Sustained ventricular tachycardia or fibrillation in the cardiac
advertisement

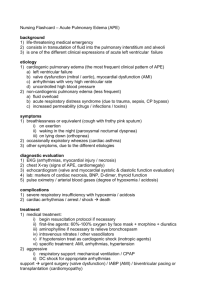
Journal of the American College of Cardiology © 2004 by the American College of Cardiology Foundation Published by Elsevier Inc. Vol. 43, No. 10, 2004 ISSN 0735-1097/04/$30.00 doi:10.1016/j.jacc.2003.09.072 Beta-Blockers in Myocardial Infarction Sustained Ventricular Tachycardia or Fibrillation in the Cardiac Catheterization Laboratory Among Patients Receiving Primary Percutaneous Coronary Intervention Incidence, Predictors, and Outcomes Rajendra H. Mehta, MD, MS,* Kishore J. Harjai, MD,† Lorelei Grines, PHD,† Gregg W. Stone, MD,‡ Judy Boura, MS,† David Cox, MD,§ William O’Neill, MD,† Cindy L. Grines, MD,† on behalf of the Primary Angioplasty in Myocardial Infarction (PAMI) Investigators Ann Arbor and Royal Oak, Michigan; New York, New York; and Charlotte, North Carolina We sought to evaluate the incidence, predictors, and outcomes of ventricular tachycardia and/or ventricular fibrillation (VT/VF) in the cardiac catheterization laboratory among patients undergoing primary percutaneous coronary intervention (PCI). BACKGROUND Although VT/VF has been known to occur during primary PCI, the current data do not identify patients at risk for these arrhythmias or the outcomes of such patients. METHODS We evaluated 3,065 patients enrolled in the Primary Angioplasty in Myocardial Infarction (PAMI) trials, who underwent primary PCI to evaluate the associations of VT/VF and the influence of these arrhythmias on in-hospital and one-year outcomes. RESULTS In patients undergoing primary PCI, VT/VF occurred in 133 (4.3%). Multivariate analysis identified the following as independent correlates of VT/VF: smoking (odds ratio [OR] 1.95, 95% confidence interval [CI] 1.26 to 3.02), lack of preprocedural beta-blockers (OR 2.34, 95% CI 1.35 to 4.07), time from symptom onset to emergency room of ⱕ180 min (OR 2.63, 95% CI 1.42 to 4.89), initial Thrombolysis In Myocardial Infarction (TIMI) flow grade 0 (OR 2.06, 95% CI 1.23 to 3.47), and right coronary artery-related infarct (OR 1.93, 95% CI 1.25 to 2.99). Although patients with VT/VF had a higher incidence of bradyarrhythmias, hypotension, cardiopulmonary resuscitation, and endotracheal intubation in the catheterization laboratory, their in-hospital and one-year adverse outcomes were similar to those of the cohort without these arrhythmias. CONCLUSIONS Our findings suggest that the incidence of VT/VF during primary PCI is low, indicating that these arrhythmias do not influence PCI success or in-hospital or one-year outcomes. Our data further help identify patients at risk of VT/VF during primary PCI and suggest that pretreatment with beta-blockers should be strongly considered to reduce these arrhythmias. (J Am Coll Cardiol 2004;43:1765–72) © 2004 by the American College of Cardiology Foundation OBJECTIVES Many studies have investigated the clinical and angiographic correlates and the prognostic significance of sustained ventricular tachycardia and/or ventricular fibrillation (VT/VF) after thrombolytic therapy in patients with STsegment elevation myocardial infarction (STEMI) (1– 6). See page 1788 Some of these investigations have suggested that these ventricular arrhythmias are associated with coronary reperfusion, although others have related them to suboptimal From the *University of Michigan, Ann Arbor, Michigan; †William Beaumont Hospital, Royal Oak, Michigan; ‡Lenox Hill Hospital, New York, New York; and §Mid Carolina Cardiology, Charlotte, North Carolina. Manuscript received June 17, 2003; revised manuscript received August 27, 2003, accepted September 8, 2003. Downloaded From: https://content.onlinejacc.org/ on 09/30/2016 reperfusion (1– 6). The occurrence of VT/VF after thrombolysis has been shown to be associated with an increased risk of in-hospital and one-year adverse events (6). However, much less is known about the incidence, risk