Comparison of Presence and Extent of Coronary Narrowing in Patients With Left
Bundle Branch Block Without Diabetes Mellitus to Patients With and Without
Left Bundle Branch Block But With Diabetes Mellitus
Ozcan Ozeke, MD*, Dursun Aras, MD, Bulent Deveci, MD, Mehmet Fatih Ozlu, MD,
Ozgul Malcok Gurel, MD, Aytun Canga, MD, Veli Kaya, MD, Tumer Erdem Guler, MD,
Ali Yildiz, MD, Kumral Ergun, MD, Mehmet Timur Selcuk, MD, Serkan Topaloglu, MD,
Orhan Maden, MD, and Omac Tufekcioglu, MD
We prospectively analyzed the clinical, echocardiographic, and coronary arteriographic data of 51 patients with type 2 diabetes mellitus with left bundle branch block
(LBBB), 51 patients with type 2 diabetes mellitus without LBBB, and 51 patients with
isolated LBBB matched for age and gender. Extent of coronary artery disease (CAD)
was classified according to the standard method into 1-, 2-, or 3-vessel disease and
was estimated by calculation of the Gensini score. The left ventricular ejection
fraction was analyzed by echocardiography. Age, gender, and percentage of patients
with a smoking habit or family history of CAD did not differ among the groups. The
rates of hypertension and levels of serum creatinine, cholesterol, and triglycerides
were statistically higher in group I compared with the other 2 groups. Patients with
diabetes and LBBB (group I) had significantly higher scores for the severity (Gensini
score) of CAD (p <0.001) and more 3-vessel disease (p <0.001). After adjustment for
hypertension, hypertriglyceridemia, and hypercholesterolemia with covariance analysis, the presence of LBBB was also associated with a higher Gensini score in patients
with diabetes compared with those with diabetes but without LBBB and those with
isolated LBBB (p <0.001). The present study, for the first time, has shown that
patients with type 2 diabetes mellitus and concomitant LBBB have more severe and
extensive CAD and advanced left ventricular dysfunction compared with those with
diabetes but without LBBB and those with isolated LBBB. © 2006 Elsevier Inc. All
rights reserved. (Am J Cardiol 2006;97:857– 859)
Diabetes mellitus is widely recognized as a significant risk
factor for the development of cardiovascular disease and is
an independent risk factor for accelerated atherosclerosis
with more severe and extensive lesions compared with those
without diabetes.1–3 Left bundle branch block (LBBB) is
also associated with an increased risk of developing overt
cardiovascular disease and increased cardiac mortality.4,5
Although some investigators have suggested that asymptomatic patients with acquired LBBB but without other risk
factors have a good prognosis,6,7 others have suggested that
LBBB is not associated with a benign prognosis. The Framingham study demonstrated that the 10-year cardiovascular mortality rate after the onset of LBBB is 50%.5 In
patients with chronic coronary artery disease (CAD) in the
Coronary Artery Surgery Study (CASS) registry,8 LBBB
was a strong predictor of mortality, independent of the
degree of heart failure, extent of coronary disease, and other
important variables. Recent reports have suggested that
Department of Cardiology, Yuksek Ihtisas Hospital, Ankara, Turkey.
Manuscript received August 30, 2005; revised manuscript received and
accepted October 3, 2005.
* Corresponding author: Tel: 90-505-383-6773; fax: 90-312-312-4120.
E-mail address: ozcanozeke@gmail.com (O. Ozeke).
0002-9149/06/$ – see front matter © 2006 Elsevier Inc. All rights reserved.
doi:10.1016/j.amjcard.2005.10.023
the presence of LBBB in patients with type 2 diabetes
mellitus may indicate worse left ventricular systolic dysfunction compared with those without LBBB and compared with those without diabetes but with LBBB.9 We
planned this study to investigate the effect of LBBB on
the presence and extent of CAD in diabetic patients by
examining the Gensini score, which was used to define
the severity of coronary atherosclerosis determined angiographically in patients with type 2 diabetes mellitus.
