Predictors of Sudden Cardiac Death and Appropriate Shock
in the Comparison of Medical Therapy, Pacing, and
Defibrillation in Heart Failure (COMPANION) Trial
Leslie A. Saxon, MD; Michael R. Bristow, MD; John Boehmer, MD; Steven Krueger, MD;
David A. Kass, MD; Teresa De Marco, MD; Peter Carson, MD; Lorenzo DiCarlo, MD;
Arthur M. Feldman, MD, PhD; Elizabeth Galle, MS; Fred Ecklund, MS
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
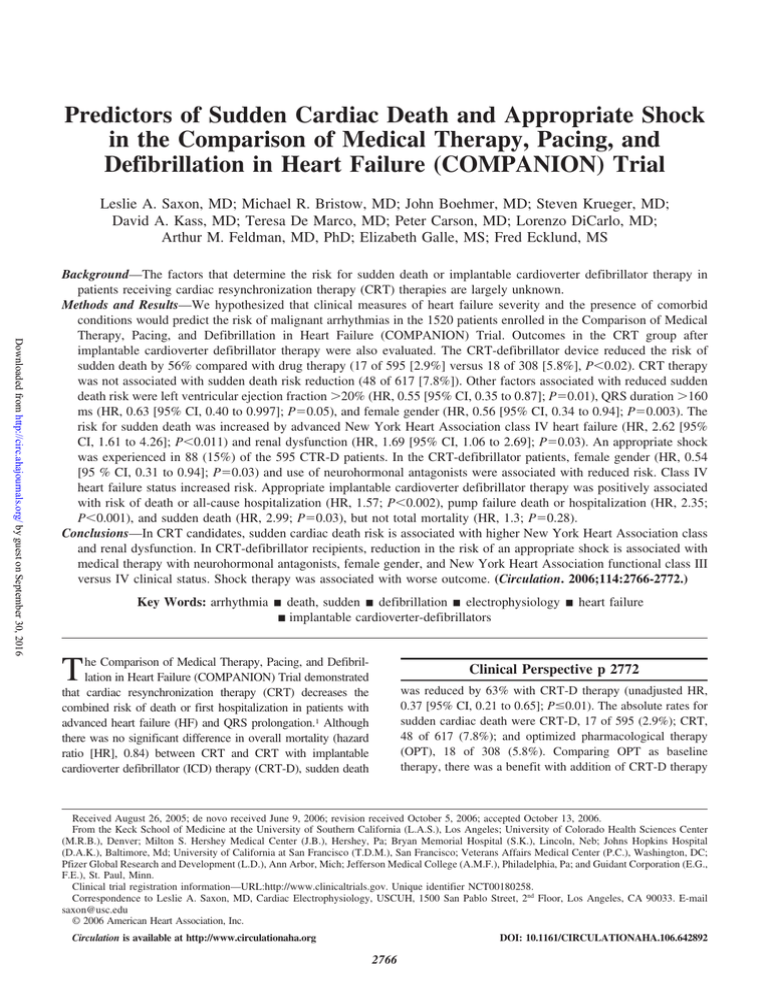
Background—The factors that determine the risk for sudden death or implantable cardioverter defibrillator therapy in
patients receiving cardiac resynchronization therapy (CRT) therapies are largely unknown.
Methods and Results—We hypothesized that clinical measures of heart failure severity and the presence of comorbid
conditions would predict the risk of malignant arrhythmias in the 1520 patients enrolled in the Comparison of Medical
Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Trial. Outcomes in the CRT group after
implantable cardioverter defibrillator therapy were also evaluated. The CRT-defibrillator device reduced the risk of
sudden death by 56% compared with drug therapy (17 of 595 [2.9%] versus 18 of 308 [5.8%], P⬍0.02). CRT therapy
was not associated with sudden death risk reduction (48 of 617 [7.8%]). Other factors associated with reduced sudden
death risk were left ventricular ejection fraction ⬎20% (HR, 0.55 [95% CI, 0.35 to 0.87]; P⫽0.01), QRS duration ⬎160
ms (HR, 0.63 [95% CI, 0.40 to 0.997]; P⫽0.05), and female gender (HR, 0.56 [95% CI, 0.34 to 0.94]; P⫽0.003). The
risk for sudden death was increased by advanced New York Heart Association class IV heart failure (HR, 2.62 [95%
CI, 1.61 to 4.26]; P⬍0.011) and renal dysfunction (HR, 1.69 [95% CI, 1.06 to 2.69]; P⫽0.03). An appropriate shock
was experienced in 88 (15%) of the 595 CTR-D patients. In the CRT-defibrillator patients, female gender (HR, 0.54
[95 % CI, 0.31 to 0.94]; P⫽0.03) and use of neurohormonal antagonists were associated with reduced risk. Class IV
heart failure status increased risk. Appropriate implantable cardioverter defibrillator therapy was positively associated
with risk of death or all-cause hospitalization (HR, 1.57; P⬍0.002), pump failure death or hospitalization (HR, 2.35;
P⬍0.001), and sudden death (HR, 2.99; P⫽0.03), but not total mortality (HR, 1.3; P⫽0.28).
