Massachusetts General Hospital Collaborate to Extubate
advertisement

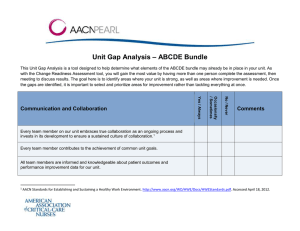
Place hospital logo here Massachusetts General Hospital (MGH) Collaborate to Extubate: A Needs Assessment and Educational Program on the ABCDEF Bundle Erica Edwards, RN, MSN, CCRN-CMC, CHFN Lisa O’Neill, RN, BSN Norine O’Malley-Simmler, RN, BSN Alicia Sheehan, RN, BSN Collaborate to Extubate Project Goal To assess intensive care nurses’ knowledge of the ABCDEF Bundle at MGH and provide education to address gaps in knowledge. What Is the ABCDEF Bundle? The ABCDEF bundle is a coordinated effort between multiple disciplines for the management of patients who are ventilated help prevent the unintended consequences of critical illness. The aim of using the bundle is to reduce oversedation, immobility and the development of delirium in patients who are ventilated thereby reducing ventilator days (VD) and length of stay (LOS). What Does ABCDEF Stand For? ABC–Awakening and Breathing Trial Coordination/ Collaboration Addresses daily Spontaneous Awakening Trials (SATs) (sedation vacation) and Spontaneous Breathing Trials (SBTs) to promote earlier extubation C also represents the Choice of sedation to be used D–Delirium Assessment and Management Addresses early identification and management of patients with delirium ABCDEF (continued) E–Early Exercise and Progressive Mobility Provides guidance for enabling patients to become progressively more active and, possibly, walk while intubated And… F–Family Involvement Involving the family in all aspects of the bundle to assist and support the patient Families Built on the work done in the MGH CICU around family presence during resuscitation and other procedures. Families provide active presence, serving as protectors, facilitators, and historians. They can act as coaches as patients are weaned from ventilators and help with early mobility.1-2 Significance: Scope of the Problem There were 790,257 hospitalizations involving mechanical ventilation in the U.S. in 2005. The estimated national cost was $27 billion, or 12% of all hospital costs. Mortality for patients who are mechanically ventilated is high. Quality improvement and cost reduction strategies are warranted when caring for these patients. Impact of Implementing Bundle on Health Care Decreased VD and LOS Implementing daily spontaneous awakening trials3 Ventilator days (VD)- ↓ 2.4 days Length of stay (LOS)- ↓ 3.5 days Using non-benzodiazepine vs benzodiazepine sedation4 VD ↓ 1.9 days LOS ↓ 1.62 days Impact of implementing bundle on healthcare – decreased ventilator days Impact of Implementing and length of stay Bundle on Health Care Implementing daily spontaneous awakening trials:² Ventilator days - ↓on2.4 days 5 Early mobility of patients ventilators - ↓↓3.5 LOS inLOS the ICU 1.4days days Using LOS innon-Benzodiazepines the hospital ↓ 3.3 days vs. Benzodiazepines sedation³ 6 - ↓ 1.9 days Delirium Ventilator detection days and prevention LOS ↓ LOS 3.6 days - ↓ 1.62 days Decreased VD and LOS Incidence of delirium ↓ 1.6% 2 Rose, Louise; Maunder, Robert; Hunter, Jon, et al. Sleep, cognitive, and psychological morbidity following sedation protocol and daily sedative interruption vs. sedation protocol alone in critically ill, mechanically ventilated adults (SLEAP-SCP). CCM .2012: 40(12) p 1–328 ³Fraser, G.L., Devlin, J.W., Worby, C.P. et al. Benzodiazepine versus nonbenzodiazapine –based sedation for mechanically ventilated , critically ill adults: a systematic review and meta-analysis of randomized trials. CCM 2013; 41(9), p 30-8 Projected Cost Savings of Implementation of the ABCDEF Bundle Cost savings (from national averages)5,7-8 SATs VD 2.4 x $1,522 (1 VD) = $3,652 LOS 3.3 x $3,500 (1 ICU day) = $11,550 Early Mobility LOS in hospital = $18,544.80 in 1 month Delirium Incremental cost of total