.10 mm over the range of flow rates presented here, which is rather small compared to a blade height of 2 mm and most characteristic dimensions of the pump. Transactions of the ASME Fig. 9 Profiles of mean velocity and MRSS at x = 0.02 m within the cut-water as a function of pulse phase „solid line… compared to contours for steady flow cases „dashed line… Measured viscous and Reynolds shear stress levels within this pump during time-varying flow are similar to those of steady flow conditions at the corresponding flow rate. Over the range of flow rates investigated here, and, therefore, the range of measured shear stresses, pump-induced hemolysis is not expected to be significant 关18兴. Stress levels at some flow rates do, however, exceed those reported to activate platelets and therefore have the potential to initiate thrombus formation 关18兴. The pulsatile nature of the flow with a native heart may prove to be beneficial because it increases blood washout by changing the flow patterns within the Journal of Biomechanical Engineering pump during every heartbeat. As an example, the recirculation regions that exist in the diffuser at high flow rates is not present at low flow rates. Fluid streamlines are directed toward the inner wall of the diffuser and create wall shear levels that act to wash this region during diastole. Similarly, the recirculation region that exists in the blade passage at low flow rates is not present for high flow rates and levels of viscous shear on the pressure side of the blade are in the range of 2 Pa, which is reportedly large enough to discourage thrombus formation 关29,30兴. APRIL 2005, Vol. 127 / 261 Fig. 10 Cut-water configuration for free-running and 2 phases of passing blade arrangements at steady flow rate of 6 L / min, 2100 rpm Implications for Pump Design. The fact that the internal fluid field varies during each heartbeat cannot be ignored when designing or testing LVAD devices. One proposed design strategy is as follows. Instead of considering the nominal operating condition as the time-averaged value of flow, two separate operating conditions should be designed for. These correspond to the high-flow 共systole兲 and low-flow 共diastole兲 conditions. During operation with a beating ventricle, the pump spends approximately 80% of the time operating at either of these operating conditions, whereas it spends less than 10% of its time operating at the flow rate corresponding to the time-averaged mean flow. Certain requirements to insure biocompatibility will apply to either one or both of these flow rates. In some ways, this is a more rigorous requirement for the flow within these pumps because it places requirements at more than one operating point. In other ways, it actually relaxes the design requirements because some specifications must be met at one, but not both, of the two flow rates. Levels of viscous and Reynolds shear stress must be kept below acceptable levels and exposure times for both design flow rates and, preferably, all flow rates between their design flow rates. The requirements of blood washing to clear areas of stagnant flow and potentially wash solid surfaces with minimal levels of viscous shear are not required at all times. The periodic 共once per heartbeat兲 clearing of these structures and washing of walls may be sufficient to prevent thrombosis in the pumps. Every area within the pump does not have to have ideal flow patterns at the same phase of the heartbeat, so long as the fluid is washed at least once per cycle. Examples in this pump are the washing of the cutwater recirculation region during the low-flow case and washing of the recirculation in the blade passage during the high-flow condition. While either of these flow rates would be unattractive operating points for steady flow, they complement one another during pulsatile flow through the pump. It is realized that the values of maximum and minimum flow rates will vary based on physiology, so it is not obvious