Advance Online Publication
doi: 10.5761/atcs.oa.10.01584
Original
Article
Zero Mortality of Continuous Veno-venous
Hemodiafiltration with PMMA Hemofilter after
Pediatric Cardiac Surgery
Takashi Miyamoto, MD, PhD,1 Akihiro Yoshimoto, MD,1 Kazuhito Tatsu, MD,1
Kentaro Ikeda, MD,2 Yoichiro Ishii, MD,2 and Tomio Kobayashi, MD, PhD2
Objective: Continuous veno-venous hemodiafiltration (CVVH) is used as one of the modalities of continuous renal replacement therapy (CRRT) in pediatric intensive units. The aim of
our study was to investigate the use of CVVH in small children with acute renal failure
(ARF) after cardiac surgery.
Patient and Methods: Between June 2005 and June 2008, 7 patients who required dialysis
after pediatric cardiac surgery without ECMO underwent CVVH with polymethylmethacrylate membrane (PMMA) treatment. The definition of ARF was based on a 100% rise in
serum creatinine (Cr) concentration, oliguria. On the other hand, PMMA-CVVH was
weaned in patients with satisfactory urine output, stable biochemical markers of renal function and adequate fluid balance.
Results: All patients treated with PMMA-CVVH alone (4 boys, 3 girls) had a median age of
36 months and a median body weight of 11kg. The averaged established time from cardiac
operation to CVVH was 2.6 days. There was a significant decrease in the post-filter compared with pre-filter levels of BUN, Cr, potassium concentration. There were no significant
changes in systolic blood pressure, lactate level and CRP; however, it was unnecessary for all
patients to use epinephrine.
Conclusions: Continuous veno-venous hemodiafiltration with PMMA-CVVH without
ECMO achieved a surprisingly Zero mortality.
Kew words: continuous veno-venous hemodiafiltration, polymethylmethacrylate membrane, pediatric cardiac surgery
Introduction
The utilization of dialysis or continuous renal replace1
Department of Cardiovascular Surgery, Gunma Children’s
Medical Center, Shibukawa, Gunma, Japan
2
Department of Pediatric Cardiology, Gunma Children’s Medical
Center, Shibukawa, Gunma, Japan
Received: April 27, 2010; Accepted: July 22, 2010
Corresponding author: Takashi Miyamoto, MD, PhD. Department
of Cardiovascular Surgery, Gunma Children’s Medical Center,
779, Shimohakoda, Hokkitsu, Shibukawa, Gunma 377-0061, Japan
Email: yonomiyataka@msn.com
©2011 The Editorial Committee of Annals of Thoracic and
Cardiovascular Surgery. All rights reserved.
ment therapy (CRRT) in critically ill post-cardiosurgical
children with acute renal failure (ARF) ranges from 1%
to 17 % of cases.1–3) Continuous veno-venous hemodiafiltration (CVVH) is used as one of the modalities of CRRT
in pediatric intensive care units. ARF is still a frequent
complication following extensive pediatric cardiac surgery due to low cardiac output, massive hemolysis and
high fluid overload. In our collection of 7 children with
congenital heart disease requiring postoperative renal
replacement, CVVH without extracorporeal membrane
oxygenation (ECMO) achieved a surprisingly low mortality. The aim of our study was to investigate the use of
CVVH in small children with ARF after cardiac surgery.
1
Advance Online Publication
Miyamoto T, et al.
