M. J. Ratain1, S. Kelsey3, L. Janisch1, J. Smith3, N.F. Go3,T
advertisement

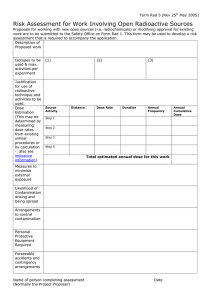
Imetelstat Sodium (GRN163L), a Telomerase Inhibitor: Tolerability, Pharmacokinetics and Pharmacodynamic Activity Using an Intermittent Once Every Four Weeks Dosing Schedule in Patients With Advanced Solid Tumors 1 Ratain , M. J. S. L. J. N.F. P.M. 1University of Chicago, Chicago, IL, USA; 2 Karmanos Cancer Institute, Detroit, MI, USA; 3Geron Corp, Menlo Park, CA, USA. Telomeres Results Rational • Purpose: Multiple doses and dosing schedules of imetelstat were assessed in a Phase I study in patients with advanced solid tumors. Endpoints included safety, tolerability and pharmacokinetics. • Initial Dosing: Weekly imetelstat • TTAGGG hexa-nucleotide repeats that cap the ends of chromosomes and prevent chromosomal fusion.1 • Shorten by 50-200 basepairs (bp) per cell division.2-3 • Critically short telomeres may cause growth arrest and senescence.4 • Telomere length is shorter in cancer cells than normal somatic cells.9 Telomerase • Consists of at least two essential components, the RNA template (hTR) and the catalytic subunit (hTERT). • Counters telomere loss by the direct addition of TTAGGG repeats to the chromosome ends.1 • Repressed in most somatic cells5 and downregulated in hematopoietic and other somatic stem cells.6 Telomerase and cancer • Telomerase activation and preservation of telomeres are required for immortalization.7-8 • Telomerase is highly activated in cancer and cancer stem cells, which have been shown to be sensitive to telomerase inhibition in several models.9 The dose-limiting toxicity (DLT) was thrombocytopenia, often seen after the first 3 weeks • Intermittent Dosing: Days 1 and 8 of a 21-day cycle Figure 1. Imetelstat Sodium (GRN163L) Structure 5’ end • Modified DNA oligonucleotide (13 nts + lipid) • N3’→P5’ phosphoramidate backbone Improves binding affinity and chemical/enzymatic stability C16 • Palmitoyl (C16) lipid covalently attached to 5’ thio-phosphate of first nucleotide Improves in vivo potency (cell uptake, Hematologic toxicity observed but may be mitigated with the intermittent dosing; other observed toxicities were mostly mild. The 9.4 mg/kg dose using this intermittent schedule is currently being tested in Phase II studies. • Alternative Dosing Schedule: Once every 28-days The purpose of this regimen is to assess the effect of a longer interval between doses on the onset and duration of cytopenias after a single dose of imetelstat and to ascertain the maximum tolerated dose. The current analysis includes 16 patients following this dosing schedule. • Design: Phase I, sequential cohort, 3+3 dose escalation, multicenter trial • Patient population: Adults with refractory advanced solid tumors Major Inclusion criteria: Patients with malignancy that is evaluable or measurable; refractory or not amenable to standard therapy, Karnofsky status ≥70%, anticipated life expectancy ≥3 months. Major Exclusion Criteria: Primary malignancy or active metastasis in CNS; Hematologic malignancies; Hemoglobin <9.0 g/dL; ANC <1,500 /mm3; Platelet count <100,000 /mm3; significant serum chemistry abnormality (bilirubin, AST, ALT, albumin, creatinine), active uncontrolled bleeding/ bleeding diathesis, elevated PT or aPTT. 3’ end O H N OH O S NP linkage Na + • Endpoints: Safety (primary), pharmacokinetics and efficacy (secondary), pharmacodynamics of telomerase activity (exploratory) Plasma samples were collected to test pharmacokinetic effects Peripheral blood mononuclear cells (PBMC) collected to further test pharmacodynamic effects. were • Dose Limiting Toxicity (DLT): Grade 4 non-hematologic toxicity, grade 3 non-hematologic toxicity lasting >3 days or not medically-controllable, grade 4 neutropenia lasting >5 days, ≥ grade 3 neutropenia associated with fever, grade 4 thrombocytopenia, inability to complete cycle 1 or treatment delays of >2 weeks from next scheduled dose due to any toxicity thought to be associated with study drug. 1 H.L.Kindler , • Sixteen patients received imetelstat on day 1 of a 28 day cycle, up to the data cut-off of October 6, 2010. • Intermittent dosing using an 11.7 mg/kg dose every 28 days ameliorated the dose limiting Grade 3 and 4 thrombocytopenia occasionally observed with the more frequent dosing schedule (see Figure 2) . • The median age was 59.7 years (range 39-80) and the sex distribution was equal. 