Mice Deficient in Mac-1 (CD11b/CD18) Are Less Susceptible
to Cerebral Ischemia/Reperfusion Injury
Sulpicio G. Soriano, MD; Angela Coxon, PhD; Yanming F. Wang, MD; Matthew P. Frosch, MD, PhD;
Stuart A. Lipton, MD, PhD; Paul R. Hickey, MD; Tanya N. Mayadas, PhD
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Background and Purpose—Macrophage-1 antigen (Mac-1) (CD11b/CD18), a leukocyte b2 integrin, facilitates neutrophil
adhesion, transendothelial migration, phagocytosis, and respiratory burst, all of which may mediate reperfusion-induced
injury to ischemic brain tissue in conditions such as stroke. To determine the role of Mac-1 during ischemia and
reperfusion in the brain, we analyzed the effect of transient focal cerebral ischemia in mice genetically engineered with
a specific deficiency in Mac-1.
Methods—Transient focal ischemia/reperfusion was induced by occluding the left middle cerebral artery for 3 hours
followed by a 21-hour reperfusion period in Mac-1– deficient (n512) and wild-type (n511) mice. Regional cerebral
blood flow was determined with a laser-Doppler flowmeter. Brain sections were stained with 2% 2,3,5-triphenyltetrazolium chloride to determine the infarct volume. Neutrophil accumulation was determined by staining the brain sections
with dichloroacetate esterase to identify neutrophils.
Results—Compared with the wild-type cohort, Mac-1– deficient mice had a 26% reduction in infarction volume (P,0.05).
This was associated with a 50%, but statistically insignificant, reduction in the number of extravasated neutrophils in
the infarcted areas of the brains in the mutant mice. There were no differences in regional cerebral blood flow between
the 2 groups.
Conclusions—Mac-1 deficiency reduces neutrophil infiltration and cerebral cell death after transient focal cerebral
ischemia. This finding may be related to a reduction in neutrophil extravasation in Mac-1– deficient mice. (Stroke.
1999;30:134-139.)
Key Words: cell adhesion molecules n cerebral ischemia, transient n macrophage-1 antigen n reperfusion injury n stroke
A
ccumulating evidence suggests that transient cerebral
ischemia elicits an inflammatory response that is augmented by reperfusion. Leukocyte infiltration has been well
documented after cerebral ischemia and reperfusion1 and is
known to mediate local tissue damage and alterations in
microvascular perfusion. Leukocyte adhesion and extravasation are controlled by adhesion molecules present on leukocytes and endothelial cells. The leukocyte adhesion receptor
macrophage-1 antigen (Mac-1) (CD11b/CD18) is a b2 integrin that is constitutively expressed on the surface of leukocytes but is transformed to an active conformation, as well as
quantitatively upregulated on the cell surface, by inflammatory mediators.2 Mac-1 mediates firm adhesion of neutrophils
to the blood vessel by binding to its endothelial ligand,
intercellular adhesion molecule-1 (ICAM-1).3 It has several
other ligands, including complement, and plays a pivotal role
in neutrophil chemotaxis, aggregation, phagocytosis, and
respiratory burst.2,4
See Editorial Comment, page 139
A functional blocking monoclonal antibody to Mac-1
reduced infarct volume after transient focal ischemia.5,6
However, administration of this antibody also led to partial
peripheral white blood cell depletion. Treatment with an
antibody to the CD18 subunit has yielded controversial
results; in a feline model, the antibody did not alter cerebral
blood flow or infarct volume,7 whereas in a primate model, it
improved microvascular patency after cerebral ischemia/
reperfusion.8 Antibody-antigen interactions can lead to complex responses, including triggering of signal transduction
events and incomplete inactivation of functional binding sites
on the target molecule. Therefore, knockout mice are being
used as an additional in vivo approach to understand the role
of leukocyte adhesion receptors in the pathogenesis of stroke.
For example, ICAM-1– deficient mice subjected to transient
focal cerebral ischemia followed by reperfusion manifested
Received September 18, 1998; final revision received October 23, 1998; accepted October 23, 1998.
