Note that this statement should be read in conjunction with our
advertisement

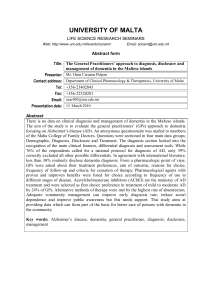
Note that this statement should be read in conjunction with our Timely Diagnosis policy statement. The Dementia Identification Specification is part of a broader set of payment mechanisms that make up a substantial element of the GP contract in England. The Quality and Outcomes Framework (QoF), incentivises quality care for people with dementia and other conditions such as diabetes or asthma and evidence suggests that it has had a broadly positive impact on the management of these conditions and quality of carei. However, the current QoF elements for dementia focus on the establishment of a register of patients and a review of care, rather than specifically on increases in the rate of diagnosis. The Enhanced Service Specification builds on the QoF and creates a specific incentive around diagnosis, with a view to achieving the targets set out in the Prime Minister’s dementia challenge to diagnose 2/3rds of all dementia patients by 2015. Estimates suggest that only half of people living with dementia receive a diagnosisii and for most people a timely diagnosis is important and can bring benefits, such as drugs or other treatments that can help with the symptoms and improve quality of life. Therefore an initiative designed to identify people with dementia is important. However, a focus on enhanced payments to GPs is only one approach to address this problem and these payments must in no way compromise the relationship of trust between patients and their GP. Importantly, given the particular difficulty of diagnosis of dementia, especially in the early stages of the condition, the incentive should not have the unintended consequence of misdiagnosis. It is incumbent on NHS England to monitor the Identification Scheme and ensure this does not happen. In order to meaningfully deliver timely diagnosis for everyone with dementia there are a number of other issues surrounding diagnosis that should also be addressed alongside any scheme to identify people with the condition. Firstly, there is no diagnostic tool that is 100% accurate and we therefore need to invest in further research and development to improve diagnostic tools as quickly as possible. Secondly, a diagnosis is dependent on the individual, often with support from their family, seeking out a diagnosis. More needs to be done to combat the stigma that still surrounds dementiaiii so that people feel comfortable seeking out a diagnosis. Thirdly, once a diagnosis is made, support is not always available locally and is often caught up in the grey area between health and social care provision. When a person is diagnosed with dementia they have a right to expect appropriate support to manage their condition. i Doran, T (2011) Effect of financial incentives on incentivised and non-incentivised clinical activities: longitudinal analysis of data from the UK Quality and Outcomes Framework. BMJ;347:f5939. Review: March 2015 www.alzheimersresearchuk.org Department of Health (2013) Dementia – a state of the nation report on dementia care and support in England. iii Bamford , S-M et al (eds) (2014) New perspectives and approaches to understanding dementia and stigma. ILC / MRC / Alzheimer’s Research UK / Alzheimer’s Society. ii Review: March 2015 www.alzheimersresearchuk.org