375
Original Contributions
Are Hypertension or Cardiac Embolism
Likely Causes of Lacunar Infarction?
J. Lodder, MD, J.M. Bamford, MD, MRCP, P.A.G. Sandercock, DM, MRCP,
L.N. Jones, BA, and C.P. Warlow, MD, FRCP
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
We tested the hypothesis that hypertension is more common and cardiac embolism less
common in patients with lacunar infarction than in patients with other types of cerebral
infarction. We studied risk factor profiles in a series of 102 consecutive patients with a lacunar
infarct and 202 consecutive patients with a carotid artery-distribution infarct involving the
cortex registered in the Oxfordshire Community Stroke Project, a community-based study of
first-ever stroke. The two groups did not differ in the prevalence of prestroke hypertension
(defined in a number of ways) or in the prevalence of markers of sustained hypertension. The
presence of atrial fibrillation and a history of myocardial infarction, particularly during the 6
weeks before the stroke, were significantly more common in the group with carotid-distribution
infarcts involving the cortex. There was no significant difference in the prevalence of other
accepted risk factors for ischemic stroke, including previous transient ischemic attack, cervical
bruit, diabetes mellitus, peripheral vascular disease, or cigarette smoking. Our results suggest
that hypertension is no more important in the development of lacunar infarction than it is in
the development of other types of ischemic stroke that are presumed to be due to atherosclerotic
thromboembolism in a major cerebral artery. Our data support the autopsy evidence that
cardioembolic occlusion is an unusual cause of lacunar infarction. (Stroke 1990^1:375-381)
L
acunar infarcts are thought to result from the
occlusion of a single perforating artery and
f may be manifested clinically as a few specific
lacunar syndromes.1-2 This clinicopathologic concept
was substantiated in a recent community-based natural history study.3 Almost 25% of all first-ever
ischemic strokes in that study were due to lacunar
infarction, and similar proportions have been
reported from other studies.4-6 From his studies on
its pathogenesis, Fisher originally suggested that
lacunar infarction was caused almost exclusively by
small-vessel disease related to hypertension, 1
although he could not exclude embolism as a possible
cause in a few cases.7 However, the role of hypertension in the genesis of lacunar infarction has been
From the Department of Neurology, University Hospital Maastricht, Maastricht, The Netherlands (J.L.), the Department of
Neurology, St. James's University Hospital, Leeds (J.M.B.), the
University Department of Clinical Neurosciences, Western General Hospital, Edinburgh (P.A.G.S., C.P.W.), and the University
Department of Community Medicine and General Practice, Radcliffe Infirmary, Oxford (L.NJ.), United Kingdom.
Supported by grants from the British Medical Research Council
and the Chest, Heart and Stroke Association. J.L. was supported
by the Dutch Heart Foundation.
Address for correspondence: J. Lodder, Department of Neurology, University Hospital Maastricht, P.O. Box 1918, 6201 BX
Maastricht, The Netherlands.
Received December 15, 1988; accepted November 27, 1989.
questioned recently.8 Both cardiac and carotid
emboli have been suggested as possible causes of
lacunar infarcts, because hypertension appeared not
to be present in a substantial number of cases.
Distinguishing the types of cerebral infarction on
the basis of the underlying pathogenesis is important
in the planning of stroke treatment trials. 910
Although additional unselected pathologic studies
would be of great value, they are difficult to perform
because of the low early case-fatality rate and consequently the low autopsy rate for persons with
lacunar infarction.3 Therefore, one needs to use
other methods of examining whether the underlying
vascular pathology of lacunar infarction is qualitatively different from that of infarction involving the
cortical distribution of the major cerebral arteries, in
which thromboembolism is thought to be the most
likely pathologic process. Comparing the distributions of vascular risk factors could add to our understanding of the pathogenesis of lacunar infarction.
We report the results of such a comparison among
patients registered with the Oxfordshire Community
Stroke Project, a community-based stroke registry.