From the Department of Anesthesia, Children’s Hospital, Boston (S.G.S., P.R.H.), and CNS Research Institute and Department of Neurosurgery
(Y.F.W., S.A.L.) and Department of Pathology (A.C., M.P.F., T.M.N.), Brigham and Women’s Hospital, Harvard Medical School, Boston, Mass. Dr
Soriano and Dr Coxon contributed equally to this work.
Correspondence to Sulpicio G. Soriano, MD, Department of Anesthesia, Children’s Hospital, 300 Longwood Ave, Boston, MA 02115. E-mail
soriano@A1.tch.harvard.edu
© 1999 American Heart Association, Inc.
Stroke is available at http://www.strokeaha.org
134
Soriano et al
significantly smaller cerebral injury compared with wild-type
counterparts that were similarly treated.9,10
ICAM-1 is a well-recognized ligand for Mac-1.3,11 Mice
deficient in Mac-1 exhibited a defect in intravascular leukocyte adhesion after leukotriene B4 administration in a cremaster muscle preparation.12 In addition, after acute glomerulonephritis, Fc g R-dependent glomerular neutrophil
accumulation and complement-dependent proteinuria were
significantly reduced in these mice.13 Furthermore, Mac-1–
deficient neutrophils were unable to phagocytose
complement-opsonized particles and displayed a 60% impairment in oxidative burst.12 To test the hypothesis that a
deficiency in Mac-1 leads to a reduction in neutrophil
accumulation and infarct size after stroke, we measured the
extent of histopathological damage after transient cerebral
ischemia/reperfusion in Mac-1– deficient and wild-type mice.
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Materials and Methods
Animals and Induction of Transient Focal
Cerebral Ischemia
Mac-1– deficient mice (Mac-1 2/2) generated by gene targeting12
and wild-type mice (Mac-1 1/1) were bred and maintained in a
virus antibody–free facility at the Longwood Medical Research
Center of the Harvard Medical School. Mac-1– deficient and wildtype mice were of a mixed C57Bl/129Sv strain and were generated
as follows. Wild-type and Mac-1– deficient progeny were obtained
from the breeding of mice heterozygous for Mac-1. The wild-type
mice were also bred to each other to produce wild-type mice, and the
Mac-1– deficient mice were bred to produce Mac-1– deficient mice,
avoiding brother-sister matings. To prevent the 2 genotypes from
straying in their background genes, new breedings with mice derived
from heterozygous breedings were routinely set up. Mice from both
the heterozygous and homozygous breedings were used in the
experiments with similar results. These mice were maintained in a
12-hour light/dark cycle and had access to water and food at libitum.
Only 8-week old male mice were used for the study.
With approval of the institutional review board, mice weighing 25
to 30 g were anesthetized with isoflurane (1% to 2%) and a 2:1
mixture of nitrous oxide and oxygen by nose cone. Body temperature
was maintained by a water blanket, which was servo controlled at
3761°C by a rectal temperature probe. The right femoral artery was
cannulated in 3 wild-type and 3 Mac-1– deficient mice to determine
arterial blood pressure and sample arterial blood gas and glucose.
Arterial blood pressure was recorded before ischemia, during ischemia, and at reperfusion continuously with a computerized data
acquisition system (MacLabs 8s, ADInstruments). Arterial blood
gases and glucose were measured 10 minutes after reperfusion with
a blood gas and glucose analyzer (Stat Profile Ultra C, Nova
Biomedical). The left internal carotid artery was exposed through a
midline cervical incision under a dissecting microscope. All of the
extracranial branches of the left internal carotid artery were ligated.
A 6.0 monofilament nylon suture (Ethicon Inc) with a flame-rounded
tip coated with silicon was inserted into the lumen of the external
carotid artery and advanced distally into the internal carotid artery
'10 mm to the base of the middle cerebral artery (MCA).9,14,15
Anesthesia was maintained for the duration of the surgical procedure, which typically lasted 30 minutes. Ischemia was induced for 3
hours by leaving the tip of the filament at the origin of the MCA.
