Alternative to Mental Hospital Treatment
advertisement

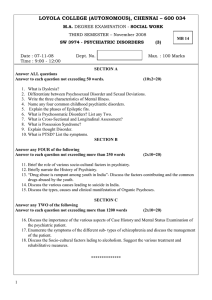
Alternative to Mental I. Conceptual Model, Treatment Program, Leonard I. Stein, MD, Mary Ann Test, PhD Gen Psychiatry 37:392-397, 1980) to the who suffered from illness were hospital¬ for a lifetime. There have since years and been continuous efforts to reduce the hospital stay and increase treatment in the community. These efforts have included the improvement of inpatient treatment to facili¬ tate early discharge,' shortening of the hospital stay,2-7 the substitution of day hospital treatment,8 the use of halfway houses for transitional living and continued treatment," and the development of community psychosocial rehabili¬ tation centers that utilize a rehabilitation model.10 The most radical form of community treatment involves attempts to develop a community-treatment alternative to the mental hospital. Three studies that randomly assigned patients from a sample in which the families accepted home treatment demonstrated that it is possible to treat patients at home rather than in the hospital."11 In all three studies, the home-treatment condition involved a relatively minimal therapeutic input. In the Pasamanick et al12 project, this consisted of visits by public health nurses to early 1950s, patients Prior chronically disabling psychiatric ized for often Accepted Treatment and Clinical Evaluation \s=b\ A conceptual model for the development of communitybased treatment programs for the chronically disabled psychiatric patient was developed, and the results of a controlled study and follow-up are reported. A community-treatment program that was based on the conceptual model was compared with conventional treatment (ie, progressive short-term hospitalization plus aftercare). The results have shown that use of the community program for 14 months greatly reduced the need to hospitalize patients and enhanced the community tenure and adjustment of the experimental patients. When the special programming was discontinued, many of the gains that were attained deteriorated, and use of the hospital rose sharply. The results suggest that community programming should be comprehensive and on- going. (Arch Hospital publication Sept 19, 1979. Department of Psychiatry, University of Wisconsin Medical School (Dr Stein), and the School of Social Work and the Institute for Research on Poverty (Dr Test), University of Wisconsin, Madison. Reprint requests to Department of Psychiatry, University of Wisconsin Medical Center, 600 Highland Ave, Madison, WI 53792 (Dr Stein). for From the Downloaded From: http://archpsyc.jamanetwork.com/ on 07/07/2012 patients' homes weekly or less often to provide drugs and supportive therapy. In the Langsley and Kaplan" study, the home treatment was family-crisis therapy that was aimed at teaching the patient ways of handling crises without hospitalization. In the Rittenhouse" project, the home treatment consisted of family-unit therapy as devel¬ oped by Satir." All three studies found that at least 77% of the experimental (E) patients could be kept out of the hospital continuously as long as the home treatment was in effect. Three controlled studies expanded the generality of the alternative to mental-hospital research to patients who did not have a stable home situation by demonstrating the possibility of treatment in a nonfamilial, residential set¬ ting. Irvin D. Rutman, PhD, (unpublished data, October 1971) diverted a random sample of nonassaultive or suicidal new admissions to Philadelphia State Hospital to a half¬ way-house-type setting where all patients who met the study-admission criteria were treated in a token-economy milieu. Mosher et al15·" reported on young, first-break schizophrenics at a residential setting that had a permis¬ sive, unstructured milieu that was staffed primarily by paraprofessionals who "guided" clients through their psy¬ choses, usually without medications. Only two of 30 patients over an average stay of 167 days had to be transferred to inpatient care. Polak and Kirby17 admitted patients in Denver to "crisis homes" run by private families who provided support and shelter for patients for several days to several weeks and who were aided by mental health workers who provided outreach services and consultation. Ten of the first 40 patients could not be so treated, but this percentage declined over time even though the sample was totally unselected. Three controlled studies compared day treatment with 24-hour in-hospital care for patients who sought admission to an in-hospital setting.1S-2" The Wilder et al2" study rejected a third of the patients randomly assigned to the day-treatment condition, whereas the other two studies only sampled from those patients "for whom both treat¬ ments were judged