Neointimal Formation After Endovascular Arterial Injury Is
Markedly Attenuated in db/db Mice
Kent Stephenson, James Tunstead, Aileen Tsai, Ronald Gordon, Scott Henderson, Hayes M. Dansky
Downloaded from http://atvb.ahajournals.org/ by guest on September 30, 2016
Objective—A diabetic mouse model of accelerated neointimal formation would be a useful tool to understand the increased
incidence of restenosis in patients with diabetes.
Methods and Results—Femoral artery endoluminal wire injury was performed in diabetic insulin 2 Akita (ins2Akita) and
leptin receptor db/db (leprdb/db) mutant mice. Neointima size in ins2Akita mouse arteries was unchanged compared with
nondiabetic wild-type littermates. Although Ki67 labeling demonstrated similar rates of replication in the neointima of
leprdb/db mouse arteries, neointimal formation in leprdb/db mice was surprisingly reduced by ⬇90% compared with
nondiabetic lepr⫹/⫹ mice. Four hours after arterial injury, medial smooth muscle cell death was diminished in leprdb/db
arteries, suggesting that the initial response to arterial injury was altered in leprdb/db mice.
Conclusions—These studies highlight a differential response to arterial injury in leprdb/db mice and suggest a potential role
for leptin in the regulation of neointimal formation in response to arterial injury. (Arterioscler Thromb Vasc Biol. 2003;
23:2027-2033.)
Key Words: leptin 䡲 diabetes 䡲 arterial injury 䡲 smooth muscle cell proliferation 䡲 restenosis
ins2Akita mouse serves as a type I model of diabetes that does
not require administration of a chemical diabetogen such as
streptozotocin. leprdb/db mice have a mutation in the leptin
receptor gene, resulting in a mutant protein lacking the
cytoplasmic domain required for intracellular signaling.17
The leprdb/db model has many of the metabolic abnormalities
(albeit more severe) noted in human obese diabetic subjects,
such as obesity, hyperglycemia, and insulin resistance.17
We initially predicted that hyperglycemia or hyperinsulinemia would accelerate neointimal formation in response to
arterial injury. Hyperglycemia per se did not alter neointimal
formation in the ins2Akita mice, and neointimal formation was
nearly absent in leprdb/db mice. Analysis of the early response
to arterial injury in leprdb/db mice revealed substantial decreases in medial smooth muscle cell death. The near absence
of neointimal formation in the leprdb/db mouse suggests a new
potential role for leptin in the response to arterial injury.
N
umerous clinical trial and observational data have indicated that diabetic patients have a higher incidence of
restenosis after percutaneous coronary transluminal angioplasty and stent implantation compared with patients without
diabetes.1–5 Serial intravascular ultrasound studies suggest
that excessive neointimal hyperplasia is responsible for accelerated restenosis after angioplasty and coronary stent
placement in patients with diabetes and impaired glucose
tolerance.6,7 However, the relationships between the metabolic abnormalities present in diabetes and the cellular and
molecular processes involved in restenosis are poorly
understood.
A diabetic mouse model of accelerated neointimal formation would be a useful tool to understand the increased
incidence of restenosis in patients with diabetes. Balloon
angioplasty is technically challenging in the mouse because
of the small vessel size, and a variety of wire injury models
exist.8 –14 Recent work has demonstrated that reproducible
arterial injury can be performed in the mouse femoral artery
using an angioplasty guidewire.8,15 We chose to study neointimal formation after bilateral femoral arterial injury in the
diabetic, nonobese insulin 2 Akita (ins2Akita) and diabetic,
obese leptin receptor db/db (leprdb/db) mouse strains. Ins2Akita
mice have a spontaneous dominant mutation in the insulin 2
gene, resulting in defective proinsulin chain folding, reduced
 cell mass, hypoinsulinemia, and hyperglycemia.16 The
Methods
Mice
C57Bl/6 ins2Akita heterozygotes were obtained from Jackson Laboratory (stock No. 3548) and were bred with C57BL/6 mice to obtain
C57Bl/6 ins2Akita heterozygotes and wild-type littermate controls for
use in arterial injury experiments. A polymerase chain reaction
(PCR) assay16,18 to identify the ins2Akita mutation was first used to
identify C57Bl/6 ins2Akita heterozygotes. In all cases, a positive
genotype correlated with a fasting blood glucose ⬎300 mg/dL.
Received September 3, 2003; revision accepted September 9, 2003.
From the Departments of Medicine (K.S., J.T., A.T., H.M.D.) and Pathology (R.G.), Microscopy Shared Resource Facility (S.H.), Brookdale
Department of Molecular, Cell and Developmental Biology (S.H.), and the Zena and Michael A. Wiener Cardiovascular Institute (K.S., J.T., A.T.,
H.M.D.), New York, NY.
Correspondence to Hayes M. Dansky, MD, Cardiovascular Institute, Box 1269, Mount Sinai School of Medicine, One Gustave Levy Place, New York,
NY 10029. E-mail hayes.dansky@mssm.edu
© 2003 American Heart Association, Inc.
Arterioscler Thromb Vasc Biol. is available at http://www.atvbaha.org
2027
DOI: 10.1161/01.ATV.0000096394.32433.E9
2028
Arterioscler Thromb Vasc Biol.