factors, and prognosis of sustained VT/VF occurring in the cardiac catheterization laboratory in patients with STEMI undergoing primary percutaneous coronary intervention (PCI). It is unclear how the rapid reperfusion achieved with primary PCI (with an associated rapid change in the metabolic cellular milieu, resulting in regional electrophysiologic instability), on the one hand, and the more complete reperfusion, on the other (7–10), influence the propensity and outcomes of these arrhythmias after primary PCI. The purpose of the current investigation was to examine the incidence, predictors, and outcomes of VT/VF occurring in the cardiac catheterization laboratory among patients undergoing primary PCI. 1766 Mehta et al. Ventricular Arrhythmias Treated With Primary PCI Abbreviations and Acronyms CI ⫽ confidence interval ECG ⫽ electrocardiogram/electrocardiographic OR ⫽ odds ratio PAMI ⫽ Primary Angioplasty in Myocardial Infarction trial PCI ⫽ percutaneous coronary intervention RCA ⫽ right coronary artery STEMI ⫽ ST-segment elevation myocardial infarction TIMI ⫽ Thrombolysis In Myocardial Infarction VF ⫽ ventricular fibrillation VT ⫽ ventricular tachycardia METHODS Patient population. We pooled the data on 3,065 patients enrolled in the four Primary Angioplasty in Myocardial Infarction (PAMI) studies (including two trials with their concomitant registries) that collected prospective data on complications occurring in the cardiac catheterization laboratory (7,11–15). The rationale, methodology, and results of the individual PAMI studies have been previously published (7,11–15). Patients were included in these investigations if they were ⱖ18 years old with STEMI presenting within 12 h of their symptom onset. Acute STEMI was defined as ST-segment elevation of at least 1 mm in two or more contiguous leads or presumed new left bundle branch block on the presenting 12-lead electrocardiogram (ECG) in the presence of chest pain and/or elevation of cardiac enzymes. Patients were excluded from these trials if they had contraindications to reperfusion, had received thrombolytic therapy for index STEMI, or had renal failure, cardiogenic shock, or a life expectancy ⬍1 year; those with child-bearing potential; or those with known contraindications to aspirin, heparin, or ticlopidine in later PAMI trials (11,14,15). Furthermore, patients randomized to the thrombolytic arm in PAMI-1 were also excluded from this analysis (7). Informed consent was obtained from all patients by the study investigators at the respective institutions. Data collection and angiographic analyses. A research coordinator at each site collected data prospectively on prespecified data elements on a case-report form in all trials. These data included baseline demographics, medical history (as reported by the patients, their families, or their referring physicians, or determined from their previous medical records), medications, procedures, complications, and clinical events. Follow-up was obtained at one year by a telephone interview or follow-up visit to the physician. Completed case-report forms were sent to the coordinating site at Beaumont Hospital, Royal Oak, Michigan, where the data were entered into an Access data base. The cineangiograms obtained at the time of the index intervention were analyzed at the core laboratory site, where coronary anatomy, Thrombolysis In Myocardial Infarction (TIMI) flow Downloaded From: https://content.onlinejacc.org/ on 09/30/2016 JACC Vol. 43, No. 10, 2004 May 19, 2004:1765–72 grades, percent diameter stenosis, left ventricular ejection fraction, and angiographic outcomes of the intervention were assessed. Definitions, group comparisons, and study end points. We categorized the study patients into two groups: those with and those without sustained VT/VF occurring in the cardiac catheterization laboratory during primary PCI. Ventricular fibrillation was defined as irregular undulations of varying