equally feasible." Thus, the daytreatment studies excluded a rather large and undefined group who were judged a priori to be "too ill" for the day-treatment setting. Of those treated, all but approxi¬ mately 20% were kept out of the hospital completely. The present study extended the quest for alternatives to mental hospital treatment for patients who suffer from chronically disabling psychiatric illness. First, we dealt with an unselected rather than a limited sample of patients who came to a state mental hospital for admission. Second, placed a major emphasis on improving psychosocial functioning by assertively working with patients who were living primarily independently rather than in parental homes or sheltered settings. The first section of the report describes a conceptual model, which is based on patients' needs, for the develop¬ ment of community-based treatment programs for the chronically disabled psychiatric patient. The second section reports the results of a controlled experiment that com¬ pared 14 months of a treatment program entitled "Train¬ ing in Community Living" (TCL) with short-term hospital¬ ization plus aftercare and describes a follow-up after the we discontinuation of TCL. CONCEPTUAL MODEL We contend that current community treatments do not effectively address certain factors that are required by patients. The absence of one or more of these factors leads to a tenuous community adjustment that keeps patients on the brink of rehospitalization. These requirements, which are derived from our clinical are as follows: ture,21 experience and the litera¬ 1. Material resources such as food, shelter, clothing, and medical Community-treatment programs must assume responsibility for helping the patient acquire these resources. 2. Coping skills to meet the demands of community life. These are skills we take for granted, such as using public transportation, preparing simple but nutritious meals, and budgeting money. Learning these skills should take place in vivo, where the patient will be needing and using them. care. 3. Motivation to persevere and remain involved with life. Our patients experience stress, and their motivation to remain in the community is easily eroded. A readily available system of support to help the patient solve real-life problems, feel that he is not alone, and feel that others are concerned is crucial. 4. Freedom from pathologically dependent relationships. We define a pathologically dependent relationship as one that inhibits personal growth, reenforees maladaptive behavior, and generates feelings of panic when its loss is threatened. Many have had a lifelong pathological dependence on families or institutions. Hos¬ pitalization can deepen this, and on discharge the patient is often returned to a highly conflictual family situation that leads to the revolving-door syndrome. To break that cycle and dependency, community programs must provide sufficient support to keep the patient involved in community life and to encourage growth toward greater autonomy. 5. Support and education of community members who are involved with patients. An important factor that influences patient behaviors and thus community tenure are the ways in which community members (family, law enforcement personnel, agency people, landlords, etc) relate to patients. Community programs must provide support and education to help these community members to relate in a manner that is both beneficial for the patient and acceptable to them. 6. A supportive system that assertively helps the patient with the previous five requirements. Chronically disabled patients are frequently passive, interpersonally anxious, and prone to develop severe psychiatric symptomatology. Such characteristics often lead these patients to fail to keep appointments and to "drop out" of treatment, particularly when they are becoming more sympto¬ matic. Hence, the program must be assertive, involve patients in their treatment, and be prepared to "go to" the patient to prevent dropout. It must also actively insure continuity of care among treatment agencies rather than assume that a patient will success¬ fully negotiate the often difficult pathways from one agency to another on his own. Downloaded From: http://archpsyc.jamanetwork.com/ on 07/07/2012 METHODS The experiment was designed to study the effects on patient functioning during a 14-month intensive community-treatment program and to evaluate patient functioning afterward when patients were transferred to traditional community programs. To accomplish this, the TCL model was rigorously evaluated by comparing it with a control (C) group that received progressive in-hospital treatment plus community aftercare. Subjects were assigned to the TCL approach for 14 months, after which they received no further input from