After the 3-hour occlusion period, the mice were reanesthetized.
Reperfusion was accomplished by withdrawing the intraluminal
filament.
Assessment of Cerebral Blood Flow
To determine changes in regional cerebral blood flow (rCBF), we
used a laser-Doppler flowmeter (BPM, Vasamedics) with a 0.7-mm
probe (P433, Vasamedics). The analog signal of the laser Doppler
January 1999
135
was collected with a computerized data acquisition system (MacLab
8s, ADInstruments, on a MacIntosh LC 475 computer). The skull
was exposed through a midline sagittal incision, and the probe tip
was placed on the skull surface 3 mm lateral to midline and 2 mm
posterior to the bregma. These cortical coordinates represented the
ischemic core of the infarct. rCBF was recorded in wild-type (n53)
and Mac-1– deficient mice (n53) over 15 minutes, before and
immediately after middle cerebral artery occlusion (MCAO) and
before and immediately after reperfusion, as previously described.9,16 Data were presented as percentage of the preischemic
rCBF.
Neurological Assessment
To ensure successful placement of the intraluminal suture, the
functional effects of ischemia were assessed by a masked observer.
We evaluated the severity of the neurological deficit by using a
modified 5-point scale (0, no deficit; 1, failure to extend right paw;
2, circling to the right; 3, falling to the right; and 4, unable to walk
spontaneously).17
Detection and Quantification of
Cerebral Infarction
After the reperfusion period, the mice were killed with a lethal dose
of pentobarbital (150 mg/kg IP). The brains were immediately
removed, and 1.5-mm coronal sections were cut with a tissue cutter.
The brain sections were stained with 2% 2,3,5-triphenyltetrazolium
chloride (TTC) in phosphate buffer at 37°C for 30 minutes.18 These
sections were fixed in 4% paraformaldehyde in phosphate buffer for
digital photography. The digitized image of each brain section and
the infarcted area was measured by a masked observer using a
computerized image analysis program (SigmaScan, Jandel Corp). To
minimize the effect of brain edema, calculation of the infarcted
volume was indirectly determined by subtracting the volume of the
noninfarcted ipsilateral hemisphere (left) from the contralateral
hemisphere (right), as previously described.19,20
Histological Examination for
Leukocyte Accumulation
A cohort of wild-type and Mac-1– deficient mice were subjected to
the same ischemia and reperfusion protocol (n58 for each group).
Brain sections were fixed in 10% formaldehyde and embedded in
paraffin. A 5-mm section from the coronal slice 4.5 mm from the
frontal pole was subjected to reaction with dichloroacetate esterase to
identify extravasated neutrophils21 and counterstained with nuclear
fast red. To assess the neutrophil infiltrate, the masked observer then
counted the number of dichloroacetate esterase–positive cells in 10
high-powered fields (340). The fields for observation were selected
to assess neutrophils present only in the periphery of the infarct. On
sections with clusters of neutrophils, the observer started at the edge
of the infarct, where the highest numbers of neutrophils were present,
and the neutrophils were then followed in 10 nonoverlapping
contiguous fields. On sections with low numbers of neutrophils, the
observer started at the recognizable edge of the infarct and tracked
the neutrophils along the edge of the infarct. In all cases, only
neutrophils in the parenchyma, and not within blood vessels, were
counted.
Statistical Analysis
Infarct volumes and neutrophil counts were compared by an unpaired
t test. Data were reported as mean6SEM. Mortality rates were
compared with Fisher’s exact test. A P value ,0.05 was accepted as
statistically significant.
Results
Mac-1 Deficiency Partially Protects Against
Cerebral Ischemia/Reperfusion Injury
To determine the role of Mac-1 in infarct development, we
subjected Mac-1– deficient mice and wild-type cohorts to 3
136
Mac-1 Deficiency Reduces Cerebral Ischemia/Reperfusion Injury
TABLE 2. Arterial Blood Gases and Glucose Determined After
Reperfusion in Wild-Type and Mac-1–Deficient Mice
Arterial Blood Gas Analysis
Genotype
Arterial pH
PaCO2, mm Hg
PaO2, mm Hg
Glucose, mg/dL
1/1
7.2660.03
4061.6
203639
15262
2/2
7.2960.05
51.567.3
177611
15462
Values are mean6SEM; n53 for each genotype. There were no differences
in arterial blood gases and glucose between the genotypes.