contour and amplitude on the ECG, with absent distinct QRS and T waves and hemodynamic compromise requiring direct-current defibrillation (Fig. 1A). Sustained VT was defined as a regular wide-complex tachycardia of ventricular origin lasting ⱖ30 s and/or accompanied by hemodynamic compromise requiring electrical cardioversion or anti-arrhythmic therapy (Fig. 1B). Re-infarction was defined as recurrent symptoms or development of new ECG changes accompanied by new elevation of creatine kinase, MB enzyme levels. Ischemia-driven target vessel revascularization was defined as PCI or coronary artery bypass graft surgery of the index infarct-related artery prompted by symptoms or objective evidence of ischemia. Sustained hypotension was defined as systolic blood pressure ⬍80 mm Hg that was unresponsive to intravenous fluids, requiring vasopressors for ⬎1 h or an intra-aortic balloon pump. For this study, we compared the baseline clinical characteristics, patient demographic features, coronary angiographic findings, and in-hospital adverse events of the two comparison groups. The principal outcomes of interest included differences in the in-hospital and one-year mortality rates and the in-hospital and one-year incidence of major adverse cardiovascular events (defined as death, or re-infarction, or ischemic target vessel revascularization) between these two groups. Statistical analysis. Summary statistics are presented as frequencies and percentages or as median values. Comparisons between the two study groups were made using the two-tailed Wilcoxon rank-sum test for continuous variables and the chi-square or Fisher exact test (when the expected frequency count in a cell was ⬍5) for categorical variables, as appropriate. In all cases, denominators reflect cases reported. Stepdown multivariate logistic regression was constructed to identify clinical predictors of sustained VT/VF, using variables showing a marginal association with it on univariate testing (p ⬍ 0.10). Only variables with a significant (p ⬍ 0.05) association with sustained VT/VF were included in the final regression models. Adjusted odds ratios (ORs) and accompanying 95% confidence intervals (CIs) were computed to determine the effect of each variable on the risk of VT/VF in the final model. Diagnostic routines (the Hosmer-Lemeshow test for lack of fit and the likelihood ratio test) were used for the final model selection. The c statistic was calculated to evaluate model discrimination. The Cochran-Mantel-Haenszel test was used for the analysis of trend. The software SAS version 8.0 (SAS Institute, Cary, North Carolina) was utilized for all analyses. JACC Vol. 43, No. 10, 2004 May 19, 2004:1765–72 Mehta et al. Ventricular Arrhythmias Treated With Primary PCI 1767 Figure 1. Electrocardiographic tracings of ventricular fibrillation (A) and ventricular tachycardia (B) during primary percutaneous coronary intervention. Downloaded From: https://content.onlinejacc.org/ on 09/30/2016 1768 Mehta et al. Ventricular Arrhythmias Treated With Primary PCI JACC Vol. 43, No. 10, 2004 May 19, 2004:1765–72 Table 1. Baseline Characteristics of Study Patients Mean age (yrs) Age ⱖ70 yrs Females Onset of symptom to ER (min) ER to balloon time (min) Medical history Previous angina Previous myocardial infarction Previous congestive heart failure Diabetes Hypertension Previous stroke Hyperlipidemia Peripheral vascular disease Current smoker Previous PCI Previous CABG COPD Presentation Pulse (beats/min) Pulse ⬎100 beats/min Systolic blood pressure (mm Hg) Systolic blood pressure ⬍100 mm Hg Killip class ⬎I Medications before PCI Aspirin Heparin Ticlopidine Beta-blockers No VT/VF Group (n ⴝ 2,932) VT/VF Group (n ⴝ 133) p Value 61 ⫾ 12 718 (25%) 780 (27%) 164 ⫾ 175 (111) 143 ⫾ 161 (113) 58 ⫾ 12 25 (19%) 33 (25%) 116 ⫾ 89 (89) 145 ⫾ 119 (120) 0.057 0.13 0.64 0.014 0.27 451 (15%) 425 (14%) 55 (1.9%) 479 (16%) 1,349 (46%) 154 (5.3%) 1,018 (35%) 167 (5.7%) 1,207 (41%) 