Conclusions—In CRT candidates, sudden cardiac death risk is associated with higher New York Heart Association class
and renal dysfunction. In CRT-defibrillator recipients, reduction in the risk of an appropriate shock is associated with
medical therapy with neurohormonal antagonists, female gender, and New York Heart Association functional class III
versus IV clinical status. Shock therapy was associated with worse outcome. (Circulation. 2006;114:2766-2772.)
Key Words: arrhythmia 䡲 death, sudden 䡲 defibrillation 䡲 electrophysiology 䡲 heart failure
䡲 implantable cardioverter-defibrillators
T
he Comparison of Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Trial demonstrated
that cardiac resynchronization therapy (CRT) decreases the
combined risk of death or first hospitalization in patients with
advanced heart failure (HF) and QRS prolongation.1 Although
there was no significant difference in overall mortality (hazard
ratio [HR], 0.84) between CRT and CRT with implantable
cardioverter defibrillator (ICD) therapy (CRT-D), sudden death
Clinical Perspective p 2772
was reduced by 63% with CRT-D therapy (unadjusted HR,
0.37 [95% CI, 0.21 to 0.65]; Pⱕ0.01). The absolute rates for
sudden cardiac death were CRT-D, 17 of 595 (2.9%); CRT,
48 of 617 (7.8%); and optimized pharmacological therapy
(OPT), 18 of 308 (5.8%). Comparing OPT as baseline
therapy, there was a benefit with addition of CRT-D therapy
Received August 26, 2005; de novo received June 9, 2006; revision received October 5, 2006; accepted October 13, 2006.
From the Keck School of Medicine at the University of Southern California (L.A.S.), Los Angeles; University of Colorado Health Sciences Center
(M.R.B.), Denver; Milton S. Hershey Medical Center (J.B.), Hershey, Pa; Bryan Memorial Hospital (S.K.), Lincoln, Neb; Johns Hopkins Hospital
(D.A.K.), Baltimore, Md; University of California at San Francisco (T.D.M.), San Francisco; Veterans Affairs Medical Center (P.C.), Washington, DC;
Pfizer Global Research and Development (L.D.), Ann Arbor, Mich; Jefferson Medical College (A.M.F.), Philadelphia, Pa; and Guidant Corporation (E.G.,
F.E.), St. Paul, Minn.
Clinical trial registration information—URL:http://www.clinicaltrials.gov. Unique identifier NCT00180258.
Correspondence to Leslie A. Saxon, MD, Cardiac Electrophysiology, USCUH, 1500 San Pablo Street, 2nd Floor, Los Angeles, CA 90033. E-mail
saxon@usc.edu
© 2006 American Heart Association, Inc.
Circulation is available at http://www.circulationaha.org
DOI: 10.1161/CIRCULATIONAHA.106.642892
2766
Saxon et al
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
(unadjusted HR, 0.45 [95% CI, 0.23 to 0.86], P⫽0.02) but not
CRT therapy (unadjusted HR, 1.21 [95% CI, 0.70 to 2.08],
P⫽0.50).
There is very little available data that identify baseline
predictors for sudden death or that describe the time course to
appropriate ICD therapy in HF patients with ICD or CRT-D
devices implanted for primary prevention indications.2– 8
Factors influencing survival benefit or likelihood of ICD
therapy that have been identified include greater time duration after myocardial infarction, higher New York Heart
Association (NYHA) functional class, and lower left ventricular ejection fraction (LVEF).3–5 For primary prevention
CRT-D recipients, early studies with short durations of
follow-up did not show a reduction in device therapies for
ventricular tachycardia (VT) or ventricular fibrillation (VF)
for the first 6 months after implantation regardless of whether
CRT was programmed on or off.6 – 8 The influence of CRT
therapy on arrhythmia outcomes is also largely unknown for
CRT recipients without a history of symptomatic ventricular
arrhythmias. In 2 other controlled mortality trials that studied
patients treated only with CRT, 1 did not report mode of
death after 6 months of CRT and the other showed a 40%
reduction in sudden death risk when follow-up was extended
to 3 years after implant.9 –11
A post hoc analysis was performed based on the hypothesis
that both the severity of HF and presence of comorbidities
would predict a higher likelihood for sudden death and, in
ICD recipients, ventricular arrhythmias requiring
defibrillation.
The impact of ICD therapies on outcomes after CRT was
also assessed.
Methods
The trial design and results of the COMPANION Trial have been
reported elsewhere.1 The trial prospectively enrolled 1520 patients
with NYHA class III or IV HF due to ischemic or nonischemic
cardiomyopathy in association with a LVEF of ⱕ0.35 and a QRS
interval of ⱖ120 ms and were hospitalized for the treatment of HF
in the year before enrollment. No patient had a history of a
symptomatic ventricular arrhythmia. Patients were randomly assigned in a 1:2:2 ratio to protocol-mandated (OPT) alone or in
association with a CRT or CRT-D device. Pharmacological therapy
required maximally tolerated dosages of diuretics, angiotensinconverting enzyme inhibitors, -blockers, and spironolactone. The
primary composite end point risk of time to death or hospitalization
from any cause was reduced by 20% in both CRT and CRT-D arms
compared with pharmacological therapy. The relative risk of allcause mortality was reduced by 36% with the CRT-D device
(P⫽0.003) and 24% with CRT (P⫽0.06).