that there are two clear choices for the values of flow rates that should be selected. Nonetheless, the pump must perform in a variety of situations, almost none of which are for the steady flow at 6 L / min. The quasi-steady assumption can greatly simplify the design process. Computational modeling and experimental testing at two steady flow rates is significantly simpler than modeling and measuring the true transient behavior within the pump. This treatment can only be justified based on measurements, such at those presented herein, that demonstrate that the quasi-steady assumption is valid for both the low-flow and high-flow conditions in this pump. Acknowledgments Financial support for this work has been provided by the Utah Artificial Heart Institute and the Department of Health and Human Services, National Institute of Health, National Heart, Lung, and Blood Institute Grant No. R01 HL64378-01. MedQuest® Products, Inc., supplied substantial assistance with the fabrication of the prototype pump. The authors would also like to thank F. Scarano and M. L. Reithmuller for use of their PIV algorithm. Detailed comments and suggestions from the two anonymous reviewers were very helpful in preparing the final version of the manuscript. Nomenclature ␦ ⫽ boundary layer displacement thickness MRSS ũ ṽ U u u⬘ ublade upulse Fig. 11 Comparison of flow at 12 / 10 in the blade passage to steady flow at the same flow rate, 6 L / min 262 / Vol. 127, APRIL 2005 ⌽blade ⌽pulse ⫽ ⫽ ⫽ ⫽ ⫽ ⫽ ⫽ ⫽ ⫽ ⫽ kinematic fluid viscosity effective turbulent viscosity angular frequency of oscillation major Reynolds shear stress instantaneous velocity in the x-coordinate direction instantaneous velocity in the v-coordinate direction time averaged-mean velocity fluctuating component of velocity rms fluctuating velocity, u fluctuating component of velocity caused by blade passage ⫽ fluctuating component of velocity caused by heart pulse ⫽ phase of blade passage ⫽ phase of heart pulse Transactions of the ASME References 关1兴 Araki, K., Taenaka, Y., Masuzawa, T.,Inoue, K., Nakatani, T., Kinoshota, M., Akagi, H., Baba, Y., Sakaki, M., Anai, H., and Takano, H., 1993, “A Flow visualization Study of Centrifugal Blood Pumps Developed for Long-Term Usage,” Artif. Organs 17共5兲, pp. 307–312. 关2兴 Ng, B. T. H., Chan, W. K., Yu, S. C. M., and Li, H. D., 2000, “Experimental and Computational Studies of the Relative Flow Field in a Centrifugal Blood Pump,” Crit. Rev. Biomed. Eng. 28共1-2兲, pp. 119–125. 关3兴 Rose, M. L. J., Mackay, T. G., and Wheatley, D. J., 2000, “Evaluation of Four Blood Pump Geometries: Fluorescent Particle Flow Visualisation Technique,” Med. Eng. Phys. 22共3兲, pp. 201–214. 关4兴 Apel, J., Neudel, F., and Reul, H., 2001, “Computational Fluid Dynamics and Experimental Validation of a Microaxial Blood Pump,” ASAIO J. 47, pp. 552–558. 关5兴 Asztalos, B., Yamane, T., and Nishida, M., 1999, “Flow Visualization Analysis for Evaluation of Shear and Recirculation in a New Closed-Type, Monopivot Centrifugal Pump,” Artif. Organs 23共10兲, pp. 939–946. 关6兴 Baldwin, J., Tarbell, J., Deutsch, S., and Geselowitz, D., 1989, “Mean Flow Velocity Patterns Within a Ventricular Assist Device,” ASAIO Trans. 35共3兲, pp. 429–433. 关7兴 Nishida, M., Yamane, T., Tsukamoto, Y., Konishi, Y., Ito, K., Masuzawa, T., Tsukiya, T., and Taenaka, Y., 2000, “Effect of Washout Hole Geometry on a Centrifugal Blood Pump,” ASAIO J. 46共2兲, pp. 172–178. 关8兴 Day, S. W., McDaniel, J. C., Wood, H. G., Allaire, P. E., Landrot, N., and Curtas, A., 2001, “Particle Image Velocimetry Measurements of Blood Velocity in a Continuous Flow Ventricular Assist Device,” ASAIO J. 47共4兲, pp. 406–411. 关9兴 Tsukiya, T., Taenaka, Y., Tatsumi, E., and Takano, H., 2002, “Visualization Study of the Transient Flow in the Centirfugal Blood Pump Impeller,” ASAIO J. 48, pp. 431–436. 关10兴 Wu, Z. J., Antaki, J. F., Burgreen, G. W., Butler, K. C., Thomas, D. C., and Griffith, B. P., 1999, “Fluid Dynamic Characterization of Operating Conditions for Continuous Flow Blood Pumps,” ASAIO J. 45, pp. 442–449. 