272 (9.3%) 125 (4.3%) 78 (2.7%) 21 (16%) 17 (13%) 4 (3%) 15 (11%) 55 (41%) 6 (4.5%) 52 (39%) 6 (4.5%) 72 (54%) 13 (9.8%) 3 (2.3%) 1 (0.8%) 0.76 0.56 0.32* 0.12 0.33 0.72 0.42 0.57 0.0024 0.84 0.29* 1.00* 87 ⫾ 20 512 ⫾ 19 114 ⫾ 25 675 ⫾ 26 322 ⫾ 11.2 86 ⫾ 21 26 ⫾ 23 107 ⫾ 22 46 ⫾ 40 15 ⫾ 11.7 0.95 0.38 0.0015 0.0011 0.84 2,425 (83%) 2,074 (71%) 1,066 (36%) 854 (29%) 102 (77%) 82 (62%) 29 (22%) 19 (14%) 0.036 0.044 0.26 0.0003 *Derived using the Fisher exact test. Data are presented as the mean ⫾ SD (median) value or number (%) of subjects. CABG ⫽ coronary artery bypass grafting; COPD ⫽ chronic obstructive pulmonary disease; ER ⫽ emergency room; PCI ⫽ percutaneous coronary intervention; SD ⫽ standard deviation; VF ⫽ ventricular fibrillation; VT ⫽ ventricular tachycardia. RESULTS Clinical and angiographic characteristics of patients with and without VT/VF (Tables 1 and 2). Of the 3,065 patients with STEMI undergoing primary PCI in the study, 133 (4.3%) had VT/VF during the procedure. The majority of patients with VT/VF required cardioversion/defibrillation (79%), whereas anti-arrhythmic drugs were used to restore sinus rhythm in the remaining patients. Compared with the cohort without VT/VF, those with these arrhythmias were more likely to be current smokers, with a trend toward being of younger age. Other patient demographics and medical history were similar in the two groups. The time from symptom onset to emergency room presentation was shorter in the group with VT/VF, with no difference in the door-to-balloon time. Systolic blood pressure on arrival was lower in patients with VT/VF. Aspirin, heparin, and betablockers were given less frequently before arriving at the cardiac catheterization laboratory in patients with VT/VF. As a result, the first activated clotting time in the catheterization laboratory was significantly lower in these patients. Important differences also existed in the angiographic characteristics between the two groups. Patients with VT/VF were more likely to have initial TIMI flow grade 0, higher initial percent stenosis of the infarct-related artery, Downloaded From: https://content.onlinejacc.org/ on 09/30/2016 and the right coronary artery (RCA) as their infarct artery. The postprocedural final percent stenosis and non–flowlimiting infarct artery dissection were higher in patients with VT/VF, with no difference between other postprocedural angiographic features, such as TIMI flow rates or the presence of thrombus. Complications in the catheterization laboratory, in the hospital, and at one-year follow-up in patients with and without VT/VF (Tables 2 and 3). Patients with VT/VF had a significantly higher incidence of bradyarrhythmias, hypotension, cardiopulmonary resuscitation, and the need for endotracheal intubation in the catheterization laboratory. Despite this, neither the mortality in the catheterization laboratory nor the in-hospital or one-year adverse outcomes differed between the two groups. The median length of stay was a day longer in the VT/VF group. Clinical factors related to VT/VF (Table 4). Stepdown logistic regression analysis identified current smoking, shorter time from symptom onset to emergency room presentation, lack of beta-blocker therapy in the emergency room, RCA-related STEMI, and lower TIMI flow grades on admission as independent correlates of VT/VF. By imputing the presence or absence of these risk variables for VT/VF in a patient (yes ⫽ 1; no ⫽ 0) into the equation JACC Vol. 43, No. 10, 2004 May 19, 2004:1765–72 Mehta et al. Ventricular Arrhythmias Treated With Primary PCI 1769 Table 2. Angiographic Data and Catheterization Laboratory Complications of Study Patients Initial angiographic data Infarct-related artery LMCA LAD LCx RCA Bypass graft Multivessel disease TIMI flow grade 0 1 2 3 Percent stenosis LVEF (%) Medications, IABP, and stent use during procedure Glycoprotein IIb/IIIa inhibitors Thrombolytics Stents IABP Initial activated