the -unit staff. The latter few months of the 14-month period was used to gradually wean the patients and to integrate them into existing programs that in essence were the same programs that treated the C group. Subjects subjects sought admission to Mendota Mental Health Insti¬ tute for inpatient care and met the following three criteria: (1) were residents in Dane County, Wisconsin (Madison and the surrounding area), (2) were aged 18 to 62 years, and (3) had any diagnosis other than severe organic brain syndrome or primary All alcoholism. single, separated, or was approximately 31 years; and patients had accumulated a mean of 14.5 months in psychiatric institutions spread over a mean of five hospitalizations per subject before the current admission. Twenty percent came directly from another institution, and 14% came from sheltered living situations. Only 17% had spent no time in a hospital. The patients had a wide range of diagnoses, and approximately 50% were schizophrenic. The E and C groups did not differ significant¬ ly on demographic characteristics or on any of the major measure¬ ment instruments given at the time of admission, with the exception of the measure of self-esteem. Seventy-three percent divorced; 55% were were men; the either mean age Experimental Design randomly assigned by the admission office The subjects were staff. Control subjects were treated in the hospital for as long as necessary and then were linked with appropriate community agencies. Experimental subjects did not enter the hospital (except in rare instances), but instead received the TCL approach for 14 months before integration into existing community programs. Assessment data on all patients were gathered at the baseline (time of admission) and every four months for 28 months through face-to-face interviews by a research staff that operated inde¬ pendently of both clinical teams. Data on E subjects who were hospitalized are reported. No patients were excluded on the basis of severity of symptomatology or for any reason other than failure to meet the three specified admission criteria. Experimental Treatment The implementation of the TCL program has been described in detail.22 In brief, the program was implemented by a retrained mental-hospital ward staff who were transplanted to the commu¬ nity.23 Staff coverage was available 24 hours a day, seven days a week. Patient programs were individually tailored and were based primarily on an assessment of the patient's coping-skill deficits and requirements for community living. Most treatment took place in vivo: in patients' homes, neighborhoods, and places of work. More specifically, staff members on-the-scene in patients' homes and neighborhoods taught and assisted them in daily living activities such as laundry upkeep, shopping, cooking, restaurant use, grooming, budgeting, and use of transportation. In addition, patients were given sustained and intensive assistance in finding a job or sheltered workshop, and the staff then continued daily contact with patients and their supervisors or employers to help with on-the-job problem solving. Patients were aided in the constructive use of leisure and the development of effective social skills by the staff, who prodded and supported their involvement in recreation and social activities. Their effort was directed toward taking advantage of patients' strengths rather than focusing on their pathology. Providing support to patients, patients' families, and community members was a key function of the staff. The program was "assertive"; if a patient did not show up for work, a staff member immediately went to the patient's home to help with any problem that was interfering. Each patient's medical status was carefully monitored and treated. Medication was routinely used for schizophrenic and manic- were fully completed partially completed. interviews were The patients were immediately screened by a member of the hospital's treatment unit that served patients from Dane County, Wisconsin. They were usually (although not necessarily) admitted for progressive treatment that was aimed at preparation for return to the community. The Dane County Unit served as a stringent control since it had a high clinical staff-to-patient ratio (1:1) and offered a wide variety of services: inpatient care, partial hospitalization, and outpatient follow-up. The patients in the unit had a median length of stay of 17 days and made liberal use of Madison, Wis. least once, for a readmission rate of 58% in the first year compared with 6% of the E patients. Employment Status.