Subjects and Methods
The detailed methodology of the Oxfordshire
Community Stroke Project has been described.11 In
brief, it is a prospective, community-based registry of
376
Stroke
Vol 21, No 3, March 1990
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
all first-ever strokes and transient ischemic attacks
(TIAs) occurring in a population of approximately
105,000. Patients were assessed by a study neurologist soon after the event, whether or not they were
admitted to a hospital. When taking the history,
particular note was made of symptoms of cardiac
disease, previous TIA, the diagnosis of diabetes
mellitus, intermittent claudication of the lower limbs,
and whether the patient was currently taking antihypertensive medication. The patients were questioned
about their smoking habits. During a standard physical examination, special note was made of blood
pressure, signs of cardiac disease, presence of cervical bruits, or evidence of lower limb ischemia. We
attempted to obtain a computed tomogram (CT
scan) or autopsy on all patients to determine accurately the pathologic type of stroke. An electrocardiogram (ECG) was recorded at the time of assessment to document cardiac rhythm abnormalities and
as an indirect assessment of left ventricular hypertrophy. On a standard chest roentgenogram cardiomegaly was denned as a cardiothoracic ratio of >50%.
One major advantage of the British National
Health Service is that >98% of the population is
registered with a general practitioner who provides
primary health care and arranges for specialist advice
or hospital admission. A unique set of health records
that comprises all correspondence with hospital specialists and details of consultations with the general
practitioner (e.g., blood pressure recordings) is held
by each patient's general practitioner. If the patient
moves to another area, then these health records are
transferred to the next general practitioner, thereby
creating a lifelong health record. We reviewed the
general practitioner's and hospital notes of all
patients with a stroke or TIA registered in the
Oxfordshire Community Stroke Project and recorded
the details of prestroke blood pressure measurements and checked the details of any significant
previous medical events. A diagnosis of myocardial
infarction (MI) was accepted only if an episode of
typical chest pain was supported by either the development of pathologic Q waves on a standard twelvelead ECG or characteristic enzyme changes at the
time of the event. Since some patients were likely to
have more than one manifestation of ischemic heart
disease, a number of features (nonrheumatic atrial
fibrillation [AF], definite MI, angina, or typical ECG
changes of myocardial ischemia) were considered to
indicate any ischemic heart disease, even if there
were no clinical symptoms.
Stroke was classified as being due to definite
cerebral infarction if a CT scan performed ^28 days
after the onset of symptoms showed either a lowdensity area in a region compatible with the clinical
symptoms and signs or no specific abnormality or if
an autopsy showed an appropriate infarct. If adequate CT or autopsy data were not available, the
Guy's Hospital Diagnostic Score, a CT-validated
score that predicts the probability of a stroke being
due to infarction or hemorrhage using a number of
clinical features, was applied.12 This is the most
accurate clinical method of making such a differentiation and has been tested on data sets other than
the one from which it was derived.13 Patients who
had a score of <4 (i.e., a >90% probability that thenstroke was due to cerebral infarction) were classified
as having probable cerebral infarction. For the purposes of this report, cases of definite and probable
cerebral infarction were combined.
Lacunar infarction was defined as a cerebral
infarction in a patient with clinical symptoms and
signs compatible with a lacunar syndrome (pure
motor stroke, pure sensory stroke, sensorimotor
stroke, or ataxic hemiparesis) as denned previously.3
Where available, CT or autopsy in such patients
showed either infarcts in an appropriate area supplied by a single artery or no specific abnormality.
Carotid artery-distribution infarction involving the
cortex was denned as a cerebral infarction in a
patient with one of the following clinical patterns at
presentation: 1) any unilateral motor and/or sensory
disturbance if accompanied by acute ipsilateral
higher cortical dysfunction (e.g., dysphasia) and/or
an ipsilateral homonymous hemianopsia; 2) an isolated motor or sensory disturbance restricted to the
face, arm, or leg (for distinction from lacunar
syndromes3); or 3) isolated acute higher cortical
dysfunction. These clinical features are usually considered to arise from infarcts in areas supplied by
cortical branches of the anterior or middle cerebral
arteries.14 Where available, CT or autopsy in such
patients showed either infarcts in an appropriate
area or no specific abnormality.
Patients with cerebral infarction presumed to be
within the distribution of the vertebrobasilar system
were excluded from the present study for two reasons. First, there is some pathologic evidence that
such infarcts are more likely to be due to in situ
thrombosis than are carotid-distribution infarcts,15
and second, there continues to be debate as to
whether lacunes can cause some of the classic brainstem syndromes.16
Differences between the two groups were analyzed
using odds ratios with 95% confidence intervals17 for
discrete variables and using analysis of covariance18
for continuous variables. The x1 test was performed
using Yates' correction.19
Results
Between November 1,1981, and October 31,1984,
515 patients with a first-ever stroke were registered
with the Oxfordshire Community Stroke Project; 102
had a lacunar infarct and 202 a carotid-distribution
infarct involving the cortex. A CT scan s28 days after
onset or an autopsy was performed in 87 (85%) and
171 (85%) of the patients in the two groups, respectively; 29 (28%) and 103 (51%) of the patients
showed infarcts in an appropriate area, respectively.