clotting time (s) Postprocedural angiographic data TIMI flow grade 0 1 2 3 Percent stenosis Thrombus Final dissection Catheterization laboratory complications Bradyarrhythmias Cardiopulmonary resuscitation Endotracheal intubation Hypotension Death No VT/VF Group (n ⴝ 2,932) VT/VF Group (n ⴝ 133) 18 (0.6%) 1,111 (37.8%) 431 (14.7%) 1,199 (40.8%) 39 (1.3%) 1,414 (48.2%) 1 (0.8%) 38 (28.6%) 15 (11.3%) 77 (57.9%) 0 53 (40%) 1,754 (59.8%) 332 (11.3%) 419 (14.3%) 324 (11%) 97.4 ⫾ 7 (100) 49 ⫾ 12 105 (78.9%) 7 (5.3%) 12 (9%) 8 (6%) 98.7 ⫾ 4 (100) 50 ⫾ 12 62 (2.1%) 125 (4.3%) 894 (31%) 38 (1.3%) 234 ⫾ 159 5 (3.7%) 10 (7.5%) 35 (26.3%) 5 (3.7%) 167 ⫾ 182 39 (1.3%) 21 (0.7%) 137 (4.6%) 2,417 (82.4%) 16 ⫾ 18 (10) 247 (8.4%) 341 (11.6%) 0 0 6 (4.5%) 123 (92.5%) 18 ⫾ 15 (20) 18 (13.5%) 29 (21.8%) 0.22 0.024 0.24 0.018 281 (9.6%) 13 (0.4%) 20 (0.7%) 141 (4.8%) 3 (0.1%) 46 (34.6%) 8 (6%) 6 (4.5%) 21 (15.8%) 1 (0.7%) ⬍ 0.0001 ⬍ 0.0001 ⬍ 0.0018 ⬍ 0.0001 0.19* p Value 0.018 0.23 0.0002 0.068 0.0008 0.0007 0.51 0.40 0.28 0.30 0.16 ⬍ 0.0001 *Derived using the Fischer exact test. Data are presented as the number (%) of subjects or mean ⫾ SD (median) value. IABP ⫽ intra-aortic balloon pump; LAD ⫽ left anterior descending coronary artery; LCx ⫽ left circumflex artery; LMCA ⫽ left main coronary artery; LVEF ⫽ left ventricular ejection fraction; RCA ⫽ right coronary artery; TIMI ⫽ Thrombolysis In Myocardial Infarction; VF ⫽ ventricular fibrillation; VT ⫽ ventricular tachycardia. shown in the Appendix and solving this equation, an estimate of the absolute risk of VT/VF in an individual patient during primary PCI can be obtained. The frequency of VT/VF increased as the time from symptom onset to emergency room arrival decreased (Fig. 2). Also, the frequency of VT/VF increased as the number of risk predictors increased: from none in patients with no risk factors to 12.6% in those with all five risk variables (Fig. 3). DISCUSSION Findings of the present study. Our study suggests that VT/VF occurs infrequently in the cardiac catheterization laboratory in patients undergoing primary PCI and identifies clinical and angiographic factors associated with this adverse event. Importantly, it shows that although the occurrence of VT/VF during primary angioplasty is associated with a greater length of stay, it does not have an impact Downloaded From: https://content.onlinejacc.org/ on 09/30/2016 on the procedural success or risk of adverse in-hospital and long-term outcomes. Thus, our study findings are in contrast to those of large trials evaluating VT/VF in patients with STEMI receiving thrombolytic therapy, which have reported a higher incidence of up to 20% and a greater risk of adverse short- and long-term outcomes with this arrhythmia (1– 6). Previous studies have shown that the size of myocardial infarction not only correlates with an increased incidence of VT/VF, but is also an important predictor of mortality in patients with STEMI (5,6,16 –18). Compared with thrombolysis, primary PCI is associated with greater myocardial salvage, a smaller infarct size, and a better ejection fraction (7–10). In patients treated with thrombolytic therapy, failed reperfusion is more common in the cohort with VT/VF than in those without these arrhythmias (6). Primary PCI is associated with not only more complete reperfusion (and fewer patients with TIMI flow grade 0), but also rapid reperfusion 1770 Mehta et al. Ventricular Arrhythmias Treated With Primary PCI JACC Vol. 43, No. 10, 2004 May 19, 2004:1765–72 Table 3. In-Hospital Complications and Long-Term Outcomes In-hospital events Bradyarrhythmias Pulmonary edema Sustained hypotension Cardiopulmonary resuscitation Need for dialysis CABG Gastrointestinal bleeding Median length of stay (days) In-hospital outcomes Re-infarction Ischemic TVR Death MACE Disabling stroke One-year outcomes Re-infarction Ischemic TVR Death MACE Disabling stroke No VT/VF Group (n ⴝ 2,932) VT/VF Group (n ⴝ 133) p