•••
We prospectively analyzed the clinical, echocardiographic,
and coronary arteriographic data in 102 patients with type 2
diabetes mellitus with and without LBBB and in 51 patients
with isolated LBBB matched for age and gender. The major
risk factors for CAD, such as age, gender, family history,
hyperlipidemia, and hypertension, were determined. Diabetes mellitus was considered present if the patient had a
history of diabetes, had a fasting blood glucose ⬎126 mg/dl,
or used an antidiabetic medication. We defined LBBB as
meeting all the following criteria: (1) QRS ⬎0.12 ms in the
presence of normal sinus or supraventricular rhythm; (2) QS
or RS complex in lead V1; (3) broad or notched R waves in
leads V5 and V6 or a RS pattern; and (4) the absence of a Q
www.AJConline.org
858
The American Journal of Cardiology (www.AJConline.org)
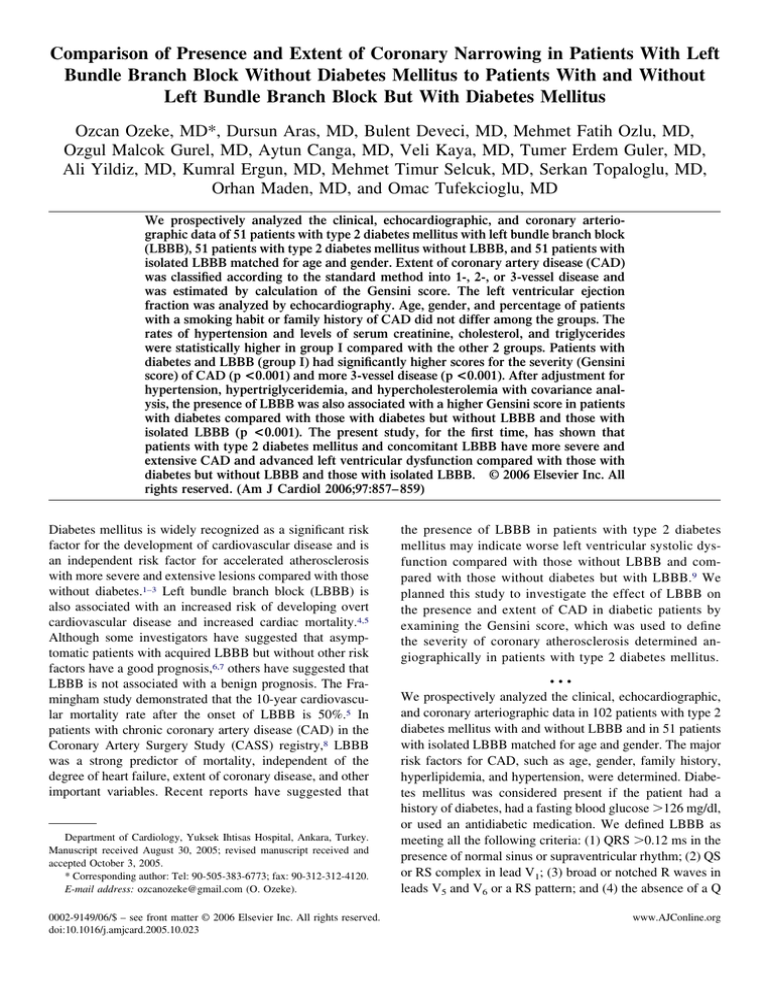
Table 1
Clinical, laboratory, echocardiographic, and angiographic data of
study population
Variable
DM With
LBBB
(n ⫽ 51)
DM Without
LBBB
(n ⫽ 51)
Isolated
LBBB
(n ⫽ 51)
p Value
Age (yrs)
Women (%)
Hypertension (%)
Family history for
CAD (%)
Smoking (%)
Triglycerides
(mg/dl)
Cholesterol
(mg/dl)
HDL-C (mg/dl)
LDL-C (mg/dl)
Creatinine (mg/dl)
BMI (kg/m2)
LVEF (%)
Presence of CAD
Single-LAD (%)
Single-LCx (%)
Single-RCA (%)
2-Vessel (%)
3-Vessel (%)
Gensini score
64 ⫾ 9
31 (61%)
39 (77%)
12 (23%)
64 ⫾ 9
28 (55%)
31 (61%)
9 (18%)
63 ⫾ 11
29 (57%)
27 (45%)
10 (20%)
NS
NS
⬍0.001
NS
7 (14%)
188 ⫾ 97
7 (14%)
168 ⫾ 83
6 (12%)
135 ⫾ 77
NS
⬍0.001
197 ⫾ 49
188 ⫾ 43
173 ⫾ 34
⬍0.001
41 ⫾ 11
118 ⫾ 44
1.1 ⫾ 0.5
28 ⫾ 4
32 ⫾ 11
35 (69%)
7 (14%)
2 (4%)
1 (2%)
9 (18%)
16 (31%)
50 ⫾ 58
43 ⫾ 11
112 ⫾ 37
1.0 ⫾ 0.4
28 ⫾ 6
52 ⫾ 10
28 (55%)
6 (12%)
3 (6%)
2 (4%)
8 (16%)
9 (18%)
28 ⫾ 43
44 ⫾ 12
99 ⫾ 29
0.9 ⫾ 0.3
27 ⫾ 3
45 ⫾ 13
23 (45%)
6 (12%)
2 (4%)
2 (4%)
5 (12%)
6 (12%)
14 ⫾ 26
NS
NS
0.037
NS
⬍0.001
0.05
NS
NS
NS
NS
0.04
⬍0.001
BMI ⫽ body mass index; LCx ⫽ circumflex artery; DM ⫽ diabetes
mellitus; HDL-C ⫽ high-density lipoprotein cholesterol; LAD ⫽ left
anterior descending artery; LDL-C ⫽ low-density lipoprotein cholesterol;
LVEF ⫽ left ventricular ejection fraction; RCA ⫽ right coronary artery.
wave in leads V5, V6, and I.10 Laboratory data for the serum
levels of total, high-density lipoprotein, and low-density
lipoprotein cholesterol, triglycerides, and creatinine were