All 1520 study patients were included in the post hoc analysis of
baseline predictors of risk for sudden cardiac death, and all 595
CRT-D patients were included in the appropriate shock analysis.
Sudden cardiac death events were adjudicated by an end points
committee that determined mode of death according to published
definitions.2,5 In the 595 patients randomized to the CRT-D device,
appropriate device therapy consisting of an ICD shock was also
analyzed. Shocks were designated as appropriate after the implanting
physician reviewed the intracardiac electrograms stored from the
event and determined that a shock was delivered for VT/VF meeting
the programmed detection parameters.
A Cox proportional hazards multivariate regression model with
stepwise selection was used for time to sudden cardiac death and
appropriate shock analysis. Date of appropriate shock was determined according to the date the shock was reported. All HRs are
Sudden Death and Appropriate CRT Shock
2767
adjusted unless indicated (unadjusted). The following baseline variables were included in the stepwise selection: NYHA class (IV
versus III), LVEF (⬎20% versus ⱕ20%), -blocker, angiotensinconverting enzyme inhibitor, angiotensin receptor blocker, and
spironolactone use, QRS ⬎160 ms, left bundle-branch block, right
bundle-branch block, heart rate ⱕ72 bpm, ischemic etiology, female
gender, diabetes, age ⱕ65 years, body mass index, and the presence
of renal dysfunction. Variables remained in the model if they were
significant at 0.05 (entry criteria ⫽0.30). All analyses were based on
intent-to-treat. Based on the log(⫺log) plot, there was no evidence
that the proportional hazards assumption was violated for the sudden
cardiac death analysis by treatment. For the composite mortality and
hospitalization analysis, any hospitalization end point and associated
follow-up time prior to the shock are excluded in the “appropriate
shock” arm.
The number needed to treat is calculated at the median follow-up
time of 12 months for the mortality and hospitalization end points,
and 15 months for the mortality only end points. The needed to treat
calculation is the reciprocal of the absolute risk reduction multiplied
by 100. The absolute risk reduction is the difference between the
percent of patients who are end point–free at the median follow-up
time in the treatment arm and the same percentage in the OPT arm.
The resulting statistic is the number of patients who must be treated
for one person to benefit.12
The clinical characteristics reflective of HF severity and comorbidities used in this analysis to assess their relationship to risk are
provided in Table 1. There were no significant differences in any of
the prespecified variables according to treatment group.
The authors had full access to the data and take full responsibility
for the integrity of the data. All authors have read and agree to the
manuscript as written.
TABLE 1. Clinical Characteristics Evaluated for Risk of
Sudden Death and Appropriate ICD Shock
OPT
(n⫽308)
CRT
(n⫽617)
CRT-D
(n⫽595)
P
Value
Class III, %
82
87
86
0.11*
Class IV, %
18
13
14
23⫾7.2
22⫾6.8
23⫾6.9
0.20†
59
54
55
0.34*
Baseline Characteristic
NYHA heart failure class
LVEF measurement, %,
mean⫾SD
HF cause, %
Ischemic
41
46
45
Heart rate, bpm, mean⫾SD
Nonischemic
72⫾12
73⫾13
73⫾13
0.48†
Age, y, mean⫾SD
67⫾11
65⫾12
66⫾11
0.19
Gender, % female
31
33
33
0.92*
Body mass index, mean⫾SD
28⫾6.2
28⫾6.0
29⫾6.2
0.13
Diabetes status, %
45
39
41
0.23*
Renal dysfunction, %
23
22
23
0.95
-Blocker, %
66
68
68
0.85*
ACE inhibitor, %
69
70
69
0.94*
Angiotensin receptor blocker, %
23
22
23
0.98*
Spironolactone, %
55
53
55
0.80*
156⫾24
159⫾25
159⫾24
0.21†
0.22*
QRS duration, ms, mean⫾SD
Left bundle-branch block, %
70
69
73
Right bundle-branch block/IVCD, %
30
31
27
䡠䡠䡠
ACE indicates angiotensin-converting enzyme; IVCD, intraventricular conduction delay.
*P value based on 2 test. The contrasts pertain to differences between any of
the treatment groups.
†P value based on t test. The contrasts pertain to differences between any
of the treatment groups.
2768
Circulation
December 19/26, 2006
Results
Unanticipated Crossovers and Study Withdrawals
Implant success of the CRT system was achieved in 87% of
CRT and 91% of CRT-D patients. During the course of the
study, a total of 113 (37%) OPT-treated, 67 (11%) CRTtreated, and 17 (3%) CRT-D–treated patients crossed over
from their treatment arms to receive a commercially available
pacemaker, CRT, or CRT-D device for arrhythmia or HF
indications. In this group, there were a total of 3 sudden
deaths, 1 in each randomization arm. Before crossing over,
the majority of patients had reached a primary study end
point: 103 (91%) OPT patients, 53 (79%) CRT patients, and
6 (35%) CRT-D) patients.