November 2003
Therefore, a fasting glucose ⬎300 mg/dL was subsequently used to
identify ins2Akita mice. C57Bl/6 mice were identified as mice having
a fasting blood glucose ⬍200 mg/dL. C57BLKS/J leprdb/⫹ breeding
pairs were obtained from Jackson Laboratory (BKS.Cg-m, ⫹/⫹,
leprdb; stock No. 000642). The genotype of the mice was confirmed
using a PCR/restriction-length polymorphism assay that can identify
the db point mutation at the lepr locus.19 Phenotypes based on coat
color and body habitus agreed with PCR genotype in all cases.
Therefore, lepr⫹/⫹ and leprdb/db mice were subsequently identified by
phenotype. The incorporation of the misty (m) gene tightly linked to
the lepr locus allowed lepr⫹/⫹ and leprdb/db mice to be identified by
their phenotypic appearance at 8 weeks of age, as previously
described (http://jaxmice.jax.org/jaxmice-gi/jaxmicedb.cgi?objtype⫽pricedetail&stock⫽000642&dest⫽N). Briefly, body habitus
and coat color were used to phenotype the mice. Lepr⫹/⫹ (genotype:
m, lepr⫹/m, lepr⫹) mice were gray and lean; lepr⫹/db (genotype m,
⫹/⫹, leprdb) were black and lean; and leprdb/db (genotype: ⫹,
leprdb/⫹, leprdb) were black and obese. All procedures were
approved by the Institutional Animal Care and Use Committee,
consistent with the Guide for the Care and Use of Laboratory
Animals.
Downloaded from http://atvb.ahajournals.org/ by guest on September 30, 2016
Arterial Injury
Bilateral femoral artery procedure was performed as previously
described8,15 with a few modifications. The arteriotomy was made in
the superficial branch of the femoral artery, and a 0.3-mm angioplasty guidewire was used to denude and dilate the artery. The wire
was removed and the superficial femoral artery was ligated, diverting
blood flow down the deep femoral branch. Mice were given free
access to food and water before and after arterial injury, and arterial
specimens were obtained as previously described.8,15 Four-monthold female ins2akita/⫹ and ins2⫹/⫹ were euthanized 4 weeks after
arterial injury. Despite setting up large numbers of synchronous
matings of lepr⫹/db mice, we were unable to obtain sufficient numbers
of sex- and age-matched lepr⫹/⫹ and leprdb/db mice for euthanasia at
2 different time points after arterial injury. Therefore, we arbitrarily
euthanized female leprdb/db mice at 4 weeks and male leprdb/db mice at
2 weeks after arterial injury. Additional sections were obtained for
immunohistochemical staining of platelets (rabbit anti-mouse thrombocyte, Cederlane Laboratories, Ontario, Canada) and smooth muscle cells (␣-actin; Dako, 1A4). The area occupied by immunostained
cells (expressed as ratio of area of immunostained cells per arterial
circumference for platelets or area of immunostained cells per
intimal area for ␣-actin) was quantified for each injured artery.
Sections were then processed for terminal deoxynucleotidyl
transferase-mediated dUTP nick end-labeling (TUNEL) staining
using a commercially available kit according to the manufacturer’s
instructions (fluorescein in situ cell death detection kit, Roche).
Sections were also incubated with DAPI (Molecular Probes) to
identify nuclei. Fluorescein (reflecting TUNEL-positive cells) and
DAPI epifluorescence from all sections were viewed and simultaneously digitized using fixed exposure times on an epifluorescence
microscope. Ki67 (Novocastra) and active Caspase-3 (BD Pharmingen) staining were visualized with a Vectastain ABC Elite kit and
DAB substrate (Vector Laboratories). Comparisons between genotypes were performed using the Student’s t test using Prism software
(Graph Pad). Analysis of males and females were performed
separately.
Biochemical Measurements
At the time of euthanasia, mice were fasted for 6 hours and blood
was obtained by ventricular puncture used to obtain plasma for
lipoprotein fractions as previously described.20 Plasma was isolated
from tail vein blood samples from fasted mice for measurements of
plasma glucose (Sigma) and insulin (Linco).