-The E subjects spent significantly less time unemployed and significantly more time in sheltered employment than did the C subjects (Table 2). There was no significant difference between the groups in the percentage of time spent in competitive employment situations; however, the E subjects earned significantly more income through competitive employment than did the C subjects (Table 3). Assessment Instruments The baseline measures were as follows: (1) the Demographic Data Form was used to collect standard demographic data on life situation and economic variables; (2) the Short Clinical Rating Scale24 measured symptomatology; (3) the Community Adjust¬ ment Form measured the patient's living situation, time spent in institutions, employment record, leisure time activities, social relationships, quality of environment, and subjective satisfaction with life; and (4) the Rosenburg Self-Esteem Scale2' was a self-report measure of self-esteem. Measures taken at the subse¬ quent four-month intervals were the Short Clinical Rating Form, the Community Adjustment Form, and the Rosenburg Self- Leisure Time Table 1.—Mean Percentage of Data-Collection Periods Within-Treatment Phase, Living Situa¬ tion Institutional Living Situations* Posttreatment Phase, mo 24 20 16 28 E C E C E C E C E C E C E C <n= 62) (n= (n= 62) (n= 60) (n= <n= 59) <n= 57) (n= 59) (n= 57) (n= (n= 56) (n= 57) (n= 54) (n= 55) 11.63 22.88 4.71 16.61 13.13 26.56 3.34 13.94 14.91 27.52 6.45 19.52 15.37 7.18 28.62 21.20 12.46 25.47 60) 62) % 59) 9.56 11.32 23.85 24.33 1.59 5.35 t 21.20 20.62 1.38 3.99 0.97 4.89 1.12 3.19 0.12 0.44 0.54 1.85 0.78 3.83 0.81 2.17 0.87 3.92 1.29 4.23 0.25 1.04 1.44 6.66 0.24 0.84 0.61 2.50 0.48 1.46 0.39 SD X SD 4.42 15.39 3.53 10.65 5.14 19.96 5.27 15.45 3.47 14.37 6.06 21.24 4.30 20.18 3.38 14.68 5.10 20.91 3.21 14.54 5.23 20.56 3.71 15.23 2.62 14.07 5.20 19.68 19.58 30.45 11.80 28.57 20.02 31.56 12.65 29.78 16.78 31.04 12.66 28.51 16.91 29.46 13.06 14.10 31.02 Total SD Noninstitutionaj Total in Various X SD Medical dent Spent mo 12 Indepen- of leisure time activities showed that measured "contact with trusted friends" showed that E subjects had significantly more contact (P < .05) than did C subjects at the 12-month period. In addition, on a scale that measured "social groups belonged to and attended in the last month," E subjects scored significantly higher than did C subjects at the 4-, 8-, and 12-month periods. There was no significant difference between the The results reported here are those of 65 E and 65 C subjects. In the tables and discussion that follow, groups of less than 65 are the result of missing data in cases where it was impossible to obtain the scheduled follow-up interview for reasons of patient nonavailability or lack of coopera¬ tion. Through assertive data collection, 80.8% of all possible vised measure significant differences, nor did several of the scales derived to measure social relationships. However, one scale no RESULTS Super- Activities, Social Relationships, and Quality of Environment—A Esteem Scale. Penal additional 6.9% The results of the first year of the study have been reported20 and reflect the within-treatment phase of the experiment. A summary of those results follows. Living Situations.—Throughout the first year, E subjects spent very little time in psychiatric institutions compared with C subjects (Table 1). This did not lead to a greater use by E subjects of medical or penal institutions or of supervised living situations in the community. In fact, the E group spent significantly more time than the C group in independent living situations in the community. Of the 58 C patients who were hospitalized, 34 were readmitted at Control Treatment Psychiatrio an Within-Treatment Results depressive patients. aftercare services available in and 17.44 28.14 8.96 23.39 6.37 22.39 12.02 24.69 8.95 26.38 86.99 34.22 70.54 37.02 32.50 82.56 28.14 91.04 23.39 | at at at < < .001. .05. < .01. 6.98 t 25.85 17.47 21.31 6.64 20.99 7.82 10.74 21.58 X SD 20.49 X SD 85.20 26.06 63.41 X SD 93.02 17.50 t 74.15 31.02 21.31 t 93.36 20.99 .;. t *E indicates the experimental group; C, the control group. tThe difference between the E and C groups is significant ÎThe difference between the E and C groups is significant §The difference between the E and C groups is significant Downloaded From: http://archpsyc.jamanetwork.com/ on 07/07/2012 i 82.09 § i 1.31 20.00 31.74 8.51 23.97 12.27 26.90 11.20 28.69 11.78 27.46 6.37 21.07 19.55 36.42 6.86 23.59 25.49 5.21 21.17 67.73 38.49 80.29 35.56 68.64 39.38 81.83 35.58 60.43 42.95 80.49 36.01 70.16 40.77 82.13 68.99 33.92 40.88 80.00 31.74 91.49 23.97 80.42 30.45 88.20 28.57 79.98 31.56 87.35 29.78 83.22 31.04 87.34 28.51 83.09 34.51 Table 2.