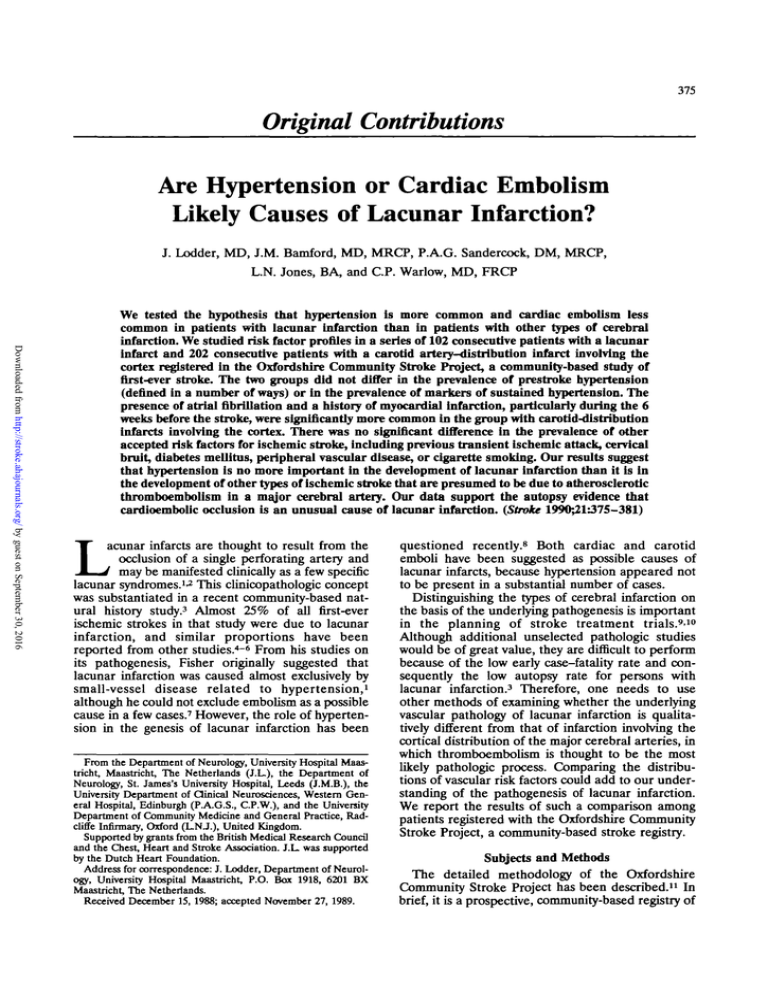
The former group comprised 42 men and 60 women
with a mean±SD age of 71.8 ±11.9 years, while the
latter group comprised 108 men and 94 women with
Lodder et al
30 -
10 -
Age
No.
<55
12 6
I
55-64
10 27
65-74
14 30
I
75-84
11 36
m\
>85
2 10
40-
Discussion
The lacunar hypothesis has two distinct components, first, that a few specific clinical syndromes are
usually caused by small deep infarcts or lacunes and
second, that lacunes are usually the result of a
distinct small-vessel arteriopathy that occludes a single perforating artery at the base of the brain.2 The
lacunar hypothesis was generated from a few meticulously performed autopsy studies.1-;-20-26 The clinicopathologic correlation has been tested and substantiated in our prospective, community-based
study, in which among 108 patients with carefully
defined lacunar syndromes, only three had a primary
intracerebral hemorrhage and only three had CT or
autopsy findings not compatible with occlusion of a
single perforating artery.3 However, the second part
of the lacunar hypothesis (i.e., that these strokes are
due to a qualitatively distinct small-vessel arteriopathy [not atheroma]) has proven more difficult to test.
In view of the low case-fatality rate of lacunar
infarction,3 few pathologic studies on unselected
patients are likely to be performed and current
radiologic techniques are of little help. Therefore, we
turned to epidemiology and asked the question "Is
there a difference in the prevalence of vascular risk
factors between patients with lacunar infarcts and
those who might reasonably be considered to have
infarcts due to thromboembolism?"