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
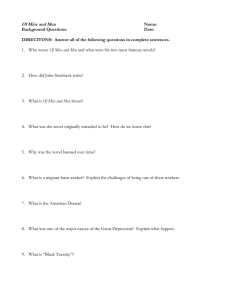
Figure 1. rCBF after ischemia/reperfusion. rCBF was measured
by laser-Doppler flowmetry over the ischemic core of the left
MCA region in wild-type (1/1) and Mac-1– deficient mice (2/2)
before, during 3 hours of MCAO, immediately after reperfusion,
and every 5 minutes. The preischemic rCBF was assigned a
value of 100%. Subsequent values are presented as a percentage of the preischemic rCBF (mean6SEM, n53 for each
genotype).
hours of focal cerebral ischemia and 21 hours of reperfusion.
Mortality values, as represented by the dead/alive ratios, of
the wild-type and Mac-1– deficient mice during this 24-hour
experimental period were 3/14 and 1/13, respectively. These
findings were not significantly different. All mice had at least
a grade 3 deficit after MCAO, indicating successful placement of the intraluminal suture. Gross examination of the
surface cerebral circulation after carbon black injection demonstrated that the vascular pattern in Mac-1– deficient mice
was indistinguishable from that in their wild-type cohorts
(data not shown). Therefore, differences in vasculature do not
explain differential sensitivity of the 2 genotypes to stroke
damage. rCBF was diminished during the period of MCAO
and was restored, albeit diminished, similarly in mutants and
wild-types (Figure 1). This suggests that postreperfusion
rCBF was not affected by Mac-1 deficiency. Furthermore,
there was no difference in arterial blood pressure, arterial
blood gases, and glucose between the genotypes (Tables 1
and 2). Tissues from wild-type (n511) and Mac-1– deficient
(n512) mice were subsequently analyzed for tissue injury.
Infarct size was measured on serial cerebral sections stained
with TTC. The infarct volume in the wild-type mice was
79.464.3 mm3, while that in the Mac-1– deficient mice was
58.965.8 mm3, which translates to a 26% reduction in tissue
injury in the Mac-1– deficient mice (Figure 2).
Mac-1 Deficiency and Neutrophil Accumulation
Neutrophil accumulation in the periphery of the infarct after
ischemia and 21 hours of reperfusion was assessed in brain
TABLE 1. Mean Arterial Blood Pressure Before, During, and
After MCAO in Wild-Type and Mac-1–Deficient Mice
Mean Arterial Pressure, mm Hg
Genotype
Before Ischemia
Ischemia
After Reperfusion
1/1
10065
9867
91610
2/2
10566
10667
9866
Values are mean6SEM; n53 for each genotype. There was no difference in
mean arterial pressure between the genotypes.
coronal sections of Mac-1 null and wild-type mice. The
wild-type mice had a 2-fold increase in neutrophil accumulation compared with the Mac-1– deficient mice, but this was
not significant (Figure 3).
Discussion
This study demonstrates that Mac-1– deficient mice are less
susceptible to focal cerebral ischemia/reperfusion injury than
wild-type mice. We found that postreperfusion infarction
volumes and neutrophil infiltration were less in the Mac-1–
deficient mice, supporting the hypothesis that Mac-1 has a
role in mediating neutrophil extravasation and infarct
development.