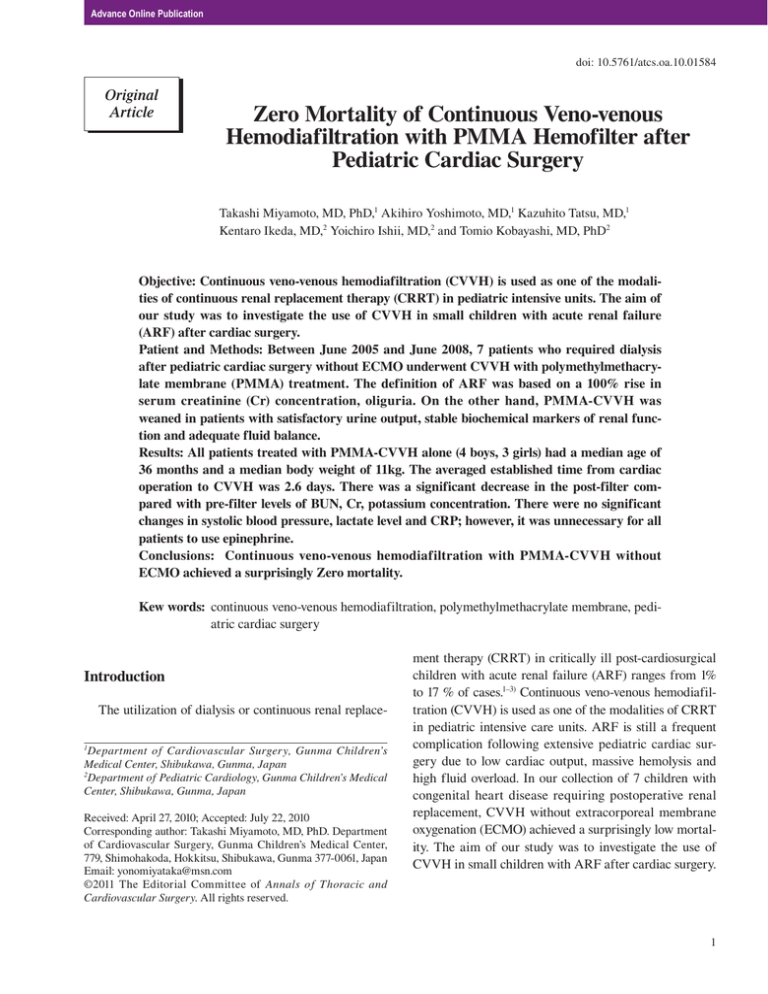
Table 1 Preoperative and operative variables
Procedure / Diagnosis
1. M-BTs / PA, hypo RV,
sinusoid communication
2.TCPC/ Ebstein’s anomaly
p-Starnes operation
3. MVR / MR, p-MVP
4. RVOTO/ PS, p-Truncus repair
5. MVR / MS, p- iAVSD
6. Central shunt with PA plasty, /
PS, p-mBTs for TGA (III)
7. ToF repair
Median Age
(m)
BW
(kg)
BSA
(m2)
CBP
(min)
ACC
(min)
Time from Ope. (days)
BAS
score
Survival/
Death
2
3.9
0.22
-
-
1
6.3
Survival
30
14.6
0.95
401
-
2
9
Survival
36
48
78
84
6.3
13.2
11
7.4
0.31
0.61
0.52
0.39
128
189
247
342
58
-
158
165
0
2
3
9
7.5
6.5
7.5
6.8
Survival
Survival
Survival
Survival
33
36 11.4
11
0.5 0.5
266
256
138
148
1
2
8
Survival
7.5 Mortality = 0 %
ACC, aortic cross clamp; BAS, basic Aristotle score; CPB, cardiopulmonary bypass; iAVSD, incomplete atrioventricular septal
defect; MR, mitral regurgitation; MS, mitral stenosis; MVP; mitral valve plasty; MVR, mitral valve replacement; M-BTs, modified
Blalock-Taussig Shunt; PA, pulmonary atresia; RV; right ventricule; RVOTO, right ventricular outflow tract obstruction; TCPC,
total cavopulmonary connection; ToF, tetralogy of Fallot
Methods
Retrospectively, we analyzed the clinical data of 7
children (< 15 y.o.) who required dialysis after cardiac
surgery without ECMO from June 2005 to June 2008.