30-
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
20-
I
10-
Age
Na
<55
5
2
55-64
5 11
65-74
17 29
75-84
21 36
377
91 of the 102 patients (89%) with lacunar infarcts
and in 184 of the 202 patients (91%) with cortical
infarcts, of which 88 and 179, respectively, were in
the general practitioner's notes. There were no significant differences between groups for the prevalence of any marker of sustained hypertension or for
either measurement of prestroke blood pressure.
Point estimates of the odds ratios and 95% confidence intervals for the prevalence of potential cardiac sources of emboli and other accepted risk factors for ischemic stroke are detailed in Table 3. The
presence of AF and MI before the stroke were
significantly more common among the patients with
carotid-distribution infarcts involving the cortex.
40 -
20 -
Risk Factors for Cerebral Infarction
>85
12 15
FIGURE 1. Bar graphs. Age distribution by sex of 102 cases of
lacunar infarction (hatched bars) and 202 cases of carotid
artery-distribution infarction involving the cortex (open bars).
Upper graph: males; lower graph: females.
a mean±SD age of 73.2±10.9 years. The odds ratio
of the sex difference was 0.61 (95% confidence
interval 0.38-0.99, ;^=3.62; difference not significant). The age and sex distributions of the two groups
is shown in Figure 1.
Table 1 summarizes the prevalence of hypertension defined in a number of ways as discrete variables. Table 2 shows the mean in each group for
maximum blood pressure ever recorded, last blood
pressure recorded in the general practitioner's notes
before the stroke, and blood pressure recorded at the
time of poststroke assessment for registration in the
Oxfordshire Community Stroke Project. Blood pressure was recorded at some time before the stroke in
TABLE 1. Prevalence of Hypertension as Discrete Variables in Patients With Lacnnar Infarction and Those With
Carotid Artery-Distribution Infarction Involving the Cortex
Patients with
Hypertension defined as
Lacunar
infarction
( n - 102)
%
No.
Cortical
infarction
(n=202)
No.
%
Odds
ratio
95% Confidence
interval
Prestroke blood pressure of > 160/90 mm Hg at
least twice
On antihypertensive medication
Left ventricular hypertrophy on electrocardiogram*
Cardiomegaly on chest roentgenogramt
45
28
15
32
95
58
23
80
0.89
0.94
1.34
0.70
0.55-1.43
0.55-1.60
0.67-2.70
0.42-1.15
44
27
15
33
Odds ratio of <1.0, less prevalent in group with lacunar infarcts.
*n=100 for lacunar infarction and n=197 for cortical infarction.
tn=97 for lacunar infarction and n = 181 for cortical infarction.
47
29
12
44
378
Stroke Vol 21, No 3, March 1990
TABLE 2. Blood Pressure Recordings In Patients With I.»cinar Infarction and Those With Carotid ArteryDlstribution Infarction Involving the Cortex
Measurement
Maximum BP before stroke
Systolic
Diastolic
Last BP recorded by GP before stroke
Systolic
Diastolic
BP at OCSP assessment
Systolic
Diastolic
Patients with
Lacunar infarction
Cortical infarction
102)
(n=2O2)
Mean
Mean
(mmHg)
No.
No.
(mmHg)
F
P
91
91
179.9
97.4
184
184
183.2
101.4
0.70
3.29
NS
NS
88
88
158.0
88.0
179
179
155.0
87.0
0.96
0.14
NS
NS
102
102
165.7
89.0
201
201
157.1
86.1
3.89
1.42
0.05
NS
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
BP, blood pressure; OCSP, Oxfordshire Community Stroke Project; GP, general practitioner, NS, not significant
The methodologic details of the Oxfordshire Community Stroke Project have been reported in detail11
and should have avoided any selection bias. We have
shown that patients with impairment of consciousness (not a feature of lacunar infarction) are more
likely than those with normal consciousness to be
admitted to a hospital,27 and therefore it is important
that any study of risk factor prevalence among clinically distinct types of stroke be community-based and
obtain complete case ascertainment Our study was
restricted to cases of first-ever stroke since one might
expect certain pathologic processes to be more likely
to cause recurrent stroke than others; in particular,
one might expect that recurrent embolism could
result from a carotid or cardiac lesion, whereas
further symptoms related to occlusion of a single
perforating artery are unlikely. There is also considerable difficulty in assessing whether patients have a
lacunar syndrome if there are residual physical signs
due to a previous stroke. The data on clinical features
and risk factors of patients registered with the
Oxfordshire Community Stroke Project were collected prospectivery and independently of each other.