11.7 mg/kg day 1 & 8 of 21 day cycle Dosing and Disposition • Sixteen (16) patients received at least 1 infusion of imetelstat. 3 patients in the 9.4mg/kg cohort • One patient in the 11.7mg/kg cohort is currently in treatment, and 12 of 15 patients discontinued the study due to disease progression. 400 300 200 • Systemic exposure of imetelstat increased with dose (range of 4.8 to 11.7 mg/kg) after a 2-hour IV infusion with T1/2 ranging from 3.6 to 5.2 hours (data not shown). 100 0 2 4 – Gr1 8 10 Gr2 Gr3 Gr4 6 14 12 16 18 Weekly Imetelstat AUC (μg/mL*hr) • Seven patients in the 11.7 mg/kg cohort received 2 or more doses, and 4 of 7 experienced dose delays, which were primarily due to hematological toxicity. • No dose delays occurred in the 9.4mg/kg cohort. • Two patients in the 11.7 mg/kg cohort discontinued imetelstat following an infusion reaction. • Due to dose delays in cycle 2 and hematological toxicity, the maximum administered dose was 11.7 mg/kg. This dose and schedule is also being tested in Phase II studies. 600 500 800 – exposure is based on 15 – mg/kg tiw dosing in mice, which was 400 – associated with both a ≥50% inhibition – of telomerase in tumors and a 0 – concomitant inhibition of tumor growth. 300 200 100 4 6 Gr1 Gr2 Gr3 Gr4 0 Screen 2 8 • No significant toxicity was observed at 9.4 mg/kg. Non-hematological adverse events ≥ Grade 3: intestinal obstruction, bile duct obstruction, blood creatinine increased, bronchitis, cholangitis, diffuse large B-cell lymphoma, headache, hyperglycemia, hypersensitivity/ infusion reaction, hypertension, hyponatremia, and pituitary tumor benign. All were assessed as unrelated to imetelstat except one infusion-related reaction in the 11.7 mg/kg cohort. • Two patients experienced an infusion reaction, both in the 11.7 mg/kg cohort, including a Grade 3 reaction classified as a dose limiting toxicity (DLT) and a Grade 1 reaction. • As previously observed with other dosing schedules, transient (<24hr) prolongation of aPTT occurred without clinical sequelae in 12/16 (75%) of patients. • Cytopenias were observed in both dose groups, which were mostly Grade 1-2 in severity. See Table 1. ι 4.8 ι 7.5 ι 9.4 10 12 14 16 18 20 • Cytopenias are delayed in onset and may still delay the administration of the next dose even using a once every 28 day schedule. The periodicity of the cytopenias is consistent with an effect on the hematopoietic progenitor population which known to express telomerase. • Pharmacodynamic (PD) evidence of target inhibition has been observed in selected patient tissues. • A once every 28 day schedule presents a reasonable alternative to the intermittent dosing schedule of Day 1 and 8 every 21 days, although the dose intensity per cycle is less. This schedule is currently being tested in ongoing Phase II studies. ι 6.0 ι 11.7 Imetelstat Dose (mg/kg) • Peripheral blood mononuclear cells (PBMC) from whole blood were collected pre- and 24h after a single dose of imetelstat on cycle-1 day-1 and analyzed for telomerase activity using the TRAP assay (Telomere Repeat Amplification Protocol). Figure 4: Inhibition of telomerase activity in peripheral blood mononuclear cells 24 hours after a single dose of imetelstat Weeks • The dose-limiting toxicity is neutropenia and thrombocytopenia. Pharmacodynamics: Telomerase Activity 1500 – Safety • Imetelstat infusions were generally well tolerated. Exposure† – †Target 400 1600 – – Target - Dosed and had platelets test done – 1200 – 11.7 mg/kg day 1 of 28 day cycle 2000 – 20 Weeks Dose Escalation 2400 – Screen • Patient weekly plasma AUC values were calculated, and individual values for each dose group are shown in Figure 3. • Plasma samples were obtained prior to and following imetelstat infusions for determination of imetelstat concentration by a validated hybridization-ELISA assay. Figure 3. Weekly AUCinf in patients and in xenograft mice (dashed line) • The once every 28 day dosing schedule is well tolerated. • The exposure in patients (AUC values at 7.5 mg/kg and above) is higher than the exposure associated with tumor growth inhibition in xenograft models. - Dosed and had platelets test done 600 500 Summary Patient Pharmacokinetics Figure 2. Platelet levels vs time with 11.7 mg/kg on different dosing schedules • All patients received prior cytotoxic regimens (mean 4.1), and 9 (56%) had prior radiation therapy. 