The patient’s files were reviewed for cardio-respiratory
parameters and physiological variables at the start of
CVVHDF and during dialysis. The data sheet included
diagnosis, body weight, acid base status at the time
beginning CVVH, duration of therapy and inotropic support, and outcome. CVVH with polymethylmethacrylate
membrane (PMMA-CVVH) treatment was initiated in
cases of low cardiac output, coagulation disorders and
fluid overload. The definition of ARF was based on a
100% rise in serum creatinine concentration, oliguria
(less than 1 ml/kg·h). On the other hand, CVVH was
weaned in patients with satisfactory urine output (at least
2 ml/kg·h), stable biochemical markers of renal function
and adequate fluid balance. Survival outcome was based
on live discharge from hospital. Vascular access was provided by placing a 6-French (UK- cathe, Unitika Co. Ltd.,
Tokyo, Japan) or 8-French (Gam cathe, Gambro Co. Ltd.,
Tokyo, Japan) flexible double-lumen catheter in the
internal jugular vein or the femoral vein. A PMMA
membrane hemofilter (Hemofeel CH-0.3, Toray Medical
Co. Ltd., Tokyo, Japan) was placed in the blood circuit to
adsorb cytokines in the circulating blood (Fig. 1). Nafamostat mesilate (Futhan, Torii Phamaceutical Co. Ltd.,
Tokyo, Japan) was used as the anticoagulant, with the
dose adjusted to maintain an activated coagulation time
of 150–180s. All data are expressed as a median with a
2
full range. Statistical analysis was performed with nonparametric tests (Mann-Whitney U test and Wilcoxon
matched-pair test). A P-value of less than 0.05 was considered significant.
Results
The 7 patients treated with PMMA-CVVH alone (4
boys, 3 girls) had a median age of 36 months (2 months to 7
years) and a median body weight of 11kg (3.9kg to 14.6 kg).
Basic, clinical parameters are expressed in Table 1. The
cardiopulmonary bypass time ranged between 128 and
401 min (average time of 262 min) in 6 patients. The aorta
clumping time ranged between 128 and 401 min (average
time of 130 min) in 5 patients. The established time from
cardiac operation to CVVH between 0 and 9 days (average time of 2.6 days). Operating conditions for PMMACVVH were as follows: blood f low rate 42.9 ± 15
(ml/min·m2) (range: 21–68); dialysate flow rate, 11.3 ± 6.0
(ml/min·m2) (range: 5.4–22.7). The lifetime of the single
filter was 2.9 ± 2.0 days (range: 1.5–7.0). The overall duration of the procedure ranged from 2 to 38 days (average
value of 13.3 ± 11.9 days). All patients were ventilated and
used inotropic support at the commencement of CVVH.
Laboratory and clinical data of CVVH efficacy are summarized in Table 2. There was a significant decrease in
the post-filter compared with pre-filter levels of BUN,
creatine, potassium concentration in all patients. During
the CVVH treatment, there were no significant changes
in systolic blood pressure, lactate level and CRP; however,
it was unnecessary for all patients to use epinephrine.
Advance Online Publication