The definition of lacunar infarction has been discussed in detail.2'3 We confined our comparison to
two groups of patients with combinations of symptoms and signs expected to result from lesions involving the cerebral cortex and conventionally thought of
as being referable to the distribution of the cortical
branches of the carotid artery.14 We excluded
patients with symptoms and signs of brainstem or
occipital lobe disturbance. Since it is unusual to see
CT abnormalities in >40% of patients with lacunar
syndromes,3-6 we considered that distinguishing the
groups by their clinical features was the method least
likely to lead to bias. Recent work using magnetic
TABLE 3. Prevalence of Cardiac Sources of EmboU and Other Accepted Risk Factors for Ischemic Stroke in Patients
With Lacnnar Infarction and Those With Carotid Arterv-Distribution Infarction Involving the Cortex
]Patients
with
Lacunar
infarctior l
(n-102)
Risk factors
Atrial fibrillation on electrocardiogram
Myocardial infarction £6 weeks
before stroke
At any time before stroke
Angina pectoris
Any ischemic heart disease
Cardiac valve disease
Previous transient ischemic attack
Cervical bruits
Diabetes mellitus
Lower limb claudication
Ever smoked cigarettes
No.
10
2
15
20
40
9
18
14
13
11
69
Cortical
infarctioi l
(n=202)
10
No.
44
2
15
20
39
9
18
14
13
11
68
17
52
38
101
22
37
27
19
28
139
%
Odds ratio of <1.0, less prevalent in group with lacunar infarcts.
95% Confidence
interval
22
Odds
ratio
0.39
8
26
19
50
11
18
13
9
14
69
0.22
0.50
1.05
0.65
0.79
0.96
1.03
1.41
0.75
0.94
0.05-0.96
0.26-0.94
0.58-1.92
0.40-1.05
0.35-1.79
0.51-1.78
0.51-2.07
0.66-2.98
0.36-1.58
0.57-1.58
%
0.19-0.81
Lodder et al
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
resonance imaging supports the view that lacunar
syndromes are usually caused by small deep infarcts
even if no lesion is visible on CT.28 The absence of
any significant difference in the age distributions
between the groups allowed direct comparisons even
for variables the prevalence of which are known to be
age-dependent.
For many years it has been accepted that lacunes
are caused by hypertensive small-vessel disease;
indeed, some authors have insisted on the presence
of hypertension as a diagnostic feature of lacunar
infarcts. However, recent reports have noted that
such lesions can occur in patients who have no
evidence of hypertension. Kappelle and van Gijn29
reviewed 14 recent studies of lacunar stroke and
found that 43-83% of cases were "hypertensive."
The association between hypertension and the presence of lacunes at autopsy was recognized by Fisher,1
although in his study 80% of the lacunes occurred in
a single patient with the clinical features of the
lacunar state rather than with discrete strokes presenting as lacunar syndromes. However, these pathologic findings cannot necessarily be regarded as one
extreme of a disease spectrum in which patients with
single lacunes presenting as lacunar strokes are at the
other end and all have similar risk factors. No
previous study has compared the prevalence of
hypertension between patients with lacunar and
other types of ischemic stroke in a population unbiased by hospital admission, yet this is important since
hypertension is recognized as the most important risk
factor (after age) for all types of stroke.30 Additional
problems include the facts that "hypertension" has
not been uniformly defined in the literature and most
studies have relied on poststroke blood pressure
measurements, which do not reliably reflect prestroke levels.31
It is clear that the most detailed way of assessing
the impact of prestroke blood pressure is in a cohort
of patients free of stroke at entry into the study. The
main problem lies in the fact that huge numbers of
people need to be followed over many years for there
to be a sufficient number of stroke events to allow
meaningful statistical analysis. We assessed prestroke
blood pressure in a number of ways, and it is noteworthy that 90% of patients had had their blood
pressure recorded by their general practitioner at
some time before their stroke. We also analyzed our
data using a conventional definition of hypertension
(blood pressure of > 160/90 mm Hg on two or more
occasions). We also compared indirect markers of
sustained hypertension. No significant or substantial
difference was found in the prevalence of any of
these factors between the groups. The significantly
lower mean systolic blood pressure in the group with
carotid-distribution infarcts involving the cortex at
the time of the stroke probably reflects the higher
prevalence of acute cardiac disease in this group.