Sudden Death
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Over a mean follow-up of 15.7 months, sudden death was
adjudicated as the cause of death in 18 of 308 (5.8%) patients
randomized to OPT, 48 of 617 (7.8%) patients who received
the CRT device, and 17 of 595 (2.9%) patients with the
CRT-D device. Compared with OPT, the CRT-D device was
associated with a 55% reduction in sudden death risk (HR,
0.45; P⫽0.02). Table 2 lists the HRs for those variables
associated with either a reduction or increased risk of sudden
death. These are based on 83 sudden deaths occurring in 1519
patients. Along with CRT-D therapy, LVEF ⬎20%, QRS
duration at baseline ⬎160 ms, and female gender were
associated with reduced risk. Conversely, class IV versus
class III HF was associated with more than twice the risk of
sudden death. Likewise, the presence of renal dysfunction
increased sudden death risk.
Appropriate Shock
ICD therapy of a first shock was delivered in 142 of 595
patients (24%). Of these, 88 (61%) were considered appropriate for sensed VT or VF and 54 (38%) were classified as
inappropriate because of either supraventricular tachycardia
(42 events), oversensing (10 events), or unclassified reasons
(2 events). The time to device shock is shown in Figure 1 and
illustrates that nearly 1 in 5 patients randomized to CRT-D
therapy experience an appropriate device shock by the second
year after implant.
Table 3 displays the odds ratios for those factors associated
with the risk of receiving an appropriate shock. Therapy with
the neurohormonal antagonists including -blockers, angiotensin-converting enzyme, angiotensin receptor blocker
TABLE 2.
Figure 1. Risk of appropriate shock in CRT-D recipients.
agents, and female gender reduced the risk of a shock. Class
IV versus class III HF status increased risk.
Impact of ICD Shocks on Outcome
Unadjusted risk of death or first all-cause hospitalization
(Figure 2A; HR, 1.6; P⬍0.009), pump failure death or
hospitalization (Figure 2B; HR, 2.4; P⫽0.001), sudden death
mortality (Figure 2C; HR, 3.0; P⫽0.03), and total mortality
(Figure 2D; HR, 1.7; P⫽0.03) were increased by the need for
an appropriate shock. After adjusting for the prespecified
variables, including class IV HF and LVEF, mortality was the
only end point not increased by shock therapy (HR, 1.3;
P⫽0.28).
Number Needed to Treat to Prevent Sudden Death
Table 4 provides data on the number of patients needed to
treat to prevent 1 patient from reaching the COMPANION
primary and secondary (mortality) study end points as well as
HF death, hospitalization, and sudden cardiac death. For
sudden death prevention, 25 patients would need to receive a
CRT-D device for 1 patient to receive survival benefit from
sudden death over a 15-month period after device implant.
The numbers needed to treat are significantly reduced when
TABLE 3.
Risk of Sudden Cardiac Death
Risk of Appropriate Shock Analysis
Appropriate Shock, CRT-D Only
(n⫽87/595)
Sudden Cardiac Death (n⫽83/1519)
Variable
Hazard Ratio
CRT-D
0.47
P Value
0.02
(0.24 to 0.91)
95% CI
CRT
1.21
0.48
(0.71 to 2.09)
LVEF ⬎20%
0.55
0.01
(0.35 to 0.87)
QRS ⬎160 ms
0.63
0.05
(0.40 to 0.997)
Female gender
0.47
⬍0.01
(0.27 to 0.82)
NYHA class IV
2.62
⬍0.01
(1.61 to 4.26)
Renal dysfunction
1.69
0.03
(1.06 to 2.69)
Variable
Hazard Ratio*
P Value
95% CI
-Blocker use
0.63
0.04
(0.41 to 0.97)
ACE inhibitor use
0.44
⬍0.01
(0.26 to 0.75)
Angiotensin receptor blocker use
0.53
0.05
(0.28 to 0.996)
Female
0.56
0.03
(0.34 to 0.94)
HF functional class IV
1.73
0.04
(1.02 to 2.93)
ACE indicates angiotensin-converting enzyme.
*Odds ratio for appropriate shock vs no shock/inappropriate only shock.
Saxon et al
Sudden Death and Appropriate CRT Shock
2769
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Figure 2. Unadjusted Kaplan-Meier survival curves after appropriate shock: A, All-cause mortality and first hospitalization; B, pump failure death and heart failure hospitalization; C, sudden cardiac death; D, all-cause mortality. Adjusted values are also provided.
evaluating the primary, secondary, and HF composite end
points.