Value 71 (2.4%) 80 (2.7%) 106 (3.6%) 19 (0.6%) 13 (0.4%) 245 (8.3%) 63 (2.1%) 5 7 (5.3%) 7 (5.3%) 9 (6.7%) 0 0 7 (5.2%) 4 (3%) 6 0.080 0.23 0.23 1.00* 1.00* 0.23 0.34* 0.019 33 (1.1%) 87 (2.9%) 84 (2.9%) 182 (6.2%) 6 (0.2%) 1 (0.8%) 7 (5.3%) 4 (3.0%) 11 (8.3%) 0 1.00* 0.12 0.79 0.34 1.00* 97 (3.3%) 312 (10.6%) 163 (5.5%) 528 (18%) 12 (0.4%) 3 (2.2%) 18 (13.5%) 6 (4.5%) 24 (18%) 0 1.00* 0.09 0.72 0.75 1.00* *Derived using the Fisher exact test. Data are presented as the number (%) of subjects. CABG ⫽ coronary artery bypass graft; MACE ⫽ major adverse cardiovascular events (re-infarction, or ischemia driven TVR or death); TVR ⫽ target vessel revascularization; other abbreviations as in Table 1. (7–10). Thus, it is not surprising that unlike previous reports of VT/VF occurring after thrombolysis (1– 6), the incidence of ventricular arrhythmias occurring with primary PCI is low and does not increase the risk of in-hospital and long-term mortality. Clinical and angiographic factors associated with the risk of VT/VF in patients undergoing primary PCI. Our study identified several clinical and angiographic variables as independent predictors of VT/VF in the cardiac catheterization laboratory during primary PCI. These included a history of current smoking, time from symptom onset to emergency room arrival, lack of beta-blocker therapy in the emergency room, RCA-related infarct, and initial TIMI flow grade 0 of the infarct-related artery. Nicotine stimulates catecholamine release and increases the heart rate and blood pressure (19). An increased level of carbon monoxide in smokers further reduces myocardial Figure 2. Time from symptom onset to emergency room (ER) arrival and frequency of ventricular tachycardia/ventricular fibrillation (VT/VF). The Cochran-Mantel-Haenszel statistic ⫽ 9.2, df 1, p ⬍ 0.0024 for trend. oxygen delivery (20). In addition, smoking has been shown to injure endothelial cells (21) and reduce prostacyclin production (22). These effects induce coronary vasospasm of both epicardial and myocardial resistance vessels, particularly in diseased coronary arteries. Smokers are also more likely to be younger—a population that is likely to have greater catecholamine surge with stress, as compared with elderly patients. Thus, both increased catecholamine levels and a greater propensity for vasospasm may make smokers particularly susceptible to VT/VF after primary PCI, which leads to rapid electrophysiologic instability of the myocardium. The speed of reperfusion has been shown to increase the rate of reperfusion arrhythmias. In animal studies, brief periods (5 to 15 min) of coronary artery occlusion followed by reperfusion are often associated, at the time of reflow, with dramatic increase in ventricular arrhythmias (23,24). If the duration of ischemia is extended to 1 to 3 h, followed by reperfusion, ventricular arrhythmias may still be present during the phase of ischemia, but reperfusion is not associated with as dramatic an increase in VT/VF (25). Clinical data support these preliminary animal observations. A pooled analysis of intracoronary thrombolysis trials suggests that VT/VF was more likely to occur when the interval between the onset of infarction and thrombolytic therapy was short (25). Similarly, in patients receiving intravenous Table 4. Adjusted Odds Ratios of Clinical Variables Associated With the Risk of Ventricular Tachycardia or Fibrillation During Primary Percutaneous Coronary Intervention Outcome Current smoker No beta-blocker in the ER RCA as infarct artery Time from symptom onset to ER ⱕ180 min Initial TIMI flow grade 0 Odds Ratio 95% Confidence Interval p Value 1.95 2.34 1.93 2.63 1.26–3.02 1.35–4.07 1.25–2.99 1.42–4.89 0.0027 0.0026 0.0033 0.0022 2.06 1.23–3.47 0.0062 Model c statistic ⫽ 0.72; Hosmer-Lemeshow chi-square ⫽ 6.03; df 8; p ⫽ 0.64. ER ⫽ emergency room. Other abbreviations as in Tables 1 and 2. Downloaded From: https://content.onlinejacc.org/ on 