Therefore, we could not find any evidence to support
the view that patients with hypertension are more
likely to develop lacunar infarction than other types
Risk Factors for Cerebral Infarction
379
of cerebral infarction, nor did hypertension (however
defined) appear to be a prerequisite for developing
lacunar infarction. Therefore, other causes of a
small-vessel arteriopathy need to be considered.
Could some lacunar infarcts be caused by cardiogenic emboli? Fisher7 suggested that embolism might
have caused lacunar infarcts in two patients who at
autopsy had no obstruction of the artery supplying
the infarcted territory. However, in view of the acute
angle at which the perforating arteries arise from the
parent artery and the flow characteristics of paniculate matter in the blood, one might speculate that
embolic occlusion of an individual perforating artery
is unlikely. Moreover, cardiogenic emboli are presumed to be large and more likely to lodge at a major
arterial branch.32 Bladin and Berkovic33 reported
that embolism could cause large striatocapsular infarcts, but these lesions were usually caused by
occlusion of more than one perforating artery, the
embolus lodging in the proximal segment of the
middle cerebral artery. Patients with this type of
lesion do not usually present with a classic lacunar
syndrome. Although the cases reported by Santamaria et al34 were likely to be due to cardiogenic emboli,
the authors noted that few presented with classic
lacunar syndromes.
The fashion for diagnosing cardioembolic stroke
waxes and wanes, and no diagnostic tests have
changed the fact that the majority of such diagnoses
are made by inference when a stroke and a cardiac
lesion coexist.35 Of the factors recorded in our study,
both AF and MI, especially MI ^6 weeks before the
stroke, would be accepted as potential sources of
cardiogenic emboli, although they may also be markers of generalized atherosclerosis. The prevalence of
AF was significantly lower in the group with lacunar
infarcts, and this finding is similar to that of a
hospital-based study.36 A recent case-control study
reported that patients with lacunar infarcts had the
same prevalence of AF as controls without stroke.37
Only two of our patients with lacunar infarcts had
sustained a recent MI, which meant that the confidence interval was wide; even so, conventional statistical significance was almost attained.
While potential sources of cardiogenic emboli are
less prevalent in patients with lacunar infarcts, it is
not certain whether embolism was actually the pathologic mechanism for the infarction since there was a
trend for cardiac disease in general to be less prevalent among such patients. Therefore, our results
support the view that cardiogenic embolism is
unlikely to be a common cause of lacunar infarction.
We did not directly assess disease at the carotid
bifurcation, although the prevalence of cervical bruits
was similar in the two groups. However, a previous
review has suggested that significant lesions are much
less frequent in patients with lacunar infarction than
in patients with other types of cerebral infarction.29-38-39 This again supports the view that arteryto-artery embolism is not a frequent cause of lacunar
infarction. It is well recognized that patients with no
380
Stroke
Vol 21, No 3, March 1990
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
abnormalities of the carotid artery can have TIAs40
and that TIAs can occur in patients who subsequently have a lacunar stroke.16 Therefore, one cannot necessarily accept that distal artery-to-artery
embolization is the cause of all TIAs. The prevalence
of previous TIAs was similar in our two groups.
Diabetes mellitus is associated with small-vessel disease in other parts of the body as well as with atheroma,
but there was no significant difference in the prevalence
of this condition between the groups. Similarly, intermittent claudication (a marker of generalized atherosclerosis) was equally prevalent in the two groups.
Although our data did not permit a detailed analysis of
the duration of smoking, we have no reason to think
that this differed between the groups.
In conclusion, hypertension is not a prerequisite for
the development of lacunar infarction and is no more
prevalent in patients with lacunar infarcts than in those
with cerebral infarcts due to occlusion of one or more
major cortical branches of a carotid artery. Further
research should be directed toward determining why
some patients develop small-vessel disease within the
brain and subsequently lacunar strokes while others
with similar risk factors develop atheromatous largevessel disease and then large infarcts involving the
cortex. The possibility that some patients have both
types of arterial pathology, with one type simply becoming symptomatic first, needs to be examined Cardiogenic embolism seems less likely to be a cause of
lacunar infarction than cortical infarction in the carotid
artery territory. This supports the idea that lacunar
infarcts may be due to a specific small-vessel arteriopathy, which may require different treatment than largevessel atherosclerosis. Although we cannot comment
on the possibility of artery-to-artery embolism, other
work suggests that this is also less likely to cause lacunar
than cortical infarction.