Results
We determined whether the presence of type 1 or type 2
diabetes would promote neointimal formation after femoral
artery endovascular injury. Ins2Akita mutant mice were used as
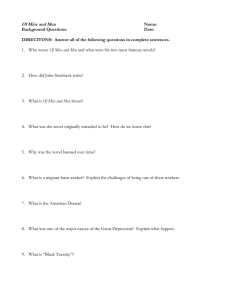
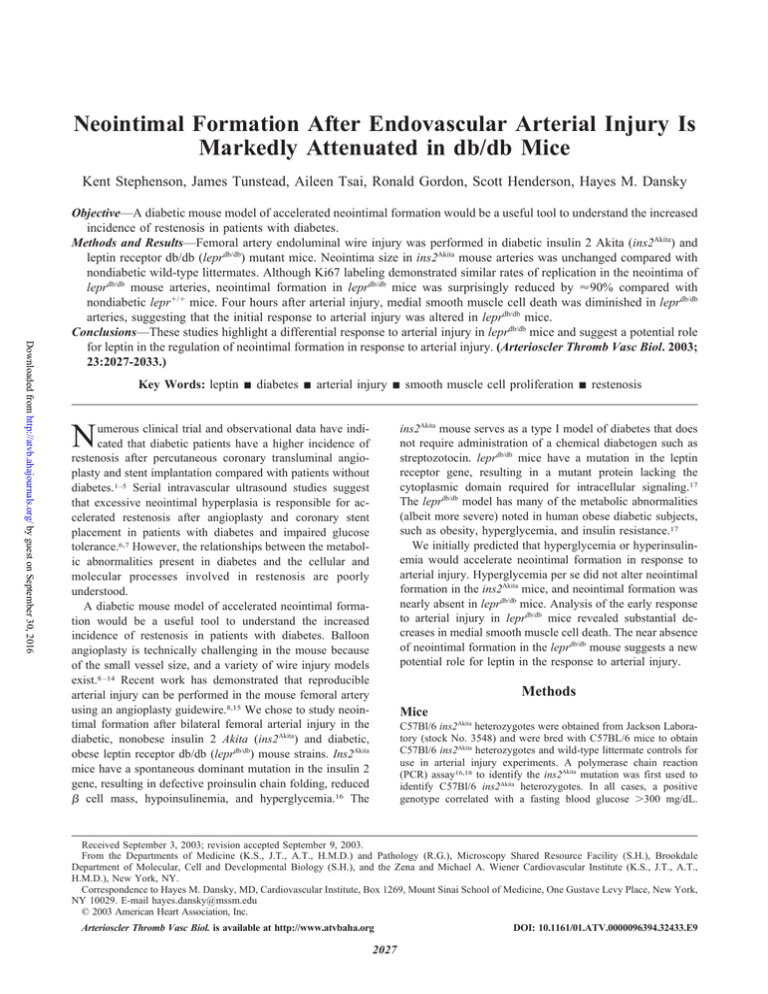
Figure 1. Representative photomicrographs (⫻100) of combined
Masson elastin–stained femoral artery sections and morphometric measurements from C57BL/6 wild-type and ins2Akita mice 4
weeks after injury. Neointima was present in sections from both
C57bL/6 wild-type mice (A) and ins2Akita mice (B). Morphometric
measurements revealed no significant difference in intimal area,
media area, or I/M ratio between the 2 groups of mice (C).
a model of type 1 diabetes. Ins2Akita mice had normal body
weight (27⫾1 versus 26⫾2 g; n⫽8 to 9 per group; P⫽NS)
and were hyperglycemic (411⫾48 versus 150⫾26 mg/dL,
n⫽7 to 9 per group, P⬍0.0001) compared with nondiabetic
littermate controls. The presence of type 1 diabetes did not
increase neointimal formation in the ins2Akita mouse model
(Figures 1A and 1B). No significant differences in intimal
area, medial area, and intimal to medial ratio (I/M) were
noted after arterial injury in ins2Akita mice compared with
nondiabetic wild-type controls (Figure 1C).
Femoral artery endovascular injury was also performed in
leprdb/db mutant mice, a model of type 2 diabetes. As previously reported,21,22 leprdb/db mice were obese, hyperglycemic,
hyperinsulinemic, and hypercholesterolemic (Table I and
Figure I, available online at http://atvb.ahajournals.org). After
arterial injury, the mean intimal area and I/M in male leprdb/db
mice were reduced by 88% and 85%, respectively, compared
with male lepr⫹/⫹ mice (Figures 2A and 2C). No differences
in medial area were noted in male mice after arterial injury
(Figure 2B). In female leprdb/db mice, intimal area and I/M
were reduced by 95% and 93%, respectively (Figures 2D and
2F). In contrast to male mice, there was also a small but
significant decrease in medial area in female leprdb/db mice
(Figure 2E). Histological examination of cross sections
through the femoral artery from lepr⫹/⫹ mice revealed the
presence of a neointima (Figures 3C and 3D). Many of these
neointimal cells stained positive with anti-smooth muscle cell
␣-actin antibody, indicating a smooth muscle cell phenotype
Dansky et al
Neointimal Formation in leprdb/db Mice
2029
Downloaded from http://atvb.ahajournals.org/ by guest on September 30, 2016
Figure 2. Morphometric measurements of cross sections of injured femoral arteries from lepr⫹/⫹ and leprdb/db mice. Measurements were
obtained from male (A, B, and C) and female (D, E, and F) mice 2 and 4 weeks after injury, respectively. Bars denote the mean⫾SEM
of intimal area (A and D), medial area (B and E), and I/M ratio (C and F). The number of arteries injured is denoted in parentheses.
(data not shown). In contrast, a neointima was absent in
nearly all sections from injured arteries from leprdb/db mice
(Figures 3E and 3F), and arteries appeared very similar to
sham-injured arteries (Figures 3A and 3B). Ki67 labeling was
performed on arterial sections from lepr⫹/⫹ mice and on the
limited number of femoral artery sections showing neointima
in leprdb/db mice (Figure 4). The percentage of intimal nuclei
labeled with Ki67 was not different in the neointima from
lepr⫹/⫹ compared with leprdb/db mice (32⫾7.4, n⫽6, versus
35⫾1.8, n⫽2; P⫽NS).