—Mean Percentages Within-Treatment of Data-Collection Periods Phase, Unemploy¬ ment ment Competi¬ tive em¬ ployment E <n= 60) (n= 61) SD 33.76 36.48 SD 26.68 38.33 SD 39.56 42.49 Sheltered employ¬ C <n= 61) t C E (n= 57) (n= 59) (n= 58) 56.76 43.31 25.94 37.08 t 57.03 31.15 Î 56.91 1.10 22.20 t 8.24 42.14 42.69 13.53 22.50 37.69 33.20 36.03 54.53 46.27 9.79 22.39 38.64 44.03 43.07 47.30 45.86 *E indicates the experimental group; C, the control group. fThe difference between the E and C groups is significant at ÎThe difference between the E and C groups is §The difference between the E and C groups is significant significant Table 3.—Mean Amounts of Within-Treatment Phase, (n= 56) E (n= 59) 2.00 t C (n= 59) C (n= 57) at at Competitive t < < < 44.71 43.11 40.21 0.95 5.16 14.91 34.10 51.86 44.24 42.02 45.31 53.94 47.43 44.36 t mo 24 C 41.34 Phase, E (n= 60) 42.93 Situations* 20 16 E 36.23 5.06 Employment Posttreatment t 61.74 22.97 t 53.97 30.31 37.04 in Various mo 12 E Spent 28 C E C (n= 57) (n= 54) (n= 56) 32.63 43.41 51.29 46.17 37.06 44.14 § 54.77 15.64 1.28 48.40 0.29 1.91 35.01 9.63 7.65 23.84 1.78 1.79 42.80 44.51 51.73 47.91 47.43 46.50 55.29 47.36 43.45 48.20 t .001. .01. .05. Income (Dollars) Earned During Data-Collection Posttreatment mo 12 Phase, 20 16 Periods* mo 24 28 C C C C C C E E CE E E E E Dollars (n=61) (n=59) (n=61) (n=54) (n=59) (n=57) ( =59) ( =56) (n=58) ( =55) (n=59) (n=55) (n=54) (n=52) X 610.00 308.80 872.30 t 436.00 759.80f 418.90 825.00 535.00 834.00 t 398.00 734.00 367.00 875.00 t 359.70 SD 696.80 1,053.40 622.80 1,260.00 834.00 1,063.50 711.60 1,085.00 955.00 1,209.00 738.00 1,236.00 690.00 1,395.00 *E indicates the experimental group; C, the control group. fThe difference between the E and C groups is significant at groups on < .05. quality of environment (meals, quality of living Table 4.—Significant Differences Between Experimental (E) and Control (C) Groups on Items From the Short Clinical Rating Scale* situation, etc). Satisfaction With Life and Self-esteem.—The E subjects were significantly more satisfied with their life situations than were the C subjects at 12 months. The E group showed significantly higher self-esteem than the C group at baseline (P < .05). The two groups may actually represent different populations on this variable, but they did not differ significantly on any other variable at baseline. Since this measure was taken a few days after the patient's admission to the study, the lower self-esteem in the C group may be related to the fact that almost all C patients initially hospitalized while almost all E patients were kept in the community. Subsequently, both t tests and analyses of covariance of self-esteem scores of all the subsequent data-collection periods showed no significant were differences between the E and C groups. Symptomatology.—The E subjects showed less symptoma¬ tology postbaseline than did the C subjects, and by 12 months they showed better functioning on seven of the 13 scales (Table 4). Medication and Compliance.-No significant difference was found between the groups on the numbers of persons with prescribed psychotropic medications. The only signif¬ icant differences on compliance were at the 8- and 12month periods for antipsychotic medication, with the E group being more compliant than the C group. Follow-up Results The following summarizes the data from the latter half of the experiment, the period in which E subjects were no longer being treated by the TCL program but instead had traditional community programming available. Living Situation.—The most striking change was in use of Downloaded From: http://archpsyc.jamanetwork.com/ on 07/07/2012 Posttreatment Within-Treatment Phase, Phase, mo 12 Items Depressed .01 mood Suicidal trends .001 Anxiety or .001 .01 .05 .01 .01 16 20 mo 24 28 .02 fear of anger Social with¬ drawal Motor agita¬ tion Motor retarda¬ tion Paranoid be¬ havior Hallucinations Thought dis¬ order Expression .001 .01 Hyperactivity or .02t .001 .01 .05 elation Physical com¬ plaints Global illness .05t .05 .001 .01 *The numbers are the values of the significant differences between the groups. For all but two of the cases of significant differences, the C subjects were more symptomatic than the E subjects. tlndicates that the E subjects were more symptomatic than the C subjects. psychiatrie hospitals. In each data-collection period after cessation of the program there was a gradual but definite increase in hospital use by the E group. The time spent in hospital at the 28-month period was double that of the 12-month period, whereas use of the hospital by the C group from the 8-month data-collection period onward remained quite stable. Employment Status.—The time spent in sheltered employ¬ ment was quite constant while E patients were in the program (22% to 26% of their employment time). This percentage began to decline strikingly after cessation, and by 28 months it had dropped to less than 8%. There was an almost equal increase in unemployment and competitive employment. Unlike their other gains, the advantage the E subjects showed in money earned in competitive employ¬ ment did not deteriorate after cessation of the TCL program. Leisure Time Activities, Social Relationships, and Quality of Environment.