关11兴 Manning, K. B., and Miller, G. E., 2002, “Flow Through an Outlet Cannula of a Rotary Ventricular Assist Device,” Artif. Organs 26共8兲, pp. 714–723. 关12兴 Orime, Y., Takatani, S., Tasai, K., Ohara, Y., Naito, K., Mizugugchi, K., Meier, D., Wernicke, J. T., Dann, G., Glueck, J., Noon, G. P., and Nose, Y., 1994, “The Baylor Total Artificial Heart,” ASAIO J. 40, pp. M499–M505. 关13兴 Baldwin, J. T., Deutsch, S., Geselowitz, D. B., and Tarbell, J. M., 1994, “LDA Measurements of Mean Velocity and Reynolds Stress-Fields Within an Artificial-Heart Ventricle,” ASME J. Biomech. Eng. 116共2兲, pp. 190–200. 关14兴 Maymir, J. C., Deutsch, S., Meyer, R. S., Geselowitz, D. B., and Tarbell, J. M., 1998, “Mean Velocity and Reynolds Stress Measurements in the Regurgitant Jets of Tilting Disk Heart Valves in an Artificial Heart Environment,” Ann. Biomed. Eng. 26共1兲, pp. 146–156. 关15兴 Mussivand, T. D., and Naber, B. K. D., 1999, “Fluid Dynamic Optimization of Journal of Biomechanical Engineering 关16兴 关17兴 关18兴 关19兴 关20兴 关21兴 关22兴 关23兴 关24兴 关25兴 关26兴 关27兴 关28兴 关29兴 关30兴 a Ventricular Assist Device Using Particle Image Velocimetry,” ASAIO J. 45共1兲, pp. 25–31. Wernert, P., and Favier, D., 1999, “Considerations About the Phase Averaging Method With Application to LDV and PIV Measurements Over Pitching Airfoils,” Exp. Fluids 27共6兲, pp. 473–83. Zhang, Z., Eisele, K., and Hirt, F., 1997, “The Influence of Phase-Averaging Window Size on the Determination of Turbulence Quantities in Unsteady Turbulent flows,” Exp. Fluids 22, pp. 265–267. Day, S. W., and McDaniel, J. C., “PIV Measurements of Flow in a Centrifugal Blood Pump: Steady Flow,” ASME J. Biomech. Eng. 共in press兲. Adrian, R. J., 1991, “Particle Imaging Techniques for Fluid Mechanics,” Annu. Rev. Fluid Mech. 23, pp. 261–304. Scarano, F., and Reithmuller, M., 1999, “Iterative Multigrid Approach in PIV Image Processing With Discrete Window Offset,” Exp. Fluids 26, pp. 513– 523. Day, S. W., McDaniel, J. C., Wood, H. G., Allaire, P. E., Song, X., Lemire, P. P., and Miles, S. D., 2002, “A Prototype HeartQuest Ventricular Assist Device for Particle Image Velocimetry Measurements,” Artif. Organs 26共11兲, pp. 1002–1005. Mills, C. J., Gabe, I. T., Gault, J. H., Mason, D. T., Ross, J. J., Braunwald, E., and Shillingford, J. P., 1970, “Pressure-Flow Relationships and Vascular Impedance in Man,” Cardiovasc. Res. 4, pp. 405–417. McKay, R. G., Aroesty, J. M., Heller, G. V., Roayl, H., Parker, A., Silverman, K. J., Kolodny, G. M., and Grossman, W., 1984, “Left Ventricular PressureVolume Diagrams and End-Systolic Pressure-Volume Relations in Human Being,” J. Am. Coll. Cardiol. 3共2兲, pp. 301–312. Wernet, M. P., 2000, “Application of DPIV to study both steady state and transient turbomachinery flows,” Opt. Laser Technol. 32, pp. 497–525. Baldwin, J. T., Deutsch, S., Petrie, H. L., and Tarbell, J. M., 1993, “Determination of Principal Reynolds Stresses in Pulsatile Flows After Elliptical Filtering of Discrete Velocity Measurements,” ASME J. Biomech. Eng. 115共4兲, pp. 396–403. Sinha, M., Katz, J., and Meneveau, C., 1998, “Addressing Passage-Averaged and LES Modeling Issues in Turbomachinery Flows Using Two-Dimensional PIV Data,” Proc. ASME Fluids Engineering Division Summer Meeting, Washington, D.C., FEDSM98-5091. Stepanoff, A. J., 1957, Centrifugal and Axial Flow Pumps, Wiley, New York. Flack, R. D., Hamkins, C. P., and Brady, D. R., 1987, “Laser Velocimeter Turbulence Measurements in Shrouded and Unshrouded Radial Flow Pump Impellers,” Int. J. Heat Fluid Flow 8共1兲, pp. 16–25. Hashimoto, S., Maeda, H., and Sasada, T., 1985, “Effects of Shear Rate on Clot Growth at Foreign Surfaces,” Artif. Organs 9, pp. 345–350. Folie, B. J., and McIntire, L. V., 1989, “Mathematical Analysis of Mural Thrombogenesis. Concentration profiles of Platelet-Activating Agents and Effects of Viscous Shear Flow,” Biophys. J. 56, pp. 1121–1141. APRIL 2005, Vol. 127 / 263