Discussion
Sudden Death Risk
The present study demonstrates that cardiac resynchronization therapy combined with an ICD favorably impacts sudden
death risk. Although the COMPANION Trial was not designed to compare CRT therapy with CRT-D therapy, the
findings of the present study demonstrate a positive therapeutic association with CRT-D but not CRT therapy with regard
to sudden death risk reduction.1,2
In the Cardiac Resynchronization-Heart Failure (CAREHF) study of 813 patients, which compared medical therapy
to a CRT device alone, total mortality was reduced by 36% at
29 months with a CRT device10 (P⬍0.002). When follow-up
was extended to 36 months, risk of death due to HF
(P⫽0.003) and sudden death (P⫽0.006) were both reduced.10,11 Although sudden death risk was decreased in
CARE-HF with CRT alone, it required 36 months of follow-up
to demonstrate, and sudden death still accounted for 32% of all
deaths in CRT-treated patients. In COMPANION, sudden
death accounted for 28% of OPT deaths, 37% of CRT deaths,
and 17% of deaths in CRT-D treated patients.
These data from CARE-HF and COMPANION suggest
that when HF is advanced enough to merit CRT therapy,
CRT-mediated improvement in HF status is an appropriate
therapeutic target for sudden death prevention in many but
not all subjects. CRT-associated improvements in HF severity
may indirectly result in fewer sudden deaths as a result of
reductions in potentially proarrhythmic electrolyte shifts,
HF-induced worsening of cardiac ischemia, or proarrhythmic
neurohormonal activation.3,13 The finding that QRS duration
⬎160 ms reduced sudden death risk may suggest that these
subjects, by virtue of having more QRS delay, received
greater benefit from CRT and sudden death risk were related
to improved HF status.14 Conversely, subjects with longer
QRS duration may be at greater risk of HF progression, even
with CRT. Time-dependent prevention of, or reversal of,
structural and electrical remodeling may also lessen the risk
of malignant arrhythmia.15–17 There does not appear to be a
direct beneficial effect of CRT on the arrhythmia substrate
early after implantation of a CRT device. In a retrospective
analysis of data from the Multicenter InSync ICD Randomized Clinical Evaluation (MIRACLE ICD) trial of CRT-D
therapy in patients with primary and secondary ICD indications, there was no difference in ICD VT or VF detections
between patients randomized to CRT therapy on or CRT
therapy off in the first 6 months after device implantation.6
Our finding that LVEF ⬎20% reduced sudden death risk
and that class IV HF increased risk is consistent with
observations that, although HF is the predominant mode of
cardiovascular death in the setting of more advanced HF, the
absolute risk of sudden death increases with disease
severity.2,18
2770
Circulation
TABLE 4.
December 19/26, 2006
Number Needed to Treat in the COMPANION Population
OPT (% With
Event)
TRT (% With
Event)
NNT*
95%
CI
CRT-D vs OPT
67
56
9
8 to 10
CRT vs OPT
67
56
9
8 to 11
CRT-D vs OPT
25
15
10
8 to 13
CRT vs OPT
25
19
17
12 to 24
CRT-D vs OPT
29
45
6
6 to 8
CRT vs OPT
30
45
7
7 to 9
CRT-D vs OPT
6
2
25
16 to 39
CRT vs OPT
6
8
䡠䡠䡠
䡠䡠䡠
Outcome (Median Follow-Up Time)
Mortality or all-cause hospitalization (12 months)
Mortality (15 months)
Mortality or HF hospitalization (12 months)
Sudden death (15 months)
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
TRT indicates treatment arm; NNT, number needed to treat.
*NNT is the number of patients who must be treated for 1 person to benefit.
ICD Therapy in CRT-Treated Patients: A Marker
of Disease Severity?
The percentage of CRT-D–treated patients who experienced
appropriate ICD shocks in COMPANION and had class III or
IV HF is twice that reported for primary prevention right
ventricular ICD-treated patients with predominantly class II
HF.19,20 Our observation that the risk of shock exceeds the
risk of sudden death in OPT-treated patients implies that not
all shocks will result in a fatal event. Nonetheless, even if the
sustained ventricular arrhythmia would have terminated
spontaneously prior to shock therapy, it is reasonable to
assume that it may have introduced morbidity such as
syncope or worsening of HF.
In the second Multicenter Automatic Defibrillator Implantation Trial (MADIT-II) of ICD therapy in postinfarction
patients with left ventricular dysfunction, women had less
ICD therapy for VF but equivalent VT therapies and mortality benefit.21 The total number of women enrolled in both
COMPANION and MADIT-II may be too few to make any
firm conclusions, but the COMPANION data also show that
women benefit similarly for the primary end point analysis
but receive less ICD therapy for VT or VF.1
Perhaps the most provocative and concerning finding of
the COMPANION ICD therapy data is that the need for ICD
therapy in CRT-treated patients predicts a number of major
adverse outcomes, including risk of subsequent sudden death.