lepr⫹/⫹ and leprdb/db mice were euthanized 4 hours after
bilateral femoral artery injury to identify potential differences
in the initial response to arterial injury that may be responsible for the inhibition of neointima in leprdb/db mice. Analysis
of sham-injured arteries did not reveal any significant differences in lumen (0.028⫾0.007 versus 0.037⫾0.002 mm2,
P⫽NS) and vessel (0.040⫾0.009 versus 0.048⫾0.001 mm2,
P⫽NS) area in the femoral arteries of lepr⫹/⫹ mice compared
with leprdb/db mice. There were also no differences in the area
occupied by adherent platelets (0.001⫾0.0006 versus
0.0009⫾0.0004 mm, n⫽5, P⫽NS; see Figure 5). Alterations
in the arterial media were noted in lepr⫹/⫹ mice compared
with leprdb/db mice. The media from injured femoral arteries
from lepr⫹/⫹ mice contained multiple areas devoid of cell
nuclei (Figures 6C and 6D), with a decrease in the area
occupied by ␣-actin–positive cells compared with leprdb/db and
sham-injured lepr⫹/⫹ mice (Figure 6G). In contrast, the media
of injured femoral arteries harvested from leprdb/db mice
(Figures 6E and 6F) appeared similar to the media from
sham-injured femoral arteries (Figures 6A and 6B), with no
change in the area of ␣-actin–immunostained cells (Figure
6G). These findings suggested that mechanical injury of the
femoral artery resulted in medial smooth muscle cell death in
lepr⫹/⫹ mice but not in leprdb/db mice. To determine whether
the difference in smooth muscle cell nuclear dropout and
␣-actin staining was attributable to mechanical injury–induced apoptosis, TUNEL staining was performed on sections
derived from mice euthanized 4 hours after injury. Frequent
TUNEL-positive smooth muscle cells were noted in sections
derived from lepr⫹/⫹ femoral arteries (Figure IIA, available
online), but TUNEL-positive cells were rarely seen in arteries
harvested from lepr db/db mice (Figure IIB, available online).
The area occupied by TUNEL-positive cells per unit area of
media was markedly reduced in leprdb/db mice compared with
lepr⫹/⫹ mice (Figure IIC). Staining for activated caspase-3
(Figure III, available online) did not identify apoptotic cells in
the media 4 hours after arterial injury, suggesting that the
TUNEL staining highlighted cell damage attributable to
mechanical injury to cells and likely was not identifying
cellular apoptosis. These results indicate that the differences
in the extent of smooth muscle cell death 4 hours after arterial
injury were related to reductions in mechanical injury–
mediated smooth muscle cell necrosis in leprdb/db mice.
Discussion
Endovascular femoral artery injury was performed in mouse
models of type 1 and 2 diabetes mellitus in an effort to create
a mouse model in which diabetes accelerates the response to
arterial injury. Neointimal size was unchanged after femoral
artery injury of ins2Akita mice, a model of type 1 diabetes.
Similar to our results, type I diabetes did not alter neointimal
formation in streptozotocin-treated Sprague-Dawley rats.23 In
contrast, neointimal formation in leprdb/db mice, a model of
type II diabetes, was markedly attenuated. This seemingly
paradoxical effect is consistent with previous reports in
leprdb/db mice demonstrating impaired responses in several
models of tissue injury.24 –28 In response to FeCl3 or
photochemical-induced injury of the carotid arteries, platelet
2030
Arterioscler Thromb Vasc Biol.
November 2003
Downloaded from http://atvb.ahajournals.org/ by guest on September 30, 2016
Figure 5. Representative photomicrographs (⫻100) of femoral
artery sections from lepr⫹/⫹ and leprdb/db mice 4 hours after arterial injury. Anti-thrombocyte antibody staining revealed platelet
adherence to the injured arterial wall in femoral arteries from
lepr⫹/⫹ (A) and leprdb/db (B) mice.
Figure 3. Representative photomicrographs of combined Masson elastin–stained femoral artery sections from sham, lepr⫹/⫹,
and lepr db/db mice 4 weeks after arterial injury. Neointima is
noted in sections from a lepr⫹/⫹ mouse (C and D) and not in
sections from a leprdb/db mouse (E and F) nor from a shamtreated lepr⫹/⫹ mouse (A and B). B, D, and F are high magnification (⫻400) images of regions enclosed by a box in A, C, and E
(⫻100).
adherence and time of vessel occlusion is delayed in both
leprdb/db and lepob/ob mice.27,28 lepob/ob mice have a point
mutation in the leptin gene, resulting in absent leptin levels,
obesity, diabetes, and a phenotype nearly identical to the
Figure 4. Representative photomicrographs (⫻400) of Ki67
staining in femoral artery sections from lepr⫹/⫹ and leprdb/db mice
2 weeks after arterial injury. Ki67-positive nuclei (brown staining)
were noted in neointima from both lepr⫹/⫹ (A) and leprdb/db (B)
mice.
db/db mouse.29 Immunoreactive platelet deposition at 4 hours
was unchanged after endovascular wire injury of leprdb/db mice
in the present study. Variations in the type of injury model
and the cellular events comprising the response to injury may
underlie the differences in platelet adhesion among the
studies. In addition, thrombosis is an uncommon finding in
the wire injury model but is the end point in the FeCl3 and
photochemical injury models. Nevertheless, the near absence
of neointima in leprdb/db in the present study provides additional evidence for an attenuated vascular response to arterial
injury in leprdb/db mice.
Preservation of ␣-actin–positive medial smooth muscle
cells 4 hours after arterial injury indicates that differences
exist in the initial response to arterial injury in leprdb/db mice.
No significant differences in lumen size were observed in
sham-injured lepr⫹/⫹ and leprdb/db arteries. Alterations in
arterial caliber, tone, or compliance in the femoral artery of
leprdb/db mice may have affected the magnitude of the mechanical force imparted to the femoral artery by the wire,
resulting in inhibition of neointimal formation. Leptin has
been shown to increase sympathetic nerve activity and
arterial blood pressure in experimental models.30,31 Although
arterial blood pressure in lepob/ob mice has been reported to be
decreased compared with wild-type controls,32 other studies
have documented no change in blood pressure in both lepob/ob
and leprdb/db mice.30,33,34 Theoretically, a decrease in sympathetic nervous system activity or a decrease in arterial blood
pressure could have had inhibitory effects on the response to
arterial injury in leprdb/db mice in the present study. However,
arterial rings isolated from lepob/ob and leprdb/db mice have
enhanced contractile responses to norepinephrine and diminished relaxation to acetylcholine.35,36 The enhanced contractile responses would be expected to increase the mechanical
force of injury and do not account for the diminished
response to arterial injury in leprdb/db mice.