recorded for all patients. The left ventricle ejection fraction
was analyzed by echocardiography. To estimate the presence and extent of CAD, the coronary angiograms of all
patients were analyzed. Patients with no angiographic disease or irregularities in any of the epicardial coronary arteries were considered to have normal coronary arteries on
angiography. The severity of CAD was determined visually
by a single experienced observer, and CAD was defined as
a 50% reduction in the internal diameter of the left anterior
descending artery or right or circumflex coronary artery or
their primary branches. The extension of CAD was classified according to the standard method into 1-, 2-, or 3-vessel
disease and was estimated by calculation of the Gensini score.
The Gensini score was computed by assigning a severity score
to each coronary stenosis according to the degree of luminal
narrowing and its geographic importance.11
The Statistical Package for Social Sciences for Windows
(release 11.5, SPSS, Inc., Chicago, Illinois) was used for
statistical analysis. The categorical variables are expressed
as a percentage and were analyzed by chi-square statistics.
The continuous variables are expressed as means and were
analyzed by 1-way analysis of variance, with Tukey post
hoc testing when appropriate. A 2-tailed p value of ⱕ0.05
was considered significant.
The data of 51 patients with type 2 diabetes mellitus with
LBBB (group I, mean age 67 ⫾ 8 years, 65% women) were
compared with the data of 51 patients with diabetes but
without LBBB (group II, mean age 68 ⫾ 10 years, 61%
women) and with the data of 51 patients without diabetes
but with LBBB (group III, mean age 65 ⫾ 10 years, 61%
women). The serum triglyceride and total cholesterol levels
in group I (diabetes mellitus and LBBB) were significantly
higher than the levels in groups II and III (p ⬍0.001);
however, no significant difference was found in the highdensity lipoprotein and low-density lipoprotein cholesterol
levels among the 3 groups (p ⫽ NS). Hypertension was
more prevalent in group I than in group II or III. The body
mass index was higher in the diabetic patients (groups I
and II), but had no statistical importance (Table 1). The
serum creatinine level in group I (diabetes mellitus and
LBBB) was significantly higher than in group II or III
(p ⬍0.037).