The finding of a protective effect of the neurohormonal
antagonists such as -blockers, angiotensin-converting enzyme, and angiotensin receptor blocker inhibitors on the risk
of ICD shock but not necessarily sudden death is not
surprising, as therapy with these agents was protocolmandated and sudden deaths are not always necessarily due
to arrhythmias. Although prior COMPANION analysis did
show that CRT-D mortality benefit was due to a reduction in
sudden death, not all ICD shocks will prevent sudden death,
particularly if it results from nontachyarrhythmic mechanisms such as pulmonary or systemic embolization or
electrical-mechanical dissociation.13 The onset of a sustained
ventricular arrhythmia in this patient population may repre-
sent a marker of worsening disease status. HF symptom
severity was linked to ICD shock rate in a prospective study
that evaluated the incidence and factors associated with right
ventricular ICD therapy in a mixed group of ICD recipients.
The risk of a device therapy increased 2-fold for patients with
class III HF symptoms compared with class I or II.5 This
interrelationship between HF severity and sudden death risk
was observed to be bidirectional in the primary prevention
MADIT II ICD trial. In patients that experienced appropriate
ICD shock therapies, the risk of a HF exacerbation was nearly
doubled over the next year.4 At the very least, an appropriate
ICD shock in our CRT-D treated patients interrupted a
sustained arrhythmia that may have introduced morbidity in
terms of worsening symptoms, prevention of syncope, injury,
or death. Yet our data also indicate that overall risk does not
end after appropriate and effective therapy delivery. In fact,
the increased subsequent risks of HF hospitalizations and
death suggest these HF patients may benefit from closer
clinical surveillance or additional adjunctive therapies to help
to further mitigate these risks.
Of clinical importance, the number needed to treat analysis
favors the placement of the ICD with CRT therapy in
COMPANION patients. This is supported by a similar
analysis performed for the RV ICD for primary prevention of
sudden death that defined a number needed to treat threshold
for a clinically meaningful survival benefit with ICD therapy
of 50 patients to prevent 1 death of any cause.22 That analysis
assumed a sudden death risk of 3% per year, much lower
than the 5.8% death risk observed in the medically treated
COMPANION arm.
Study Limitations
Although study hypotheses were determined before data
analysis, this was a post hoc analysis of COMPANION data.
Appropriate ICD shock is not a surrogate for mortality, as
sustained VT/VF may terminate spontaneously before shock
delivery or may occur in conjunction with a terminal event
such as fatal pulmonary embolism. Conclusions derived from
the composite mortality and hospitalization end points must
Saxon et al
be considered with caution, as all follow-up times and events
prior to appropriate shock were excluded from the “Appropriate Shock” arm, making the reasons for any differences in
arms challenging to isolate. ICD electrograms were not
available for central adjudication of appropriate or inappropriate shocks; such adjudication occurred at the implant
centers. Detection and ICD therapy programming was not
mandated. This limited our analysis of the prognostic importance of shocks for VT versus VF. The presence of renal
dysfunction was not rigorously defined in the COMPANION
protocol, limiting interpretation of risk-associated sudden
death. Previous studies have linked arrhythmia risk to chronic
renal dysfunction in populations with and without ICDs.
Chronic renal dysfunction is associated with a heightened
susceptibility to sudden death and elevated defibrillation
thresholds.23,24
Conclusions
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
In CRT candidates, sudden cardiac death risk is associated
with higher NYHA class and renal dysfunction. In primary
prevention CRT-D recipients, reduction in the risk of an
appropriate shock is associated with medical therapy with
neurohormonal antagonists and female gender, whereas
NYHA functional class IV clinical status increased risk.
Compared with the risks in patients not experiencing ICD
shocks, shock therapy is associated with increased risk of
hospitalization and death from both sudden and pump-failure
causes.
Sources of Funding
This study was supported by Guidant, a Boston Scientific company.
Disclosures
Dr Saxon has received honoraria from, served as a consultant to and
on the advisory board for, and received a research grant for work on
MADIT-CRT and CONTAK Renewal 3 AVT from Guidant Corporation. Dr Saxon has also received honoraria, grants, and consulting
fees from Medtronic. Dr Bristow has served as a consultant and on
the advisory board for Guidant Corporation. Dr Boehmer has
received research grants from Guidant Corporation and Medtronic,
Inc, and honoraria from Guidant Corporation and has served as a
consultant on the Guidant Heart Failure Advisory Board. Dr Kass
has received honoraria from, served as a consultant to, and served on
the Heart Failure, Neurostimulation, and Biologicals advisory boards
of Guidant Corporation. He has also received research grants for
work on BICAF, CRT in Patients, and Molecular Signaling in Mice.
Drs De Marco, Carson, and Feldman have served as consultants and
on the Advisory Board for Guidant Corporation. Dr DiCarlo is the
Senior Director of Cardiovascular Development, Pfizer Global Research and Development, with ownership interest in Pfizer, Inc. E.
Galle and F. Ecklund have ownership interest in Guidant Corporation. Dr Krueger reports no conflcts.
References
1. Bristow MR, Saxon LA, Boehmer J, Krueger S, Kass DA, De Marco T,
Carson P, DiCarlo L, DeMets D, White BG, DeVries DW, Feldman AM;
Comparison of Medical Therapy, Pacing, and Defibrillation in Heart
Failure (COMPANION) Investigators. Cardiac-resynchronization therapy
with or without an implantable defibrillator in advanced chronic heart
failure. N Engl J Med. 2004;350:2140 –2150.