—There continued to be no significant differ¬ ence between the groups on leisure time activities and quality of environment. However, the greater contact with trusted friends shown by the E group at 12 months disappeared postcessation. During the entire period, the E group maintained their significantly higher attendance at social groups. Satisfaction With Life and Self-esteem.—The greater satis¬ faction with life expressed by the E subjects at 12 months disappeared. The lack of difference between the groups in self-esteem continued unchanged from 4 months to the end of the experiment at 28 months. Symptomatology.—The striking difference in symptoma¬ tology that favored the E group while they were involved with TCL disappeared very rapidly. Medication.—After TCL, there continued to be no differ¬ ence between the groups in medications prescribed; howev¬ er, the difference in compliance that favored the E group at 8 and 12 months disappeared. COMMENT There are several factors that may influence any general conclusions from these findings. The study was conducted in a nonindustrial, progressive community that was recep¬ tive to this type of study. Our therapeutic interventions and our outcome measures involved values. These values were summarized by Cumming27: (1) it is better to be outside a hospital rather than inside; (2) it is better to work productively than to be dependent on others; (3) it is important to be effectively interdependent; and (4) it is a good thing for people to be happy. It should be clear that our diagnoses were based on clinical judgment rather than on research diagnostic crite¬ ria. We carefully trained our raters to measure symptoma¬ tology, but once the study was initiated, further reliability estimates were not made. Although there was no signifi¬ cant difference in medications prescribed, patients in the E group reported significantly greater compliance in the 8and 12-month collection periods than did the C patients. We can not partial out how much of the gains made by the E subjects was secondary to the success of the TCL program in gaining medication compliance as compared with its psychosocial interventions. it was possible to treat in the community an unselected group of patients who applied for admission to a state mental hospital. While most of the C subjects were admitted to the hospital and many were subsequently readmitted, almost all of the E patients had a sustained community tenure for the year. Most important, the data indicated that their sustained community living was not gained at the expense of their quality of life, level of adjustment, self-esteem, or personal satisfaction with life. Instead, relative to C patients, the E patients showed enhanced functioning in several significant areas and maintained less subjective distress and greater satisfac¬ tion with their lives in the 14 months of TCL treatment. However, our follow-up results indicated that when patients were weaned from the TCL program to more traditional community programming, many of the pre¬ viously noted differences between the groups disappeared and use of the hospital began to increase. Other studies have similarly found that when intensive treatment ceases patients regress and their use of the hospital sharply increases.2"-"' Several interrelated conclusions can be drawn. The first is that traditional community programming for these patients is either insufficient, inappropriate, or both. The second is that when community programming is inade¬ quate, the hospital is forced to serve as the primary locus of treatment for the patient rather than being used for the more appropriate specialized role it is capable of perform¬ ing. Third, the results suggest that for a large number of chronically disabled psychiatric patients treatment must be an ongoing rather than a time-limited endeavor. Our study suggests to us that this ongoing treatment program must be organized so that it can provide a flexible system of delivery that gives the patient only what he needs when he needs it and where he needs it. This involved careful assessment of patient needs, close monitoring of patient functioning, assertive intervention, and working closely with and providing support to community members as well hospital, as patients. Implementation Problems This treatment model has several barriers to wide implementation. The major one is financing; even though this model is economically feasible in terms of total costs and benefits (for details see the second article in this series by Weisbrod et al, pp 400-405), the kinds of services it provides are largely not reimbursable by third-party