PMMA-CVVH after Pediatric Cardiac Surgery
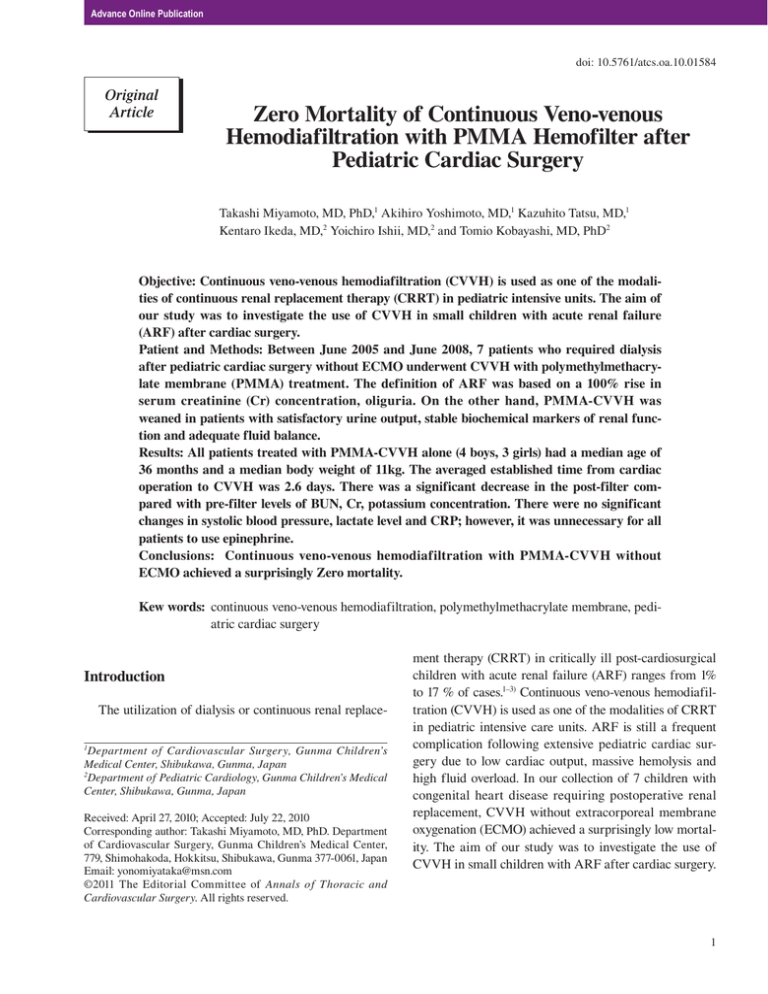
Table 2 Biochemical and clinical parameters before and after CVVH
Parameter
Systolic BP (mmHg)
Epinephrine (μg/kg・min)
Dopamine (μg/kg・min)
Hct (%)
Platelet count (× 104)
BUN (mmol/l)
Creatinine (μmol/l)
K (mmol/l)
CRP (mg/l)
Lactate (mmol/l)
Baseline 87.7 ± 20.2
0.5 ± 0.05
3.3 ± 1.9
42.5 ± 8.3
15.3 ± 9.5
54.2 ± 19.6
1.1 ± 0.3
5.7 ± 1.5
4.3 ± 4.4
2.4 ± 1.1
(50–107)
(0–13)
(0–5)
(31.2–55.6)
(4.9–27.2)
(27.8–77.8)
(0.6–1.5)
(3.9–8.2)
(0.1–10.4)
(0.7–4.0)
Post CVVHDF
90.1 ± 7.7 (80–103)
0.65
0
0.03
1.5 ± 1.4 (0–3)
0.07
37.1 ± 7.2 (29.2–50.5) 0.18
15.0 ± 4.6 (7.9–22.0) 0.74
13.0 ± 7.3 (4.3–26) < 0.01
0.4 ± 0.1 (0.2–0.6) < 0.01
3.8 ± 0.4 (3.2–4.5) < 0.01
2.1 ± 2.8 (0.1–7.4)
0.03
1.8 ± 1.3 (1–4.0)
0.99
BP, blood pressure; BUN, blood urea nitrogen; Cr, Creatinin; CRP, C-reactive protein; Hct.,
Hematocrit
They were all weaned from CVVH, and discharged from
the hospital.
Discussion
The incidence of acute ARF requiring dialysis treatment after cardiac surgery with cardio-pulmonary-bypass
(CPB) has been described to range between 1% and 17%
depending on the complexity of procedure, entry criteria,
and criteria for commencement of the dialysis treatment.
The survival rate of 21%–70 % in infants with acute renal
failure after cardiac surgery has been reported by several
authors.4–7) CVVH is still an uncommon treatment in my
PICU with an incidence of approximately 1%–2% per
year. In this cohort of 7 children requiring vasoactive
dosages, such as dopamine and epinephrine, PMMACVVH achieved a surprisingly high survival rate. The
most recently published reports described low cardiac
output, young age, low body weight, associated systemic
disorders, high fluid overload on starting hemofiltration,
pre-existing renal insufficiency or mechanical ventilation
before surgery as additional risk factors. Especially, it has
also been also suggested that higher fluid overload is
related to cytokines. The mechanisms of cytokine
removal by blood purification include convection, diffusion, and adsorption. The extent of cytokine removal by a
particular blood purification therapy (utilizing any of
these mechanisms alone or in combination with another)
principally depends on the material and shape of the
hemofilter/ hemodialyzer/ absorber used and the operating conditions employed. Cole et al. reported that CVVH
reduced the dose of norepinephrine required to maintain
circulation, a clinically useful effect.8) Cornejo et al. also
reported a decrease in the requirement of norepineph-
rine, an improved blood lactate level, and a high survival
rate, all due to improvement of hemodynamics in their
series.9) Nakada found that PMMA-CVVH exhibited a
higher capacity to remove cytokines than CHDF using a
hemofilter made of a different material.10) This high
capacity for cytokine removal of PMMA-CVVH was
principally ascribable to adsorption of cytokines to the
hemofilter membrane.