Dansky et al
Downloaded from http://atvb.ahajournals.org/ by guest on September 30, 2016
Figure 6. Immunohistochemical staining for smooth muscle
␣-actin in femoral artery sections obtained 4 hours after arterial
injury. A significant loss of medial ␣-actin–positive smooth muscle cells was noted in injured arterial sections from lepr⫹/⫹ mice
(C and D). The decrease in ␣-actin–immunostained medial cells
was not observed in arterial sections from leprdb/db mice (E and
F) and sham-injured lepr⫹/⫹ mice (A and B). Quantification of the
percentage of the media occupied by ␣-actin–positive cells is
displayed in G. B, D, and F are high-magnification (⫻400)
images of the boxed regions shown on low magnification (⫻100)
images A, C, and E.
Medial smooth muscle cell death after arterial injury has
been observed in numerous animal models of endovascular
injury.37–39 The extent of TUNEL-positive staining was reduced in leprdb/db mice compared with lepr⫹/⫹ mice, but we
were unable to document smooth muscle cell apoptosis by
staining for activated caspase-3 at 4 hours after arterial injury.
However, it is likely that both medial smooth muscle cell
necrosis and apoptosis play a role in medial smooth muscle
cell death after endovascular injury, because other reports
have documented chromatin condensation on transmission
electron microscopy and DNA fragmentation in medial
smooth muscle cells after mechanical endovascular injury in
the rat and the mouse.37–39 It is possible that decreases or
delays in medial smooth muscle cell death may have affected
the elaboration of chemotactic factors important for smooth
muscle cell migration into the intima. At 2 weeks after arterial
injury, Ki67 staining was unchanged in the neointima of
Neointimal Formation in leprdb/db Mice
2031
leprdb/db mice. These data suggest that the marked inhibition of
neointima formation in leprdb/db mice was not a direct result of
diminished cellular proliferation but was more likely attributable to inhibition of events important in the initiation of
smooth muscle migration in response to arterial injury.
The mechanism for the paradoxical reduction of neointimal
formation in leprdb/db mice may be difficult to elucidate
without the use of additional mutant mouse models. It is
intriguing to speculate that inhibition of leptin signaling at the
level of the vessel may have directly or indirectly impaired
the response to arterial injury in the leprdb/db mice. Leptin
administration just before FeCl3 or photochemical-induced
carotid injury restores the time to thrombosis (to that observed in wild-type mice) in mice lacking leptin (lepob/ob) but
not in mice with defective leptin signaling (leprdb/db).27,28
Arterial injury studies in the obese Zucker rat with a mutation
in the leptin receptor (fa/fa) have not been consistent. One
study demonstrated a 2-fold increase in neointimal formation
in balloon-injured arteries23; however, this was not reproduced in a subsequent study.40 In addition to the central role
of leptin in the regulation of food intake and energy balance,41
leptin seems to have numerous effects on vascular cells.
Experimental studies have documented effects of leptin on
vascular tone,42,43 endothelial reactive oxygen species generation,44 angiogenesis,45 proliferation of cultured vascular
smooth muscle cells,46 platelet aggregation,47 and HDL metabolism.21 Elevation in HDL cholesterol in leprdb/db mice may
have had an inhibitory effect on neointimal formation. Previous studies have demonstrated that human apoA-I exerts a
protective effect on neointimal formation in injured mouse
carotid arteries in hyperlipidemic mice.48,49 However, it is
unclear whether this protective effect of HDL on neointimal
formation occurs after endovascular injury in humans, because clinical studies have not clearly established low HDL
as a predictor of restenosis after revascularization
procedures.50,51
The understanding of the relationships among metabolic
parameters and restenosis may lead to the identification of
therapeutic agents that have salutary effects on both metabolism and restenosis. Thiazolidinediones, insulin-sensitizing
agents used for glycemic control in humans, have been
effective in reducing intimal formation in Zucker fatty and
Sprague-Dawley rats52,53 and in one small human trial.54
Additional arterial injury studies in leptin-dependent (such as
lepob/ob) and leptin-independent mouse models of type 2
diabetes should provide additional insight into whether the
attenuated response to arterial injury is specific for leptin
receptor mutant mice. It remains to be seen whether the
presence of insulin resistance and diabetes will increase the
response to arterial injury in the mouse.
Acknowledgments
This study was supported by Animal Models of Diabetic Complication Consortium NIH grant HL-70524 and from funds from the Zena
and Michael Wiener Cardiovascular Institute of the Mount Sinai
School of Medicine. Dr Stephenson was supported by the GlorneyRaisbeck Cardiovascular Fellowship from the New York Academy
of Medicine, New York, NY. The authors wish to thank Drs Edward
A. Fisher, Mark Taubman, and Jan Breslow for their scientific input.
2032
Arterioscler Thromb Vasc Biol.
November 2003
The authors gratefully acknowledge technical assistance from Otis
Defritas and Yolanda Ortaga.