payers. Modes of treatment that are reimbursable have a profound influence on shaping the types of services pro¬ vided. As Mechanic" pointed out, it is relatively easy to determine what one must pay for a day in the hospital, but it is much more difficult to determine how to pay for a total pattern of services that includes medical care and social supports. One possible solution is payment on a capitation basis, but if new funding mechanisms are not developed, TCL-type programs will not be widely implemented. Another barrier lies in the difficulties inherent in dissem¬ inating programs that require social technologies that require considerable coordinating ability and that fall outside of the usual organizational patterns of the medical sector.31 Role of the Effects of the TCL Program With such limitations in mind, the within-treatment results indicated that the TCL program was an effective alternative to mental hospital treatment for the large majority of subjects. Specifically, with minimal use of the Downloaded From: http://archpsyc.jamanetwork.com/ on 07/07/2012 The Hospital study has helped us define our own views of what a hospital's role can optimally be. Although hospitalization may have undesirable effects on patients, there may be greater patient harm and certainly greater burden to the community if use of the hospital is denied on "principle" without providing adequate community programming in its place. The more comprehensive the community pro¬ gram, the less need there is to use the hospital. With a program such as TCL available, we believe that the hospi¬ tal need be used only for the following cases: 1. For protection of the individual or others when the patient is imminently suicidal or homicidal. Care must be taken to not hospitalize patients who use self-destructive behavior as a means of getting help. This presents a very burdensome clinical judg¬ that can be learned and made if the clinician is willing to do so. In our experience, if the patient is provided with the support he needs, the danger is minimal. 2. For patients whose psychiatric illness is complicated by significant medical problems that require the special diagnostic and treatment facilities only available in a hospital. 3. For patients whose psychosis is so severe that they require the structure and good nursing care that only a hospital can provide. The goal here is to medicate the patient and interrupt the psychotic process as quickly as possible. We have used the hospital for this purpose with patients in the midst of a very manic episode or a highly disruptive schizophrenic episode when we were unable to insure that the patient was being adequately medicated. The length of hospitalization in these cases was rarely over two weeks and often a matter of days. ment, but one Psychosis per se was not necessarily an indication to hospitalize the patient. We were able to successfully treat many patients who were acutely psychotic without use of the hospital. Furthermore, the TCL program, which limited hospital use, did not increase the burden to families or to the community (for details see the third article in this series by Test and Stein, pp 409-412). Given adequate community programming, we envisage use of the psychiat¬ ric hospital only in the specific instances just described. There is one obvious qualifier: we do not know what the TCL program would provide or encounter over a period of five years Finally, or longer. we chronic believe that until we are able to prevent or psychiatric disease we should change our treatment strategy from preparing patients for communi¬ ty life to maintaining patients in community life. A fruitful area for research would be to identify what Holzman32 referred to as "pathotrophic factors" (that is, cure those that feed and nurture the disorder once it has developed) as well as to identify those factors that we call 'normatrophic" (that is, those that lead toward stabiliza¬ tion and normalization of functioning). Treatment pro¬ grams constructed to help the chronically disabled psy¬ chiatric patient to modify or avoid pathotrophic factors and to acquire normatrophic factors would be very useful to this long-neglected group of people. This investigation was supported in part by grant 05-R 000009 from the National Institute of Mental Health. The research staff. Rick Bowman, MA, Carl Schwanz, BS, Suzanne Senn, BA, and Gene Jackson, MSW, provided skillful and diligent assistance. References 1. Anthony WA, Buell GJ, Sharratt S, et al: Efficacy of psychiatric rehabilitation. Psychol Bull 78:447-456, 1972. 2. Caffey EM, Jones RB, Diamond LS, et al: Brief hospital treatment of schizophrenia: Early results of a multiple hospital study. Hosp Community Psychiatry 19:282-287, 1968. 