There is evidence that early neutrophil influx follows an
ischemic insult and may contribute to ischemia-related neuronal damage.22 Neutrophils are recruited to tissues by
chemoattractants and adhesion molecules expressed by endothelial cells and are critically involved in mediating inflammatory injury to the brain parenchyma by liberation of
reactive oxygen species, proteases, eicosanoids, and cytokine.23 Neutrophil accumulation in cerebral infarcts of patients has been associated with poor clinical outcomes.24 A
deficiency in the leukocyte adhesion receptor ICAM-1 led to
a .75% reduction in infarct volume in the ischemia/reperfusion model described here9,10 and was associated with a 40%
to 80% reduction in tissue neutrophil accumulation in the
infarcted area. A 26% reduction in infarct volume in Mac-1–
deficient mice was associated with a 50%, although not
statistically significant, reduction in the number of neutrophils present in the periphery of the infarcted area. Alternatively, it is possible that the interaction of ICAM-1 and
lymphocyte function–associated antigen-1 (LFA-1), a sister
b2 integrin of Mac-1, may be important in ICAM-1–mediated
neutrophil accumulation and tissue injury.4
Since Mac-1 mediates neutrophil adhesion to the endothelial surface, reperfusion would increase the likelihood of
infiltration of these neutrophils into the affected brain parenchyma. However, permanent ischemia also results in neutrophil adhesion to microvessels and extravasation after occlusion of the MCA.22,25 Although anti–Mac-1 monoclonal
antibodies decreased tissue injury after transient focal cerebral ischemia, Garcia et al26 demonstrated that similar treatment did not decrease the number of neutrophils or infarct
volume after permanent MCAO. Most human strokes represent transient rather than permanent occlusion. Therefore, we
believe that transient MCAO with reperfusion is the most
pathophysiologically relevant model for this condition.
Soriano et al
January 1999
137
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Figure 2. Effect of Mac-1 on infarct volume. A representative reddish TTC staining of the midcoronal section from wild-type (1/1,
n511) (a) and Mac-1– deficient mice (2/2, n512) (b) delineates viable tissue (bar51.0 mm). c, Infarct volume of wild-type (1/1) and
Mac-1– deficient mice (2/2) after 3 hours of MCAO and 21 hours of reperfusion. d, Infarct area of each coronal section for wild-type
(1/1) and Mac-1– deficient (2/2) mice (mean6SEM). *P,0.05.
ICAM-1– deficient mice have smaller infarct volumes than
the Mac-1– deficient or neutropenic mice.10 Thus, ICAM-1
deficiency may confer protection by mechanisms other than
the reduction of neutrophil accumulation in tissues. It is
known that infarcts are initiated during the ischemic period
because of deprivation of oxygen, and therefore any mechanism that reduces the ischemic time, such as a decrease in the
no-reflow phenomenon during the reperfusion period, would
be protective. In fact, ICAM-1– deficient mice and
neutrophil-depleted animals were shown to have an increase
in rCBF compared with the contralateral (nonischemic) hemisphere after a 45-minute period of cerebral ischemia.10 The
lack of no-reflow may be the result of a reduction in
neutrophil-neutrophil or neutrophil-platelet interactions with
subsequent vessel occlusion. In our study the ischemic period
was 4-fold longer, and we measured rCBF in the ischemic
hemisphere and compared subsequent values with the preischemic rCBF. The rCBF during the MCAO was 5% to 10%
of the preischemic values, and restoration of flow resulted in
rCBF equal to 50% of baseline in both genotypes (Mac-1–
deficient and wild-type). This finding is consistent with
previous studies using a 3-hour ischemic period.9,14 The 50%
decrease from the baseline preischemic rCBF may be due to
a combination of perivascular edema and non–Mac-1–mediated microvascular plugging. This prolonged period of ischemia can lead to perivascular edema, which would result in
external compression of blood vessels27 and a subsequent
decrease in rCBF compared with preischemic values. Therefore, we would expect some baseline tissue injury due to
reduced perfusion of ischemic tissue in both genotypes.
Furthermore, microvascular plugging occurs during reperfusion, and relevant receptors in this phenomenon may be
ICAM-1 and LFA-1, a b2 integrin present on both neutrophils and platelets.28,29 Differences in tissue injury and
neutrophil infiltration between wild-type and Mac-1– deficient mice are most probably due to events beyond microvascular plugging, since rCBFs were comparable during both
the ischemic and reperfusion periods.