References
Downloaded from http://atvb.ahajournals.org/ by guest on September 30, 2016
1. Van Belle E, Bauters C, Hubert E, Bodart JC, Abolmaali K, Meurice T,
McFadden EP, Lablanche JM, Bertrand ME. Restenosis rates in diabetic
patients: a comparison of coronary stenting and balloon angioplasty in
native coronary vessels. Circulation. 1997;96:1454 –1460.
2. Mercado N, Boersma E, Wijns W, Gersh BJ, Morillo CA, de Valk V, van
Es GA, Grobbee DE, Serruys PW. Clinical and quantitative coronary
angiographic predictors of coronary restenosis: a comparative analysis
from the balloon-to-stent era. J Am Coll Cardiol. 2001;38:645– 652.
3. Elezi S, Kastrati A, Pache J, Wehinger A, Hadamitzky M, Dirschinger J,
Neumann FJ, Schomig A. Diabetes mellitus and the clinical and angiographic outcome after coronary stent placement. J Am Coll Cardiol.
1998;32:1866 –1873.
4. Schofer J, Schluter M, Rau T, Hammer F, Haag N, Mathey DG. Influence
of treatment modality on angiographic outcome after coronary stenting in
diabetic patients: a controlled study. J Am Coll Cardiol. 2000;35:
1554 –1559.
5. Van Belle E, Perie M, Braune D, Chmait A, Meurice T, Abolmaali K,
McFadden EP, Bauters C, Lablanche JM, Bertrand ME. Effects of coronary stenting on vessel patency and long-term clinical outcome after
percutaneous coronary revascularization in diabetic patients. J Am Coll
Cardiol. 2002;40:410 – 417.
6. Kornowski R, Mintz GS, Kent KM, Pichard AD, Satler LF, Bucher TA,
Hong MK, Popma JJ, Leon MB. Increased restenosis in diabetes mellitus
after coronary interventions is due to exaggerated intimal hyperplasia: a
serial intravascular ultrasound study. Circulation. 1997;95:1366 –1369.
7. Takagi T, Akasaka T, Yamamuro A, Honda Y, Hozumi T, Morioka S,
Yoshida K. Impact of insulin resistance on neointimal tissue proliferation
after coronary stent implantation: intravascular ultrasound studies. J
Diabetes Complications. 2002;16:50 –55.
8. Roque M, Fallon JT, Badimon JJ, Zhang WX, Taubman MB, Reis ED.
Mouse model of femoral artery denudation injury associated with the
rapid accumulation of adhesion molecules on the luminal surface and
recruitment of neutrophils. Arterioscler Thromb Vasc Biol. 2000;20:
335–342.
9. Zhu B, Reardon CA, Getz GS, Hui DY. Both apolipoprotein E and
immune deficiency exacerbate neointimal hyperplasia after vascular
injury in mice. Arterioscler Thromb Vasc Biol. 2002;22:450 – 455.
10. Zhu B, Kuhel DG, Witte DP, Hui DY. Apolipoprotein E inhibits neointimal hyperplasia after arterial injury in mice. Am J Pathol. 2000;157:
1839 –1848.
11. Tanner FC, Boehm M, Akyurek LM, San H, Yang ZY, Tashiro J, Nabel
GJ, Nabel EG. Differential effects of the cyclin-dependent kinase inhibitors p27(Kip1), p21(Cip1), and p16(Ink4) on vascular smooth muscle
cell proliferation. Circulation. 2000;101:2022–2025.
12. Harmon KJ, Couper LL, Lindner V. Strain-dependent vascular
remodeling phenotypes in inbred mice. Am J Pathol. 2000;156:
1741–1748.
13. Mayr U, Mayr M, Li C, Wernig F, Dietrich H, Hu Y, Xu Q. Loss of p53
accelerates neointimal lesions of vein bypass grafts in mice. Circ Res.
2002;90:197–204.
14. Simon DI, Dhen Z, Seifert P, Edelman ER, Ballantyne CM, Rogers C.
Decreased neointimal formation in Mac-1(-/-) mice reveals a role for
inflammation in vascular repair after angioplasty. J Clin Invest. 2000;
105:293–300.
15. Reis ED, Roque M, Dansky H, Fallon JT, Badimon JJ, Cordon-Cardo C,
Shiff SJ, Fisher EA. Sulindac inhibits neointimal formation after arterial
injury in wild-type and apolipoprotein E-deficient mice. Proc Natl Acad
Sci U S A. 2000;97:12764 –12769.
16. Wang J, Takeuchi T, Tanaka S, Kubo SK, Kayo T, Lu D, Takata K,
Koizumi A, Izumi T. A mutation in the insulin 2 gene induces diabetes
with severe pancreatic beta-cell dysfunction in the Mody mouse. J Clin
Invest. 1999;103:27–37.
17. Chua SC Jr, Chung WK, Wu-Peng XS, Zhang Y, Liu SM, Tartaglia L,
Leibel RL. Phenotypes of mouse diabetes and rat fatty due to mutations
in the OB (leptin) receptor. Science. 1996;271:994 –996.
18. Yoshioka M, Kayo T, Ikeda T, Koizumi A. A novel locus, Mody4, distal
to D7Mit189 on chromosome 7 determines early-onset NIDDM in
nonobese C57BL/6 (Akita) mutant mice. Diabetes. 1997;46:887– 894.
19. Horvat S, Bunger L. Polymerase chain reaction-restriction fragment
length polymorphism (PCR-RFLP) assay for the mouse leptin receptor
(Lepr(db)) mutation. Lab Anim. 1999;33:380 –384.