episode of care = $8,19959 Project Logo and Catch Phrase: “Collaborate to Extubate” Study Design Convenience sample of nurses working in all areas at MGH that have patients who are ventilated Survey design adapted from AACN Pearl: Implementing the ABCDE Bundle at the Bedside and unit gap analysis to assess: Communication and collaboration Sedation awakening/spontaneous breathing trial/coordination and choice of sedation Delirium Early exercise Family involvement Data Collection Procedure IRB approval per MGH policy Met with nurse directors and CNSs of ICUs for approval and permission to send survey to staff Survey sent via Qualtrics Emailed weekly survey reminders Used posters and offered candy in snowman-decorated boxes to remind staff to take survey Demographics N = 212 respondents How many years as a nurse? Mean = 14.4 + 11.34 Highest level of nursing education AD: 9%, BSN: 79.7%, MSN: 9.9%, Doctorate: 0.9% CCRN certification 17% (36 RNs) Demographics Which unit do you work on? Blake 12 ICU: 10.8% Burn ICU (Bigelow 13): 2.8% Cardiac ICU (Ellison 9): 14.6% Cardiac Surgical ICU (Blake 8): 5.7% Medical ICU (Blake 7): 15.6% Neuroscience ICU (Lunder 6): 18.4% PICU: 4.7% RACU (Bigleow 9): 8.5% Surgical ICU (Ellison 4): 17.5% Survey Results Communication and Collaboration10 Yes/ No/ Always Never Every nurse on our unit embraces true collaboration as an ongoing process and invests in its development to ensure a sustained culture of collaboration. 89.5% 10.5% Every nurse contributes to the achievement of common unit goals. 90.4% 9.6% All staff nurses are informed and knowledgeable about patient outcomes and performance improvement data for our unit. 81.9% 18.1% Survey Results Sedation Awakening Trial/ Spontaneous Breathing Trial/ Coordination and Choice of Sedation Our unit has a sedation and analgesia protocol in place. Yes/ No/ Always Never 72.2% 27.8% 91% 9% Our nurses currently perform Spontaneous Awakening Trials (SATs, aka “sedation vacations”) daily on all patients receiving sedation. 72.3% 27.7% We have a standardized protocol for performing SATs. 70.1% 29.9% The nurses routinely perform both a pain and sedation assessment on patients, using a validated tool. Survey Results Delirium Assessment and Management Yes/ No/ Always Never All patients are assessed daily for the presence of delirium. 69.5% 30.5% Our nurses use a validated tool to assess for the presence of delirium (CAM-ICU, ICDSC, pCAMICU). 46.9% 53.1% Our nurses have a standardized delirium management protocol. 24.5% 75.5% Delirium monitoring is included in our daily rounds for patients. 38.8% 61.2% Survey Results Early Exercise and Progressive Mobility Yes/ No/ Always Never Our nurses have a protocol for early exercise and progressive mobility for patients. 67.5% 32.5% Immobile patients on our unit receive passive range of motion regularly, if tolerated. 62.2% 37.8% Our nurses have the necessary support equipment to safely assist with patients’ increased mobility. 78.4% 21.6% Respiratory therapists and physical therapists are available to assist with implementing early exercise and progressive mobility protocols. 83% 17% 61.7% 38.3% Mobility is addressed during daily rounds. Survey Results Family Involvement Our nurses provide a family-centered philosophy of care that supports visitations. Yes/ No/ Always Never 99% 1% Families are encouraged to give their input and ask questions. 97.1% 2.9% Family support and participation in all aspects of patient care are encouraged. 88.7% 11.3% Our nurses recognize the importance of updating families daily regarding their loved one’s condition. 