In both the ICAM-1 and Mac-1– deficient mice, the effects
of reperfusion-induced injury at time points .24 hours after
the onset of ischemia were not assessed. It is possible that the
lack of Mac-1 or ICAM-1 may only delay the conversion of
the ischemic lesion to infarction. On the other hand, leukocyte subtypes differ at 1 and 7 days after the onset of MCAO,
138
Mac-1 Deficiency Reduces Cerebral Ischemia/Reperfusion Injury
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Figure 3. Effect of Mac-1 on neutrophil accumulation after transient focal cerebral ischemia. Extravascular neutrophils (arrows) in the
brain parenchyma were identified in coronal sections stained with dichloroacetate esterase and nuclear fast red. Representative sections from wild-type mice (a) and Mac-1– deficient mice (b) are shown. Bars550 mm. c, Number of neutrophils in the ischemic hemisphere in wild-type (1/1) and Mac-1– deficient mice (2/2) (mean6SEM; n58 for each genotype).
with neutrophil predominance in the former and monocytes
and macrophages in the latter.25 Both monocytes and activated microglia residing in the brain may be play a role in the
progression of cerebral ischemic injury.30 Notably, Mac-1
and ICAM-1 are expressed and upregulated on activated
microglia31–33 and may play a role in microglia- and
monocyte-mediated maturation of ischemic lesions. Therefore, the role of the microglia in the development of stroke
injury is a fertile area for further investigation. In summary,
our data suggest an important role for Mac-1 in the evolution
of ischemic injury after transient cerebral ischemia. Our
findings demonstrate that selective inhibition of Mac-1 is a
promising therapeutic option for the acute treatment of
transient focal cerebral ischemia.
Acknowledgments
This study was supported by the William F. Milton Fund and
William Randolph Hearst Fund (Dr Soriano), National Institutes of
Health grant NS33296 (Dr Mayadas), and a postdoctoral fellowship
from the Lady Tata Memorial Trust (Dr Coxon). The authors wish to
thank Michael Goodman (Department of Pathology, Brigham and
Women’s Hospital, Boston, Mass) for his technical assistance.
References
1. Kochanek PM, Hallenbeck JM. Polymorphonuclear leukocytes and
monocytes/macrophages in the pathogenesis of cerebral ischemia and
stroke. Stroke. 1992;23:1367–1379.
2. Arnaout MA. Structure and function of the leukocyte adhesion molecules
CD11/CD18. Blood. 1990;75:1037–1050.
3. Diamond MS, Springer TA. A subpopulation of Mac-1 (CD11b/CD18)
molecules mediates neutrophil adhesion to ICAM-1 and fibrinogen. J Cell
Biol. 1993;120:545–556.
4. Springer TA. Traffic signals on endothelium for lymphocyte recirculation
and leukocyte emigration. Annu Rev Physiol. 1995;57:827– 872.
5. Chopp M, Zhang RL, Chen H, Li Y, Jiang N, Rusche JR. Postischemic
administration of an anti–Mac-1 antibody reduces ischemic cell damage
after transient middle cerebral artery occlusion in rats. Stroke. 1994;25:
869 – 876.
6. Chen H, Chopp M, Zhang RL, Bodzin G, Chen Q, Rusche JR, Todd RF.
Anti-CD11b monoclonal antibody reduces ischemic cell damage after
transient focal cerebral ischemia. Ann Neurol. 1994;35:458 – 463.
7. Takeshima R, Kirsch JR, Koehler RC, Gomoll AW, Traystman RJ.
Monoclonal leukocyte antibody does not decrease the injury of transient
focal cerebral ischemia in cats. Stroke. 1992;23:247–252.
8. Mori E, del Zoppo GJ, Chambers JD, Copeland BR, Arfors KE. Inhibition
of polymorphonuclear leukocyte adherence suppresses no-reflow after
focal cerebral ischemia in baboons. Stroke. 1992;23:712–718.