20. Dansky HM, Charlton SA, Sikes JL, Heath SC, Simantov R, Levin LF,
Shu P, Moore KJ, Breslow JL, Smith JD. Genetic background determines
the extent of atherosclerosis in ApoE-deficient mice. Arterioscler Thromb
Vasc Biol. 1999;19:1960 –1968.
21. Silver DL, Jiang XC, Tall AR. Increased high density lipoprotein (HDL),
defective hepatic catabolism of ApoA-I and ApoA-II, and decreased
ApoA-I mRNA in ob/ob mice: possible role of leptin in stimulation of
HDL turnover. J Biol Chem. 1999;274:4140 – 4146.
22. Kobayashi K, Forte TM, Taniguchi S, Ishida BY, Oka K, Chan L. The
db/db mouse, a model for diabetic dyslipidemia: molecular characterization and effects of Western diet feeding. Metabolism. 2000;49:22–31.
23. Park SH, Marso SP, Zhou Z, Foroudi F, Topol EJ, Lincoff AM. Neointimal hyperplasia after arterial injury is increased in a rat model of
non-insulin-dependent diabetes mellitus. Circulation. 2001;104:815– 819.
24. Tsuboi R, Shi CM, Rifkin DB, Ogawa H. A wound healing model using
healing-impaired diabetic mice. J Dermatol. 1992;19:673– 675.
25. Lerman OZ, Galiano RD, Armour M, Levine JP, Gurtner GC. Cellular
dysfunction in the diabetic fibroblast: impairment in migration, vascular
endothelial growth factor production, and response to hypoxia. Am J
Pathol. 2003;162:303–312.
26. Stepanovic V, Awad O, Jiao C, Dunnwald M, Schatteman GC. Leprdb
diabetic mouse bone marrow cells inhibit skin wound vascularization but
promote wound healing. Circ Res. 2003;92:1247–1253.
27. Konstantinides S, Schafer K, Koschnick S, Loskutoff DJ. Leptindependent platelet aggregation and arterial thrombosis suggests a
mechanism for atherothrombotic disease in obesity. J Clin Invest. 2001;
108:1533–1540.
28. Bodary PF, Westrick RJ, Wickenheiser KJ, Shen Y, Eitzman DT. Effect
of leptin on arterial thrombosis following vascular injury in mice. JAMA.
2002;287:1706 –1709.
29. Leibel RL, Chung WK, Chua SC Jr. The molecular genetics of rodent
single gene obesities. J Biol Chem. 1997;272:31937–31940.
30. Aizawa-Abe M, Ogawa Y, Masuzaki H, Ebihara K, Satoh N, Iwai H,
Matsuoka N, Hayashi T, Hosoda K, Inoue G, Yoshimasa Y, Nakao K.
Pathophysiological role of leptin in obesity-related hypertension. J Clin
Invest. 2000;105:1243–1252.
31. Haynes WG, Morgan DA, Walsh SA, Mark AL, Sivitz WI. Receptormediated regional sympathetic nerve activation by leptin. J Clin Invest.
1997;100:270 –278.
32. Mark AL, Shaffer RA, Correia ML, Morgan DA, Sigmund CD, Haynes
WG. Contrasting blood pressure effects of obesity in leptin-deficient
ob/ob mice and agouti yellow obese mice. J Hypertens. 1999;17:
1949 –1953.
33. Swoap SJ. Altered leptin signaling is sufficient, but not required, for
hypotension associated with caloric restriction. Am J Physiol Heart Circ
Physiol. 2001;281:H2473–H2479.
34. Koya D, Haneda M, Nakagawa H, Isshiki K, Sato H, Maeda S, Sugimoto
T, Yasuda H, Kashiwagi A, Ways DK, King GL, Kikkawa R. Amelioration of accelerated diabetic mesangial expansion by treatment with a
PKC beta inhibitor in diabetic db/db mice, a rodent model for type 2
diabetes. FASEB J. 2000;14:439 – 447.
35. Winters B, Mo Z, Brooks-Asplund E, Kim S, Shoukas A, Li D, Nyhan D,
Berkowitz DE. Reduction of obesity, as induced by leptin, reverses
endothelial dysfunction in obese (Lep(ob)) mice. J Appl Physiol. 2000;
89:2382–2390.
36. Kanie N, Kamata K. Contractile responses in spontaneously diabetic
mice, I: involvement of superoxide anion in enhanced contractile
response of aorta to norepinephrine in C57BL/KsJ(db/db) mice. Gen
Pharmacol. 2000;35:311–318.
37. Perlman H, Maillard L, Krasinski K, Walsh K. Evidence for the rapid
onset of apoptosis in medial smooth muscle cells after balloon injury.
Circulation. 1997;95:981–987.
38. Pollman MJ, Hall JL, Gibbons GH. Determinants of vascular smooth
muscle cell apoptosis after balloon angioplasty injury: influence of redox
state and cell phenotype. Circ Res. 1999;84:113–121.
39. Sata M, Sugiura S, Yoshizumi M, Ouchi Y, Hirata Y, Nagai R. Acute and
chronic smooth muscle cell apoptosis after mechanical vascular injury
can occur independently of the Fas-death pathway. Arterioscler Thromb
Vasc Biol. 2001;21:1733–1737.
40. Zhou Z, Wang K, Penn MS, Marso SP, Lauer MA, Forudi F, Zhou X, Qu
W, Lu Y, Stern DM, Schmidt AM, Lincoff AM, Topol EJ. Receptor for
Dansky et al
41.
42.
43.
44.
45.
46.
Downloaded from http://atvb.ahajournals.org/ by guest on September 30, 2016
47.