2. Carson P, Anand I, O’Connor C, Jaski B, Steinberg J, Lwin A, Lindenfeld
J, Ghali J, Barnet JH, Feldman AM, Bristow MR. Mode of death in
advanced heart failure: the Comparison of Medical, Pacing, and Defibrillation Therapies in Heart Failure (COMPANION) trial. J Am Coll
Cardiol. 2005;46:2329 –2334.
Sudden Death and Appropriate CRT Shock
2771
3. Wilber DJ, Zareba W, Hall WJ, Brown MW, Lin AC, Andrews ML,
Burke M, Moss AJ. Time dependence of mortality risk and defibrillator
benefit after myocardial infarction. Circulation. 2004;109:1082–1084.
4. Moss AJ, Greenberg H, Case RB, Zareba W, Hall WJ, Brown MW,
Daubert JP, McNitt S, Andrews ML, Elkin AD; Multicenter Automatic
Defibrillator Implantation Trial-II (MADIT-II) Research Group.
Long-term clinical course of patients after termination of ventricular
tachyarrhythmia by an implanted defibrillator. Circulation. 2004;110:
3760 –3765.
5. Whang W, Mittleman MA, Rich DQ, Wang PJ, Ruskin JN, Tofler GH,
Muller JE, Albert CM; TOVA Investigators. Heart failure and the risk of
shocks in patients with implantable cardioverter defibrillators: results
from the Triggers Of Ventricular Arrhythmias (TOVA) study. Circulation. 2004;109:1386 –1391.
6. Wilkoff BL, Hess M, Young J, Abraham WT. Differences in
tachyarrhythmia detection and implantable cardioverter defibrillator
therapy by primary or secondary prevention indication in cardiac resynchronization therapy patients. J Cardiovasc Electrophysiol. 2004;15:
1002–1009.
7. Higgins SL, Hummel JD, Niazi IK, Giudici MC, Worley SJ, Saxon LA,
Boehmer JP, Higginbotham MB, De Marco T, Foster E, Yong PG.
Cardiac resynchronization therapy for the treatment of heart failure in
patients with intraventricular conduction delay and malignant ventricular
tachyarrhythmias. J Am Coll Cardiol. 2003;42:1454 –1459.
8. Young JB, Abraham WT, Smith AL, Leon AR, Lieberman R, Wilkoff
BL, Canby RC, Schroeder JS, Liem D, Hall S, Wheelan K; for The
Multicenter Insync ICD Randomized Clinical Evaluation (MIRACLE
ICD) Trial Investigators. Combined cardiac resynchronization and
implantable cardioversion defibrillation in advanced chronic heart failure:
The MIRACLE ICD Trial. JAMA 2003;289:2685–2694.
9. Abraham WT, Fisher WG, Smith AL, Delurgio DB, Leon AR, Loh E,
Kocovic DZ, Packer M, Clavell AL, Hayes DL, Ellestad M, Trupp RJ,
Underwood J, Pickering F, Truex C, McAtee P, Messenger J; MIRACLE
Study Group. Multicenter InSync Randomized Clinical Evaluation.
Cardiac resynchronization in chronic heart failure. N Engl J Med. 2002;
346:1845–1853.
10. Cleland JG, Daubert JC, Erdmann E, Freemantle N, Gras D,
Kappenberger L, Tavazzi L. The Effect of Cardiac Resynchronization on
Morbidity and Mortality in Heart Failure. N Engl J Med. 2005;352:
1539 –1549.
11. Cleland JG. New Results from the CARE-HF Programme. European
Society of Cardiology Congress Reports. Available: www.escardio.org/
knowledge/congresses/CongressReports/clinical/2005/cleland.htm.
Accessed online April 18, 2006.
12. Altman DG. Confidence intervals for the number needed to treat. BMJ.
1998;317:1309 –1312.
13. Luu M, Stevenson WG, Stevenson LW, Baron K, Walden J. Diverse
mechanisms of unexpected cardiac arrest in advanced heart failure. Circulation. 1989;80:1675–1680.
14. Auricchio A, Stellbrink C, Butter C, Sack S, Vogt J, Misier AR, Bocker
D, Block M, Kirkels JH, Kramer A, Huvelle E; Pacing Therapies in
Congestive Heart Failure II Study Group; Guidant Heart Failure Research
Group. Clinical efficacy of cardiac resynchronization therapy using left
ventricular pacing in heart failure patients stratified by severity of ventricular conduction delay. J Am Coll Cardiol. 2003;42:2109 –2116.
15. Saxon LA, De Marco T, Schafer J, Chatterjee K, Kumar UN, Foster E;
VIGOR Congestive Heart Failure Investigators. Effects of long-term
biventricular stimulation for resynchronization on echocardiographic
measures of remodeling. Circulation. 2002;105:1304 –1310.