9. Soriano SG, Lipton SA, Wang YF, Xiao M, Springer TA,
Gutierrez-Ramos JC, Hickey PR. Intercellular adhesion molecule-1
(ICAM-1) deficient mice are less susceptible to cerebral ischemiareperfusion injury. Ann Neurol. 1996;39:295–301.
Soriano et al
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
10. Connolly ES, Winfree CJ, Springer TA, Naka Y, Liao H, Yan SD, Stern
DM, Solomon RA, Gutierrez-Ramos JC, Pinsky DJ. Cerebral protection
in homozygous null ICAM-1 mice after middle cerebral artery occlusion:
role of neutrophil adhesion in the pathogenesis of stroke. J Clin Invest.
1996;97:209 –216.
11. Diamond MS, Staunton DE, Marlin SD, Springer TA. Binding of the
integrin Mac-1 (CD11b/CD18) to the third immunoglobulin-like domain
of ICAM-1 (CD54) and its regulation by glycosylation. Cell. 1991;65:
961–971.
12. Coxon A, Rieu P, Barkalow FJ, Askari S, Sharpe AH, von Andrian UH,
Arnaout MA, Mayadas TN. A novel role for the b2 integrin CD11b/CD18
in neutrophil apoptosis: a homeostatic mechanism in inflammation.
Immunity. 1996;5:653– 666.
13. Tang T, Rosenkranz A, Assmann KJM, Goodman MJ, Gutierrez-Ramos
JC, Carroll MC, Cotran RS, Mayadas TN. A role for Mac-1
(CD11b/CD18) in immune complex-stimulated neutrophil function in
vivo: Mac-1 deficiency abrogates sustained Fcg receptor-dependent neutrophil adhesion and complement-dependent proteinuria in acute glomerulonephritis. J Exp Med. 1997;186:1853–1863.
14. Yang G, Chan PH, Chen J, Carlson E, Chen SF, Weinstein P, Epstein CJ,
Kamii H. Human copper-zinc superoxide dismutase transgenic mice are
highly resistant to reperfusion injury after focal cerebral ischemia. Stroke.
1994;25:165–170.
15. Huang Z, Huang PL, Panahian N, Dalkara T, Fishman MC, Moskowitz
MA. Effects of cerebral ischemia in mice deficient in neuronal nitric
oxide synthase. Science. 1994;265:1883–1885.
16. Wang YF, Tsirka SE, Strickland S, Steig PE, Soriano SG, Lipton SA.
Tissue plasminogen activator (tPA) increases neuronal damage after focal
cerebral ischemia in wild-type and tPA-deficient mice. Nat Med. 1998;
4:228 –231.
17. Bederson JB, Pitts LH, Tsuiji M. Rat middle cerebral artery occlusion:
evaluation of the model and development of a neurologic examination.
Stroke. 1986;17:472– 476.
18. Bederson JB, Pitts LH, Germano SM, Nishimura MC, Davis RL, Bartkowski
HM. Evaluation of 2,3,5-triphehyltetrazolium chloride as a stain for detection
and quantification of experimental cerebral infarction in rats. Stroke. 1986;
17:1304–1308.
19. Swanson RA, Morton MT, Tsao-Wu G, Savalos RA, Davidson C, Sharp
FR. A semiautomated method for measuring brain infarct volume.
J Cereb Blood Flow Metab. 1990;10:290 –293.
January 1999
139
20. Lin T, He YY, Wu G, Khan M, Hsu CY. The effect of brain edema on
infarct volume in focal cerebral ischemia model in rats. Stroke. 1993;24:
117–121.
21. Yam LT, Li CY, Crosby WH. Cytochemical identification of monocytes
and granulocytes. Am J Clin Pathol. 1971;55:283–290.
22. Zhang RL, Chopp M, Chen H, Garcia JH. Temporal profile of ischemic
tissue damage, neutrophil response, and vascular plugging following
permanent and transient (2H) middle cerebral artery occlusion. J Neurol
Sci. 1994;125:3–10.
23. Barone FC, Schmidt DB, Hillegass LM, Price WJ, White RF, Feuerstein
GZ, Clark RK, Lee EV, Griswold DE, Sarau HM. Reperfusion increases
leukotriene B4 receptor binding in rat focal ischemia. Stroke. 1992;23:
1347–1348.