99.5% 0.5% Hospital Fiscal Savings VD and LOS Reduction in VD by 1.21% (50 days/quarter) Projected cost savings per quarter: $76,100 50 VD x $1,522 (average cost/VD)7 Projected annual savings = $305,600 $76,400 x 4 quarters No reduction in LOS Educational Intervention Live educational sessions on each unit, 1 on day shift and 1 during evening (with 2 repeated for a total of 20 live sessions) Assessed current practice with each unit’s specific patient population Celebrated practices that were already in place and educated staff on other parts of bundle HealthStream PowerPoint slides Education on best practices Education - Best Practices CAM-ICU and P-CAM ICU delirium assessment tools SAT/SBT and mobility protocols Delirium prevention strategies – “Give PEACE a Chance” Physiologic, Environmental, ADLs/Sleep, Communication, Education/Evaluation 11 Strategies to Enhance Participation Poster Distributed to All ICUs Future Directions Met with Dr. Perrin Cobb (Director of the Massachusetts General Hospital Critical Care Center and Vice Chair for Critical Care in the Department of Anesthesia, Critical Care and Pain Medicine) about CSI project. He recently presented the ABCDE bundle in a critical care grand rounds. MGH CSI Team has been invited to take part in hospital-wide implementation. Widespread use of CAM-ICU delirium assessment Mobility protocols Continued re-assessment of impact on LOS and VD Special Thanks AACN CSI Faculty: Dave Hanson, MSN, RN, CNS, NEA-BC Chief Nurse and Senior Vice President for Patient Care at MGH: Jeanette Ives Erickson, RN, DNP, FAAN MGH Coaches: Colleen K. Snydeman, RN, PhDc, NE-BC and Susan Stengrevics, RN, MSN, ACNS-BC, CCRN MGH Norman Knight Nursing Center for Clinical and Professional Development: Kathryn Larivee, RN, MSN MGH Yvonne Munn Center for Nursing Research: Dorothy Jones, EdD, FAAN; Mary Duffy, RN, PhD; Susan Lee, RN, PhD; and Jane Flanagan, PhD, ANP-BC References 1. Edwards EE, Despotopulos LD, Carroll DL. Changes in provider perceptions of family presence during resuscitation. Clin Nurse Spec. 2013;27(5):239-244. 2. Rukstele CD, Gagnon MM. Making strides in preventing ICU-acquired weakness: involving family in early progressive mobility. Crit Care Nurs Q. 2013;36(1):141-147. 3. Rose L, Maunder R, Hunter J, et al. Sleep, cognitive and psychological morbidity following sedation protocol and daily sedative interruption vs sedation protocol alone in critically ill, mechanically ventilated adults (SLEAP-SCP). Crit Care Med. 2012;40(12suppl 1):1-328. 4. Fraser GL, Devlin JW, Worby CP, et al. Benzodiazepine versus nonbenzodiazapine–based sedation for mechanically ventilated, critically ill adults: a systematic review and metaanalysis of randomized trials. Crit Care Med. 2013;41(9suppl1):S30-S38. 5. Morris PE, Goad A, Thompson C, et al. Early intensive care unit mobility therapy in the treatment of acute respiratory failure. Crit Care Med. 2008;36(8):2238-2243. 6. Allen KR, Fosnight SM, Wilford R, et al. Implementation of a system-wide quality improvement project to prevent delirium in hospitalized patients. Jclin Outcomes Manage. 2011;18(6):253-258. References 7. Dasta JF, McLaughlin TP, Mody SH, Piech CT. Daily cost of an intensive care unit day: the contribution of mechanical ventilation. Crit Care Med. 2005;33(6):1266-1271. 8. King L. Developing a progressive mobility activity protocol. Orthop Nurs. 2012;31(5):253262. 9. Research Triangle Institute for Center for Medicare & Medicaid Services. Analysis report: Estimating the incremental costs of hospital-acquired conditions (HACs). 2012. http://www.cms.gov/Medicare/Medicare-Fee-for-ServicePayment/HospitalAcqCond/index.html. Accessed April 1, 2014. (Click Incremental Updated Cost Report). 10. American Association of Critical-Care Nurses. AACN standards for establishing and sustaining healthy work environments: a journey to excellence. 2005. http://www.aacn.org/WD/HWE/Docs/HWEStandards.pdf. Accessed April 18, 2012. 11. Balas MC, Rice M, Chaperon C, Smith H, Disbot M, Fuchs B. Management of delirium in critically ill older adults. Crit Care Nurse. 2012;32(4):15-26.