Curriculum Development in Medical Education
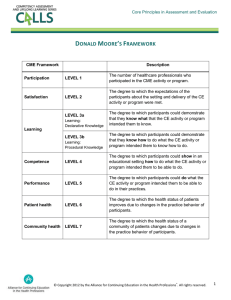
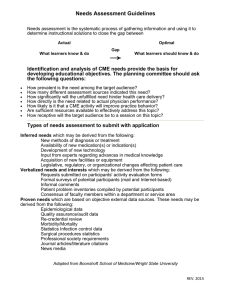
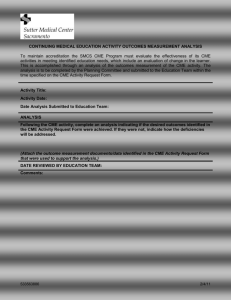
advertisement

Curriculum Development in Medical Education: Planning a CME Activity Richard F. Tischler, Jr., PhD, FACEHP Executive Director, CME University of Maryland School of Medicine Curriculum Development Models • Many models in existence • Today’s discussion will focus on the model reflected in the regulations of the Accreditation Council for Continuing Medical Education (ACCME) • That model was used to plan and develop this presentation Professional Practice Gap Many CME activities are planned and implemented without a clear curriculum model for learner‐ centered education. In addition, course directors sometimes do not implement required regulatory guidelines into their activity planning. As a result, their activities are less effective in achieving practice change and in complying with regulatory requirements. Optimal practice would include the planning and implementation of learner‐centered, compliant, effective CME activities. Can a 45‐minute presentation help address this practice gap? Can a 45‐minute presentation help address this practice gap? Yes! Target Audience • CME activity Course Directors • CME activity Planning Committee members • CME activity faculty members Educational Needs • Lack knowledge of the required curriculum model • Lack awareness of regulatory requirements in curriculum and content planning • Lack complete knowledge of CME industry “best practices” • Lack a complete set of strategies for implementation of models, regulatory requirements, and best practices in proposed activities Learning Objectives At the conclusion of this presentation, participants should be able to: • Describe a curriculum planning model • Complete required CME Application and Planning Documents • Define relevant, selected regulatory requirements for planning certified CME activities • Implement best practices and strategies for a successful CME activity Desired Result Participants will be able to implement strategies for designing a successful CME activity, including: – Documenting their implementation of the required curriculum model – Choosing appropriate faculty members – Developing, reviewing, and presenting CME content that is learner‐centered, compliant, and effective in changing practice Evaluation of Effectiveness • • • • • Quality of CME documentation Regulatory compliance Quality of the presentations Review of participant feedback Course director follow‐up A Curriculum Model for CME A Curriculum Model for CME A Curriculum Model for CME A Curriculum Model for CME A Curriculum Model for CME INEFFECTIVE What is the difference between current practice and optimal practice? Current Practice Optimal Practice The GAP Is CME the answer? What’s causing the gap? Current Practice Optimal Practice Institutional Barriers Financial Barriers Technology Politics What’s causing the gap? Current Practice Lack of: Awareness Knowledge Competence Performance Optimal Practice Educational Needs Current Practice Lack of: Awareness Knowledge Competence Performance Optimal Practice Educational Need Educational Intervention Target Audience Scope of Practice Target Audience Scope of Practice Target Audience Scope of Practice Target Audience Scope of Practice Target Audience Spectrum Generalist Resident Status Quo Specialist Experienced Practitioner Ready to change Target Audience Narrow Spectrum Generalist Resident Status Quo Specialist Experienced Practitioner Ready to change Target Audience Wide Spectrum Generalist Resident Status Quo Specialist Experienced Practitioner Ready to change Teacher‐Centered Model Student Student Teacher Student Learner‐Centered Education Expert Expert Learner Expert Keep the desired result in mind! Raise Awareness Increase Knowledge Improve Competence Improve Performance Improve Patient Health Writing the Learning Objectives What do you want the learners to do when they leave your activity? “Understand” Linking it Together Identified Practice Gap Educational Need of the Target Audience Learning Objective for the Educational Activity Desired Result (Measurable) Gap Need Result Objective Educational Formats and Methodologies What is the best way to achieve the desired results? Lecture with Q&A Case Presentations (with learner engagement) Simulated/Actual Patients Hands‐on Practice Multi‐media What is the rationale for the educational formats or methodologies you’ve chosen? Physician Attributes and Competencies Patient Care Medical Knowledge Practice Based Learning and Improvement Systems Based Practice Professionalism Interpersonal Skills and Communication Choosing Faculty Members A …zzzzz ? B Desirable Faculty Member Characteristics Knowledgeable Skilled Presenter Learner‐centered Reliable and Punctual Financial Relationships Conflict of Interest National Faculty Education Initiative www.nfeinitiative.org “The ABCs of Accredited CME” www.abcsofcme.org American Academy of Dermatology Content Concerns Content Concerns Complexity Content Concerns Complexity Evidence‐based Content Concerns Complexity Evidence‐based Learner‐centered Content Concerns Complexity Evidence‐based Learner‐centered Clearly presented Patient Care Recommendations Logistics Faculty and Learner Travel Registration Room Setup and Lighting Audio/Visual Logistics Faculty and Learner Travel Registration Room Setup and Lighting Audio/Visual Logistics Faculty and Learner Travel Registration Room Setup and Lighting Audio/Visual Logistics Faculty and Learner Travel Registration Room Setup and Lighting Audio/Visual Evaluation of Effectiveness Thank you! 6‐8634 rtischler@som.umaryland.edu