Furthermore, blood cytokine levels in critically ill
patients were significantly decreased after PMMACVVH treatment.11) They also examined the clinical efficacy of PMMA- CVVH in patients with septic shock
exhibiting extremely high blood IL-6 levels, and demonstrated a significant decrease in the blood IL-6 level during PMMA-CHDF treatment for 72 h. The high capacity
of PMMA-CVVH to remove cytokines thus resulted in
excellent therapeutic effects. His study also described
that a significant decrease in blood lactate level during
PMMA-CVVH. Ricci et al. reported that BNP levels
were significant reduced after three and four days from
PMMA-CVVH start.12) The present study examined the
CRP and Lactate level; however, there was no significant
difference in all the parameter’s levels after CVVH
removal. They were all weaned from CVVH, and the
many parameters such as BUN, creatine, potassium, CRP
and Lactate level returned to the normal range on discharge from the Hospital. Although the mechanism by
which improvement of hemodynamics occurs after
PMMA-CVVH initiation remains to be determined in
detail, it might entail removal of a cytokinemia13) (estimated by measurement of blood CRP level), dysoxygenation (estimated by measurement of blood lactate level)
and cardiac failure marker in pediatric patients (estimated
by measurement of BNP level).
3
Advance Online Publication
Miyamoto T, et al.
Conclusion
In conclusion, we analyzed the clinical date of 7 children requiring PMMA-CVVH after pediatric cardiac
surgery, retrospectively. They were all weaned from
CVVH, and the many parameters such as BUN, creatine,
potassium, CRP and Lactate level returned to the normal
range on discharge from the Hospital.
References
1)Sorof JM, Stromberg D, Brewer JE, Feltes TF, Fracer
CD. Early initiation of peritoneal dialysis after surgical repair of congenital heart disease. Pediatr Nephrol
1999; 13: 641-5.
2)Shaw NJ, Blockenbank JT, Dickinson DF, Wilson N,
Walker DR. Long-term outcome for children with
acute renal failure following cardiac surgery. Int J
Cardiol 1991; 31: 161-6.
3)Kist-van Holthe M, Echten JE, Goedvolk CA, Doornar
MBME. Acute renal insufficiency and renal replacement therapy after pediatric cardiopulmonary bypass
surgery. Pediatr Cardiol 2001; 22: 321-6.
4)Picca S, Prncipato F, Mazzera E, Corona R, Ferrigno L,
et al. Risk of acute renal failure after cardiopulmonary
bypass surgery in children: a retrospective 10-year
case—control study. Nephrol Dial Transplant 1995; 10:
630-6.
5)Baskin E, Saygili A, Harmanci K, Agras PI, Ozdemir
4
FN, et al. Acute renal failure and mortality after openheart surgery in infants. Ren Fail 2005; 27: 557-60.
6)Goldstein SL. Overview of pediatric renal replacement
therapy in acute renal failure. Artif Organs 2003; 27:
781-5.
7)Werner HA, Wensley DF, Lirenman DS, LeBlanc JG.
Peritoneal dialysis in children after cardiopulmonary
bypass. J Thorac Cardiovasc Surg 1997; 113: 64
8)Cole L, Bellomo R, Journois D, Davenport P, Baldwin I,
et al. High-volume haemofiltration in human septic
shock. Intensive Care Med 2001; 27: 978-86.
9)Cornejo R, Downey P, Castro R, Romero C, Regueira T,
et al. High-volume hemofiltration as salvage therapy
in severe hyperdynamic septic shock. Intensive Care
Med 2006; 32: 713-22.
10)Hirasawa H, Oda S, Shiga H, Matsuda K. Endotoxin
adsorption or hemodiafiltration in the treatment of
multiple organ failure. Curr. Opin Crit. Care 2000; 6:
421-5.
11)Matsuda K, Hirasawa H, Oda S, Shiga H, Nakanishi K.
Current topics on cytokine removal technologies. Ther.
Apher 2001; 5: 306-14.
12)Ricci Z, Garisto C, Morelli S, Chiara LD, Ronco C, et
al. Brain natriuretic peptide is removed by continuous
veno-venous hemofiltration in pediatric patients. Interact CardioVasc Thorac Surg 2009; 9: 33-36.
13)Matsuda K, Moriguchi T, Oda S, Hirasawa H. Efficacy
of continuous hemodiafiltration with a cytokineadsorbing hemofilter in the treatment of acute respiratory distress syndrome. Contrib Nephrol 2010; 166:
83-92.