The mean left ventricular ejection fraction in group I was
significantly lower than in groups II and III (p ⫽ 0.01).
Normal coronary arteries were more prevalent in the isolated LBBB group (55% in group III vs 45% in group II and
31% in group I). The prevalence and localization of 1-vessel
disease were not statistically different among the 3 groups
(Table 1). The prevalence of multivessel disease (2- or
3-vessel disease) was 49% in group I, 33% in group II, and
23% in group III. The Gensini angiographic score was
higher in group I than in groups II and III (p ⬍0.001).
Because statistically significant differences were found for
hypertension, hypertriglyceridemia, and hypercholesterolemia among the 3 groups, univariate analysis of variance
was performed, which revealed continued statistical significance for the Gensini score (p ⬍0.001).
•••
Patients with diabetes have a considerable risk of cardiovascular disease, and up to 80% of deaths within this group
of patients are from cardiovascular disease.12 Recent reports
have suggested that the presence of LBBB in patients with
type 2 diabetes mellitus may indicate worse left ventricular
systolic dysfunction compared with those without LBBB.9
This study, for the first time, has demonstrated that the
presence of complete LBBB in diabetic patients is unequivocally associated with more extensive CAD, with higher
prognostic risk scores.
1. Eschwege E, Simon D, Balkau B. The growing burden of diabetes
mellitus in world population. Int Diabetes Fed Bull 1997;42:14 –19.
2. Raman M, Nesto RW. Heart disease in diabetes mellitus. Endocrinol
Metab Clin North Am 1996;25:425– 438.
3. Shehadeh A, Regan TJ. Cardiac consequences of diabetes mellitus.
Clin Cardiol 1995;18:301–305.
4. Fahy GJ, Pinski SL, Miller DP, McCabe N, Pye C, Walsh MJ, Robinson K. Natural history of isolated bundle branch block. Am J Cardiol
1996;77:1185–1190.
Arrhythmias and Conduction Disturbances/LBBB in Diabetes Mellitus
5. Schneider JF, Thomas HE Jr, Sorlie P, Kreger BE, McNamara PM,
Kannel WB. Comparative features of newly acquired left and right
bundle branch block in the general population: the Framingham Study.
Am J Cardiol 1981;47:931–940.
6. Smith RF, Jackson DH, Harthorne JW, Sanders CA. Acquired bundle
branch block in a healthy population. Am Heart J 1970;80:746 –751.
7. Beach TB, Gracey JG, Peter RH, Grunenwald PW. Benign left bundlebranch block. Ann Intern Med 1969;70:269 –276.
8. Freedman RA, Alderman EL, Sheffield LT, Saporito M, Fisher LD.
Bundle branch block in patients with chronic coronary artery disease:
angiographic correlates and prognostic significance. J Am Coll Cardiol
1987;10:73– 80.
9. Guzman E, Singh N, Khan IA, Niarchos AP, Verghese C, Saponieri C,
Singh HK, Gowda RM, Vasavada BC, Cohen RA. Left bundle branch
859
block in type 2 diabetes mellitus: a sign of advanced cardiovascular
involvement. Ann Noninvasive Electrocardiol 2004;9:362–365.
10. Willems JL, Robles de Medina EO, Bernard R, Coumel P, Fisch C,
Krikler D, Mazur NA, Meijler FL, Mogensen L, Moret P, for the
World Health Organizational/International Society and Federation for
Cardiology Task Force Ad Hoc. Criteria for intraventricular conduction disturbances and pre-excitation. J Am Coll Cardiol 1985;5:1261–
1275.
11. Gensini GG. A more meaningful scoring system for determining the
severity of coronary heart disease. Am J Cardiol 1983;51:606 – 607.
12. Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality
from coronary heart disease in subjects with type 2 diabetes and in
nondiabetic subjects with and without myocardial infarction. N Engl
J Med 1998;339:229 –234.