2 LoRusso Results Platelet Levels • Grade 3 or higher non-hematological adverse events were reported in 5/16 (31%) patients. O P TAGGGTTAGACAA 13-base aminoglycerol complement of thioRNA template phosphate region linker palmitoyl group • Treatment: Successive cohorts of a single dose of 9.4 or 11.7mg/kg imetelstat given by 2-hour IV infusion on day 1 of a 28 day cycle, with delays up to 2 weeks allowed between cycles. 1 M.L.Maitiland , Results • Patients received a median of 2 (range 1-3) cycles prior to disease progression. Methods 3 Lin , Baseline Characteristics 13 patients in the 11.7mg/kg cohort. PK, biodistribution) • Molecular Weight ≈4600 3 Go ,T. Allowed for plasma concentrations and exposures to be achieved consistent with efficacy in the preclinical models. Imetelstat: A Telomerase Inhibitor • 5’palmitoylated 13-mer thio-phosphoramidate oligonucleotide complimentary to the hTR template in telomerase. • Inhibits telomerase by acting as a competitive inhibitor of the enzyme.10 • Demonstrates telomerase inhibitory and cancer growth and metastasis inhibitory effects in both in vitro and in vivo preclinical models.10-13 3 Smith , Platelets (10^3/uL) • Preservation of telomere length is crucial to cell survival and enabling the unlimited replicative capacity of cancer cells. • Telomerase is a promising target for novel cancer therapeutics. • Imetelstat (GRN163L) is the only telomerase inhibitor in clinical development. Dose 1 Janisch , Platelets (10^3/uL) Introduction 3 Kelsey , Acknowledgements • The authors gratefully acknowledge Deena Gruver, Shuling Hwang and Dianne Morfeld for their important contributions and dedicated work throughout this study. • The authors would like to acknowledge the patients and their families who participated in this study and the investigators and study coordinators who made this study possible. • Funding provided by Geron Corp. 1000 – Table 1. Hematological adverse events by grade Dose (mg/kg) 9.4 # of Patients 3 Thrombocytopenia Grade 1 2 Grade 2 0 Grade 3 -4 0 Anemia Grade 1 2 Grade 2 0 Grade 3-4 0 Neutropenia Grade 1 0 Grade 2 0 Grade 3 0 Grade 4 0 11.7 13 12 1 0 Total 16 14 1 0 8 1 0 10 1 0 0 3 1 1 0 3 1 1 Percent Telomerase Activity Change 50 – References 0– -50 – -100 – ι 6.0 ι 7.5 ι 9.4 ι 11.7 Imetelstat Dose (mg/kg) *note single outlier with significant increase in post-treatment telomerase activity • Significant inhibition of telomerase was observed at all dose levels above 7.5 mg/kg. • Median telomerase inhibition for the 9.4 mg/kg group was 34.0% (p value 0.2891*). • Median telomerase inhibition for the 11.7 mg/kg group was 48.0% (p value 0.0215). • Overall median telomerase inhibition from 23 patients (cohorts 6.0 to 11.7mg.kg) tested was 40.5% (p value 0.0106). 1. McEachern MJ. Annu Rev Genet. 2000;34:331-58. 2. Harley CB. Oncogene. 2002;21:494-502. 3. Harley CB. Nature. 1990;345:458-60. 4. Bodnar AG. Science. 1998;279:349-52. 5. Wright WE. Dev Genet. 1996;18(2):173-9. 6. Chiu CP. Proc Soc Exp Biol Med. 1997;214(2):99-106. 7. Counter CM. EMBO J. 1992;11(5):1921-9. 8. Kim NW. Science. 1994;266(5193):2011-5. 9. Harley CB. Nature Reviews Cancer. 2008;8:167-79. 10. Brittney-Shea H, et al. Oncogene. 2005;24:5262-8. 11. Dikmen ZG, et al. Cancer Res. 2005;65:7866-73. 12. Djojosobruto MW, et al. Hepatol. 2005;42:1-11. 13. Hochreiter AE, et al. Clin Cancer Res. 2006;12:3184-92. Poster (#388) presented at the EORTC-NCI-AACR symposium on “Molecular Targets and Cancer Therapeutics” in Berlin, Germany, 16-19 November 2010