09/30/2016 Figure 3. Increasing number of risk factors for ventricular tachycardia/ ventricular fibrillation (VT/VF) (as shown in Table 4) and the incidence of these arrhythmias. The Cochran-Mantel-Haenszel statistic ⫽ 50.7, df 1, p ⬍ 0.0001 for trend. JACC Vol. 43, No. 10, 2004 May 19, 2004:1765–72 thrombolysis, VT/VF was more likely to occur when the time to treatment was shorter (6,26). The inverse relationship of the time from symptom onset to emergency room and the risk of VT/VF in our study is thus consistent with these previous observations. The use of beta-blockers in patients with STEMI in the pre-thrombolysis era has been shown to be associated with a reduction in early mortality, cardiac rupture, and ventricular arrhythmias (27,28). This beneficial effect of betablockers in reducing the incidence of VT/VF was also shown in patients receiving thrombolytic therapy (6). Our data are consistent with these earlier observations and extend the paradigm of the benefits of beta-blockers to patients receiving primary PCI. Thus, previous studies and our investigation suggest that beta-blockers are not only useful in preventing ischemia-mediated VT/VF (in nonreperfused patients), but also in reducing the incidence of these arrhythmias. These findings argue in favor of routine use of early beta-blocker therapy for all patients with STEMI, including those receiving primary PCI, to reduce the incidence of VT/VF, as well as to improve outcomes. Similar to the finding in our investigation, the risk of VT/VF has been shown to increase in patients with STEMI related to the RCA, who are receiving thrombolytic therapy (5,6,18), even in those undergoing rescue angioplasty (29). Several potential mechanisms may be implicated in this increased risk of VT/VF during reperfusion of an infarct related to the RCA. Sudden reperfusion of the RCA increases vagal tone through the Bezold-Jarisch reflex, which, in turn, results in a marked compensatory increase in sympathetic tone (29). Further, RCA-related infarctions are more common among younger patients and smokers (30), individuals who are more likely to have markedly heightened sympathetic tone, particularly after stress such as STEMI. Finally, animal studies have demonstrated that the severity of ischemic injury governs the extent of reperfusion injury (23,24). The greater the degree of myocardial hypoperfusion, the greater is the rate of formation of free radicals with reperfusion, and hence the greater chance of reperfusion arrhythmias (31). An increased heart rate worsens the severity of ischemic injury, augmenting the incidence of reperfusion arrhythmias (32). Conversely, agents that reduce the heart rate (beta-blockers) decrease reperfusion arrhythmias (33). Our investigation concurs with these animal experiments in that VT/VF was more common in patients undergoing primary PCI who had more severe ischemia at the onset (those with TIMI flow grade 0), compared with those with a lesser severity of ischemia (TIMI flow grade ⱖ1). Also, patients with TIMI flow grade 0 are more likely to have true reperfusion arrhythmias, as opposed to those with partial flow (TIMI flow grade ⱖ1). Conclusions. Our study suggests that in patients undergoing primary PCI, VT/VF occurs infrequently in the cardiac catheterization laboratory and does not influence PCI success or in-hospital or one-year outcomes when treated Downloaded From: https://content.onlinejacc.org/ on 09/30/2016 Mehta et al. Ventricular Arrhythmias Treated With Primary PCI 1771 promptly. Our data further help identify clinical and angiographic variables associated with an increased risk of these arrhythmias during primary PCI and suggest that prophylactic treatment with beta-blockers may be the best strategy to prevent ventricular arrhythmias in patients undergoing primary PCI. Reprint requests and correspondence: Dr. Cindy L. Grines, William Beaumont Hospital, 3601 West 13 Mile Road, Royal Oak, Michigan 48073. E-mail: cgrines@beaumont.edu. REFERENCES 1. Zehender M, Utzolino S, Furtwangler A, et al. Time course and interrelation of reperfusion-induced ST changes and arrhythmias in acute myocardial infarction. Am J Cardiol 1991;68:1138 –42. 