References
1. Fisher CM: The arterial lesions underlying lacunes. Acta
Neuropathol (Berl) 1969;12:1-15
2. Bamford JM, Warlow CP: Evolution and testing of the lacunar
hypothesis. Stroke 1988;19:1074-1082
3. Bamford JM, Sandercock P, Jones L, Warlow C: The natural
history of lacunar infarction: The Oxfordshire Community
Stroke Project Stroke 1987;18:545-551
4. Mohr JP, Caplan LR, Melski JW, Goldstein RJ, Duncan GW,
Kistler JP, Pessin MS, Bleich HL: The Harvard Cooperative
Stroke Registry: A prospective registry. Neurology 1978;
28:754-762
5. Kunitz SC, Gross CR, Heyman A, Kase CS, Mohr JP: The
Pilot Stroke Data Bank: Definition, design and data. Stroke
1984;15:740-746
6. Gross CR, Kase CS, Mohr JP, Cunningham SC, Baker WE:
Stroke in south Alabama: Incidence and diagnostic features —
A population based study. Stroke 1984;15:249-255
7. Fisher CM: Capsular infarcts —The underlying vascular
lesions. Arch Neurol 1979;36:65-73
8. van Gijn J, Kraaijeveld CL: Blood pressure does not predict
lacunar infarction. / Neurol Neurosurg Psychiatry 1982;
45:147-150
9. Miller VT: Lacunar stroke. A reassessment. Arch Neurol
1983;40:129-134
10. Spence JD, Donner A: Problems in the design of stroke
treatment trials. Stroke 1982;13;94-99
11. Bamford J, Sandercock P, Dennis M, Warlow C, Jones L,
McPherson K, Vessey M, Fowler G, Molyneux A, Hughes T,
Burn J, Wade D: A prospective study of acute cerebrovascular
disease in the community: The Oxfordshire Community Stroke
Project 1981-1986. 1. Methodology, demography and incident
cases of first-ever stroke. / Neurol Neurosurg Psychiatry 1988;
51:1373-1380
12. Allen CMC: Clinical diagnosis of the acute stroke syndrome.
QJMed 1983^08:515-523
13. Sandercock PAG, Allen CMC, Corsten RN, Harrison MJG,
Warlow CP: Clinical diagnosis of intracranial haemorrhage
using Guy's Hospital score. Br Med J 1985;291:1675-1678
14. Ad Hoc Committee of the National Institute of Neurological
and Communicative Disorders and Stroke: A classification and
outline of cerebrovascular diseases IT. Stroke 1975;6:564-616
15. Escourelle R: Manual of Basic Neuropathology. Philadelphia,
WB Saunders Co, 1978
16. Fisher CM: Lacunar strokes and infarcts: A review. Neurology
1982;32:871-876
17. Morris A, Gardner MJ: Calculating confidence intervals for
relative risks (relative odds) and standardized ratios and rates.
BrMedJ (Clin Res) 1988;296:1313-1316
18. Nie NH, Hull CH, Jenkins CG, Steinbrenner K, Brent DH:
Statistical Package for the Social Sciences. New York, McGrawHill Book Co, 1975
19. Armitage P: Statistical Methods in Medical Research. Oxford,
Blackwell, 1971
20. Fisher CM, Curry HB: Pure motor hemiplegia of vascular
origin. Arch Neurol 1965;13:30-44
21. Fisher CM: Pure sensory stroke involving face, arm and leg.
Neurology 1965;15:76-80
22. Fisher CM, Cole M: Homolateral ataxia and crural paresis: A
vascular syndrome. / Neurol Neurosurg Psychiatry 1965;
28:48-55
23. Fisher CM: A lacunar stroke. The dysarthria-clumsy hand
syndrome. Neurology 1967;17:614-617
24. Mohr JP, Kase CS, Meckler RJ, Fisher CM: Sensorimotor
stroke due to thalamocapsular ischaemia. Arch Neurol 1977;