3. Gove inpatients: W, Ludach JE: A An intensive treatment program for description and evaluation. psychiatric J Health Soc Behav 10:225-236, 1969. 4. Weisman G, Feirstein A, Thomas C: Three-day hospitalization: A model for intensive intervention. Arch Gen Psychiatry 21:620-629, 1969. 5. Glick ID, Hargreaves WA, Drues J, et al: Short versus long hospitalization: A prospective controlled study: IV. One-year follow-up results for schizophrenic patients. Am J Psychiatry 133:509-514, 1976. 6. Glick ID, Hargreaves WA, Drues J, et al: Short versus long hospitalization: A prospective controlled study: V. One-year follow-up results for nonschizophrenic patients. Am J Psychiatry 133:515-517, 1976. 7. Herz MI, Endicott J, Spitzer RL: Brief hospitalization: A two-year follow-up. Am J Psychiatry 134:502-507, 1977. 8. Glasscote RM, Kraft AM, Glassman SM, et al: Partial Hospitalization for the Mentally Ill. Washington, DC, Joint Information Services of the American Psychological Association and the National Association for Mental Health, 1969. 9. Budson RD: Psychiatric Halfway Houses: A Handbook of Theory and Practice. Pittsburgh, University of Pittsburgh Press, 1978. 10. Glasscote RM, Cumming E, Rutman IP, et al: Rehabilitating the Mentally Ill in the Community. Washington, DC, Joint Information Services of the American Psychological Association and the National Association for Mental Health, 1978. 11. Langsley DG, Kaplan DM: The Treatment of Families in Crisis. New York, Grune & Stratton Inc, 1968. 12. Pasamanick B, Scarpitti F, Dinitz S: Schizophrenics in the Communi- ty: An Experimental Study in the Prevention of Hospitalization. New York, Appleton-Century-Crofts, 1967. 13. Rittenhouse JD: Endurance of effect: Family-unit treatment compared to identified-patient treatment, in Proceedings of the Annual Conven- tion of the American Psychological Association. Washington, DC, American Psychological Association, 1970, vol 2, pp 535-536. 14. Satir V: Conjoint Family Therapy. Palo Alto, Calif, Science and Behavior Books Inc, 1967. 15. Mosher LR, Menn AZ, Mathews S: Soteria: Evaluation of a homebased treatment for schizophrenia. Am J Orthopsychiatry 45:455-469, 1975. 16. Mosher LR, Menn AZ: Lowered barriers in the community: Downloaded From: http://archpsyc.jamanetwork.com/ on 07/07/2012 The Soteria model, in Stein LI, Test MA (eds): Alternatives to Mental Hospital Treatment. New York, Plenum Publishing Corp, 1978, pp 75-113. 17. Polak PR, Kirby MW: A model to replace psychiatric hospitals. J Nerv Ment Dis 162:13-22, 1976. 18. Herz MI, Endicott J, Spitzer RL, et al: Day versus inpatient hospitalization: A controlled study. Am J Psychiatry 127:1371-1382, 1971. 19. Michaux MH, Chelst MR, Foster SA, et al: Day and full-time psychiatric treatment: A controlled comparison. Curr Ther Res 14:279-292, 1972. 20. Wilder JF, Levin G, Zweling J: A two-year follow-up evaluation of acute psychiatric patients treated in a day hospital. Am J Psychiatry 122:1095-1101, 1966. 21. Mechanic D: Alternatives to mental-hospital treatment: A sociological perspective, in Stein LI, Test MA (eds): Alternatives to Mental Hospital Treatment. New York, Plenum Publishing Corp, 1978, pp 309-320. 22. Stein LI, Test MA: An alternative to mental-hospital treatment, in Stein LI, Test MA (eds): An Alternative to Mental Hospital Treatment. New York, Plenum Publishing Corp, 1978, pp 43-55. 23. Stein LI, Test MA: Retraining a hospital staff for work in a community program in Wisconsin. Hosp Community Psychiatry 27:266-268, 1976. 24. French NH, Heninger GR: A short clinical rating scale for use by nursing personnel: I. Development and design. Arch Gen Psychiatry 23:233-240, 1970. 25. Rosenburg M: Society and the Adolescent Self-image. Princeton, NY, Princeton University Press, 1965. 26. Test MA, Stein LI: Training in community living: Research design and results, in Stein LI, Test MA (eds): An Alternative to Mental Hospital Treatment. New York, Plenum Publishing Corp, 1978, pp 57-74. 27. Cumming JH: Some criteria for evaluation, in Roberts LM, Greenfield N, Miller M (eds): Comprehensive Mental Health: The Challenge of Evaluation. Madison, University of Wisconsin Press, 1968, pp 29-40. 28. Marx AJ, Test MA, Stein LI: Extrohospital management of severe mental illness: Feasibility and effects of social functioning. Arch Gen Psychiatry 29:505-511, 1973. 29. Langsley DG, Machotka P, Flomenhaft K: Avoiding mental hospital admission: A follow-up study. Am J Psychiatry 127:1391-1394, 1971. 30. Davis AE, Dinitz S, Pasamanick B: Schizophrenia in the New Custoidal Community. Ohio, Ohio State University Press, 1974. 31. Mechanic D: Consideration in the design of mental health benefits under national health insurance. Am J Public Health 68:482-488, 1978. 32. Holzman PS: The modesty of nature: A social perspective on schizophrenia. Soc Sci Rev 588:-603, 1977.