24. Akopov SE, Simonian NA, Grigorian GS. Dynamics of polymorphonuclear leukocyte accumulation in acute cerebral infarction and
their correlation with brain tissue damage. Stroke. 1996;27:1739 –1743.
25. Garcia JH, Liu KF, Yoshida Y, Lian J, Chen S, del Zoppo GJ. Influx of
leukocytes and platelets in an evolving brain infarct (Wistar rat). Am J
Pathol. 1994;144:188 –199.
26. Garcia JH, Liu KF, Bree MP. Effects of CD11b/18 monoclonal antibody
on rats with permanent middle cerebral artery occlusion. Am J Pathol.
1996;148:241–248.
27. Garcia JH. Time course of cerebral blood flow and histological outcome
after focal cerebral ischemia in rats. Stroke. 1992;23:1143–1144.
28. McCaffery PJ, Berridge MV. Expression of the leukocyte functional
molecule (LFA-1) on mouse platelets. J Clin Invest. 1986;67:1757–1764.
29. Weber C, Springer TA. Neutrophil accumulation on activated, surfaceadherent platelets in flow is mediated by interactions of Mac-1 with
fibrinogen bound to aIIbb3 and stimulated by platelet-activating factor.
J Clin Invest. 1997;100:2085–2093.
30. Moore S, Thanos S. The concept of microglia in relation to central
nervous system disease and regeneration. Prog Neurobiol. 1996;48:
441– 460.
31. Perry VH, Hume DA, Gordon S. Immunohistochemical localization of
macrophages and microglia in the adult and developing mouse brain.
Neuroscience. 1985;15:313–326.
32. Akiyama H, McGeer PL. Brain microglia constitutively express b-2
integrins. J Neuroimmunol. 1990;30:81–93.
33. Shrikant P, Weber E, Jilling T, Benveniste EN. Intercellular adhesion
molecule-1 gene expression by glial cells. J Immunol. 1995;155:
1489 –1501.
Editorial Comment
Inflammatory response and leukocyte infiltration after cerebral ischemia have been known to play key roles in ischemic
brain injury, particularly during the reperfusion phase. Previous experimental approaches used chemical methods to
produce leukopenia or to use selective antibodies specific for
adhesion molecules that are associated with the binding of
leukocytes to endothelial cells. These approaches may have
unwarranted side effects and toxicity. One current experimental strategy to prove the principle of the involvement of
leukocyte infiltration is to use animals that lack the expression of the key molecule involved in the binding process
between leukocytes and endothelium.
Using this unique approach, Soriano and colleagues now
provide strong evidence that the ischemic infarction is significantly reduced in mice deficient in Mac-1 (CD11b/CD18),
an adhesion molecule that mediates adhesion of neutrophils
to ICAM-1, an endothelial ligand, after transient focal cerebral ischemia. The study appears to be carefully done, and the
findings are independent of the alteration of cerebral blood
flow but are closely related to the reduced infiltration of
neutrophils. Although the findings provide an impetus for
future pharmacological developments and therapeutic approaches in stroke research, the acute nature (ie 21 hours after
reperfusion) may preclude a definite conclusion as to whether
the neuroprotection in the mutant mice is long-lasting. Additional studies during the long reperfusion/recovery period
may be helpful to address this important issue.
Pak H. Chan, PhD, Guest Editor
Department of Neurosurgery
Stanford University
Palo Alto, California
Mice Deficient in Mac-1 (CD11b/CD18) Are Less Susceptible to Cerebral
Ischemia/Reperfusion Injury
Sulpicio G. Soriano, Angela Coxon, Yanming F. Wang, Matthew P. Frosch, Stuart A. Lipton,
Paul R. Hickey and Tanya N. Mayadas
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Stroke. 1999;30:134-139
doi: 10.1161/01.STR.30.1.134
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1999 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/30/1/134
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published
in Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click
Request Permissions in the middle column of the Web page under Services. Further information about this
process is available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/