34:739-741
25. Fisher CM: Thalamic pure sensory stroke: A pathologic study.
Neurology 1978;28:1141-1144
26. Fisher CM: Ataric hemiparesis. A pathologic study. Neurology
1978;35:126-128
27. Bamford JM, Sandercock PAG, Warlow CP, Gray JM: Why
are patients with acute stroke admitted to hospital? Br Med J
(Clin Res) 1986;292:1369-1372
28. Rothrock JF, Lyden PD, Hesselink JR, Brown JJ, Healy ME:
Brain magnetic resonance imaging in the evaluation of lacunar
stroke. Stroke 1987;18:781-786
29. Kappelle LJ, van Gijn J: Lacunar infarcts. Clin Neurol Neurosurg 1986;88:3-17
30. Wolf PA, Kannel WB, McGee DL: Prevention of ischemic
stroke: Risk factors, in Barnett HJM, Stein BM, Mohr JP,
Yatsu FM (eds): Stroke. New York, Churchill Livingstone Inc,
1986, pp 967-988
31. Schulte BPM, Leyten ACM, Herman B: Differing aspects of
pre-stroke and post-stroke hypertension, in Stober T, Schimrigk K, Ganten D, Sherman DG (eds): Central Nervous System
Control of the Heart. Boston, Martinus Nijhoff Publishing,
1986, pp 145-152
32. Hart RG: Prevention and treatment of cardioembolic stroke,
in Furlan AJ (ed): The Heart and Stroke. London, SpringerVerlag, 1987, pp 117-138
33. Bladin PF, Berkovic SF: Striato-capsular infarction: Large
infarcts in the lenticulo-striate arterial territory. Neurology
1984^4:1423-1430
34. Santamaria J, Graus F, Rubio F, Arbizu T, Peres J: Cerebral
infarction of the basal ganglia due to embolism from the heart
Stroke 1983;14:911-914
35. Sandok BA: Evaluation of patients with suspected cardioembolic brain infarction, in Furlan AJ (ed): The Heart and Stroke.
London, Springer-Verlag, 1987, p 37
36. Loeb C, Gandolfo C, Mancardi GL, Primavera A, Tassinari T:
The lacunar syndromes: A review with personal contribution,
Lodder et al
in Lechner H, Meyer JS, Ott E (eds): Cerebrovascular Disease:
Research and Clinical Management. Amsterdam, Elsevier Science Publishing Co Inc, 1986, vol 1, pp 107-156
37. Gandolfo C, Capanetto C, Del Sotte M, Santoloci D, Loeb C:
Risk factors in lacunar syndromes: A case control study. Ada
Neurol Scand 1988;77:22-26
38. Kappelle LJ, Koudstaal PJ, van Gijn J, Ramos LMP, Keunen
JEE: Carotid angiography in patients with lacunar infarction:
A prospective study. Stroke 1988;19:1093-1096
Risk Factors for Cerebral Infarction
381
39. Norrving B, Cronqvist S: Clinical and radiologic features of
lacunar versus nonlacunar minor stroke. Stroke 1988;19:59-64
40. Harrison MJG, Marshall J: Arteriographic comparison of
amaurosis fugax and hemispheric transient ischaemic attacks.
Stroke 1985;16:795-797
KEY WORDS • embolism • hypertension • lacunar infarction
• risk factors
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Are hypertension or cardiac embolism likely causes of lacunar infarction?
J Lodder, J M Bamford, P A Sandercock, L N Jones and C P Warlow
Stroke. 1990;21:375-381
doi: 10.1161/01.STR.21.3.375
Downloaded from http://stroke.ahajournals.org/ by guest on September 30, 2016
Stroke is published by the American Heart Association, 7272 Greenville Avenue, Dallas, TX 75231
Copyright © 1990 American Heart Association, Inc. All rights reserved.
Print ISSN: 0039-2499. Online ISSN: 1524-4628
The online version of this article, along with updated information and services, is located on the
World Wide Web at:
http://stroke.ahajournals.org/content/21/3/375
Permissions: Requests for permissions to reproduce figures, tables, or portions of articles originally published in
Stroke can be obtained via RightsLink, a service of the Copyright Clearance Center, not the Editorial Office.
Once the online version of the published article for which permission is being requested is located, click Request
Permissions in the middle column of the Web page under Services. Further information about this process is
available in the Permissions and Rights Question and Answer document.
Reprints: Information about reprints can be found online at:
http://www.lww.com/reprints
Subscriptions: Information about subscribing to Stroke is online at:
http://stroke.ahajournals.org//subscriptions/