48.
AGE (RAGE) mediates neointimal formation in response to arterial
injury. Circulation. 2003;107:2238 –2243.
Friedman JM, Halaas JL. Leptin and the regulation of body weight in
mammals. Nature. 1998;395:763–770.
Quehenberger P, Exner M, Sunder-Plassmann R, Ruzicka K, Bieglmayer
C, Endler G, Muellner C, Speiser W, Wagner O. Leptin induces
endothelin-1 in endothelial cells in vitro. Circ Res. 2002;90:711–718.
Cao R, Brakenhielm E, Wahlestedt C, Thyberg J, Cao Y. Leptin induces
vascular permeability and synergistically stimulates angiogenesis with
FGF-2 and VEGF. Proc Natl Acad Sci U S A. 2001;98:6390 – 6395.
Yamagishi SI, Edelstein D, Du XL, Kaneda Y, Guzman M, Brownlee M.
Leptin induces mitochondrial superoxide production and monocyte chemoattractant protein-1 expression in aortic endothelial cells by increasing
fatty acid oxidation via protein kinase A. J Biol Chem. 2001;276:
25096 –25100.
Sierra-Honigmann MR, Nath AK, Murakami C, Garcia-Cardena G,
Papapetropoulos A, Sessa WC, Madge LA, Schechner JS, Schwabb MB,
Polverini PJ, Flores-Riveros JR. Biological action of leptin as an
angiogenic factor. Science. 1998;281:1683–1686.
Oda A, Taniguchi T, Yokoyama M. Leptin stimulates rat aortic smooth
muscle cell proliferation and migration. Kobe J Med Sci. 2001;47:
141–150.
Nakata M, Yada T, Soejima N, Maruyama I. Leptin promotes aggregation
of human platelets via the long form of its receptor. Diabetes. 1999;48:
426 – 429.
Dimayuga P, Zhu J, Oguchi S, Chyu KY, Xu XO, Yano J, Shah PK,
Nilsson J, Cercek B. Reconstituted HDL containing human apoli-
49.
50.
51.
52.
53.
54.
Neointimal Formation in leprdb/db Mice
2033
poprotein A-1 reduces VCAM-1 expression and neointima formation
following periadventitial cuff-induced carotid injury in apoE null mice.
Biochem Biophys Res Commun. 1999;264:465– 468.
De Geest B, Zhao Z, Collen D, Holvoet P. Effects of adenovirus-mediated
human apo A-I gene transfer on neointima formation after endothelial
denudation in apo E-deficient mice. Circulation. 1997;96:4349 – 4356.
Bittner V, Hardison R, Kelsey SF, Weiner BH, Jacobs AK, Sopko G.
Non-high-density lipoprotein cholesterol levels predict five-year outcome
in the Bypass Angioplasty Revascularization Investigation (BARI). Circulation. 2002;106:2537–2542.
Boccuzzi SJ, Weintraub WS, Kosinski AS, Roehm JB, Klein JL.
Aggressive lipid lowering in postcoronary angioplasty patients with
elevated cholesterol (the Lovastatin Restenosis Trial). Am J Cardiol.
1998;81:632– 636.
Aizawa Y, Kawabe J, Hasebe N, Takehara N, Kikuchi K. Pioglitazone
enhances cytokine-induced apoptosis in vascular smooth muscle cells and
reduces intimal hyperplasia. Circulation. 2001;104:455– 460.
Shinohara E, Kihara S, Ouchi N, Funahashi T, Nakamura T, Yamashita
S, Kameda-Takemura K, Matsuzawa Y. Troglitazone suppresses intimal
formation following balloon injury in insulin-resistant Zucker fatty rats.
Atherosclerosis. 1998;136:275–279.
Takagi T, Akasaka T, Yamamuro A, Honda Y, Hozumi T, Morioka S,
Yoshida K. Troglitazone reduces neointimal tissue proliferation after
coronary stent implantation in patients with non-insulin dependent
diabetes mellitus: a serial intravascular ultrasound study. J Am Coll
Cardiol. 2000;36:1529 –1535.
Downloaded from http://atvb.ahajournals.org/ by guest on September 30, 2016
Neointimal Formation After Endovascular Arterial Injury Is Markedly Attenuated in
db/db Mice
Kent Stephenson, James Tunstead, Aileen Tsai, Ronald Gordon, Scott Henderson and Hayes M.
Dansky
Arterioscler Thromb Vasc Biol. 2003;23:2027-2033; originally published online September 18,
2003;
doi: 10.1161/01.ATV.0000096394.32433.E9
Arteriosclerosis, Thrombosis, and Vascular Biology is published by the American Heart Association, 7272
Greenville Avenue, Dallas, TX 75231
Copyright © 2003 American Heart Association, Inc. All rights reserved.
Print ISSN: 1079-5642. Online ISSN: 1524-4636
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://atvb.ahajournals.org/content/23/11/2027
Data Supplement (unedited) at:
http://atvb.ahajournals.org/content/suppl/2004/01/30/23.11.2027.DC1.html
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Arteriosclerosis, Thrombosis, and Vascular Biology can be obtained via RightsLink, a service of the
Copyright Clearance Center, not the Editorial Office. Once the online version of the published article for
which permission is being requested is located, click Request Permissions in the middle column of the Web
page under Services. Further information about this process is available in the Permissions and Rights
Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Arteriosclerosis, Thrombosis, and Vascular Biology is online
at:
http://atvb.ahajournals.org//subscriptions/