16. Sutton MG, Plappert T, Hilpisch KE, Abraham WT, Hayes DL, Chinchoy
E. Sustained reverse left ventricular structural remodeling with cardiac
resynchronization at one year is a function of etiology: quantitative
Doppler echocardiographic evidence from the Multicenter InSync Randomized Clinical Evaluation (MIRACLE). Circulation. 2006;113:
266 –272.
17. Spragg DD, Leclercq C, Loghmani M, Faris OP, Tunin RS, DiSilvestre
D, McVeigh ER, Tomaselli GF, Kass DA. Regional alterations in protein
expression in the dyssynchronous failing heart. Circulation. 2003;108:
929 –932.
18. MERIT HF Study Group. Effect of Metoprolol CR/XL in chronic heart
failure. Metoprolol CR/XL randomized intervention trial in congestive
heart failure (MERIT-HF). Lancet 1999;353:2001–2007.
19. Kadish A, Dyer A, Daubert JP, Quigg R, Estes NA, Anderson KP,
Calkins H, Hoch D, Goldberger J, Shalaby A, Sanders WE, Schaechter A,
Levine JH; Defibrillators in Non-Ischemic Cardiomyopathy Treatment
2772
Circulation
December 19/26, 2006
Evaluation (DEFINITE) Investigators. Prophylactic defibrillator implantation in patients with nonischemic dilated cardiomyopathy. N Engl
J Med. 2004;350:2151–2158.
20. Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R,
Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, ClappChanning N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip
JH; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005;352:225–237.
21. Zareba W, Moss AJ, Jackson Hall W, Wilber DJ, Ruskin JN, McNitt S,
Brown M, Wang H; MADIT II Investigators. Clinical course and
implantable cardioverter defibrillator therapy in postinfarction women
with severe left ventricular dysfunction. J Cardiovasc Electrophysiol.
2005;16:1265–1270.
22. Jolly S, Dorian P, Alter DA. The impact of implantable cardiac defibrillators for primary prophylaxis in the community: baseline risk and clinically meaningful benefits. J Eval Clin Pract. 2006;12:190 –195.
23. Foley RN, Parfrey PS, Sarnak MJ. Clinical epidemiology of cardiovascular disease in chronic renal disease. Am J Kidney Dis. 1998;32:
S112–S119.
24. Wase A, Basit A, Nazir R, Jamal A, Shah S, Khan T, Mohiuddin I, White
C, Saklayen M, McCullough PA. Impact of chronic kidney disease upon
survival among implantable cardioverter-defibrillator recipients. J Interv
Card Electrophysiol. 2004;11:199 –204.
CLINICAL PERSPECTIVE
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
The vast majority of implantable cardioverter defibrillators (ICDs) are implanted for primary prevention of sudden death.
Cardiac resynchronization therapy (CRT) in conjunction with an ICD represents nearly one third of all ICDs implanted in
the United States and offers the potential benefit of improving HF for patients with class III or IV symptoms and ventricular
dysschrony. Although CRT can be implemented with pacing, without defibrillation, 90% of patients receive CRTdefibrillator. The predictors of sudden death and appropriate shock in the COMPANION Trial evaluates sudden death and
appropriate shock outcomes in patients treated with CRT devices versus medical therapy. Sudden death risk paralleled HF
severity and was associated with class IV HF and renal dysfunction. Women and patients with better LVEFs were at lower
risk. Appropriate ICD shocks for ventricular arrhythmias occurred at a rate of 15% at 16 months, greater than in primary
prevention ICD studies without CRT, and much greater than the risk of sudden death without an ICD, which suggests that
not all appropriate shocks would have resulted in sudden death. Appropriate shocks are associated with worse subsequent
outcome, including the combined end point of all-cause hospitalization and mortality. These findings are both reassuring
and concerning when viewed in the context of our clinical practice. The CRT-defibrillator device reduces sudden death
compared with medical therapy, but ventricular arrhythmias are a marker for worse outcomes despite effective termination
by the device, which suggests that additional evaluation and therapies should be considered for these high-risk patients.
Predictors of Sudden Cardiac Death and Appropriate Shock in the Comparison of
Medical Therapy, Pacing, and Defibrillation in Heart Failure (COMPANION) Trial
Leslie A. Saxon, Michael R. Bristow, John Boehmer, Steven Krueger, David A. Kass, Teresa
De Marco, Peter Carson, Lorenzo DiCarlo, Arthur M. Feldman, Elizabeth Galle and Fred
Ecklund
Downloaded from http://circ.ahajournals.org/ by guest on September 30, 2016
Circulation. 2006;114:2766-2772; originally published online December 11, 2006;
doi: 10.1161/CIRCULATIONAHA.106.642892
Circulation is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 2006 American Heart Association, Inc. All rights reserved.
Print ISSN: 0009-7322. Online ISSN: 1524-4539
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://circ.ahajournals.org/content/114/25/2766
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Circulation can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial
Office. Once the online version of the published article for which permission is being requested is located,
click Request Permissions in the middle column of the Web page under Services. Further information about
this process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Circulation is online at:
http://circ.ahajournals.org//subscriptions/