2. Gressin V, Louvard Y, Pezzano M, Lardouz H. Holter recording of ventricular arrhythmias during intravenous thrombolysis for acute myocardial infarction. Am J Cardiol 1992;69:152–9. 3. Six AJ, Louwerenburg JH, Kingma JH, et al. Predictive value of ventricular arrhythmias for patency of infarct-related coronary artery after thrombolytic therapy. Br Heart J 1991;66:143–6. 4. Buckingham TA, Devine JE, Redd RM, Kennedy HL. Reperfusion arrhythmias during coronary reperfusion therapy in man: clinical and angiographic correlations. Chest 1986;90:346 –51. 5. Berger PB, Ruocco NA, Ryan TJ, et al. Incidence and significance of ventricular tachycardia and fibrillation in the absence of hypotension or heart failure in acute myocardial infarction treated with recombinant tissue-type plasminogen activator: results from the Thrombolysis in Myocardial Infarction (TIMI) phase II trial. J Am Coll Cardiol 1993;22:1773–9. 6. Newby KH, Thompson T, Stebbins A, et al. Sustained ventricular arrhythmias in patients receiving thrombolytic therapy: incidence and outcomes. Circulation 1998;98:2567–73. 7. Grines CL, Browne KF, Marco J, et al., the Primary Angioplasty in Myocardial Infarction Study Group. A comparison of immediate angioplasty with thrombolytic therapy for acute myocardial infarction. N Engl J Med 1993;328:673–9. 8. Zijlstra F, de Boer MJ, Hoorntje JC, et al. A comparison of immediate coronary angioplasty with intravenous streptokinase in acute myocardial infarction. N Engl J Med 1993;328:680 –4. 9. Gibbons RJ, Holmes DR, Reeder GS, et al., the Mayo Coronary Care Unit in Catheterization Laboratory Groups. Immediate angioplasty compared with the administration of a thrombolytic agent followed by conservative treatment for myocardial infarction. N Engl J Med 1993;328:685–91. 10. The Global Use of Strategies to Open Occluded Coronary Arteries in Acute Coronary Syndromes (GUSTO-IIb) Angioplasty Substudy Investigators. A clinical trial comparing primary coronary angioplasty with tissue plasminogen activator for acute myocardial infarction. N Engl J Med 1997;336:1621–8. 11. Grines CL, Cox DA, Stone GW, et al., the Stent Primary Angioplasty in Myocardial Infarction Study Group. Coronary angioplasty with or without stent implantation for acute myocardial infarction. N Engl J Med 1999;341:1949 –56. 12. Stone GW, Marsalese D, Brodie BR, et al., the Second Primary Angioplasty in Myocardial Infarction (PAMI-II) Investigators. A prospective, randomized evaluation of prophylactic intraaortic balloon counterpulsation in high risk patients with acute myocardial infarction treated with primary angioplasty. J Am Coll Cardiol 1997;29:1459 – 67. 13. Grines CL, Marsalese D, Brodie B, et al., for the PAMI-II Investigators. Safety and cost effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. J Am Coll Cardiol 1998;31:967–72. 14. Stone GW, Brodie BR, Griffin JJ, et al. Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of PAMI Stent Pilot trial. J Am Coll Cardiol 1998;31:23–30. 15. Stone GW, Brodie BR, Griffin JJ, et al. Clinical and angiographic follow-up after primary stenting in acute myocardial infarction: the 1772 16. 17. 18. 19. 20. 21. 22. 23. 24. 25. 26. 27. 28. Mehta et al. Ventricular Arrhythmias Treated With Primary PCI Primary Angioplasty in Myocardial Infarction (PAMI) Stent Pilot trial. Circulation 1999;99:1548 –54. Tofler GH, Stone PH, Muller JE, et al. Prognosis after cardiac arrest due to ventricular tachycardia or ventricular fibrillation associated with acute myocardial infarction (the MILIS study). Am J Cardiol 1987; 60:755–61. Volpi A, Maggioni A, Franzosi MG, et al. In-hospital prognosis of patients with acute myocardial infarction complicated by primary ventricular fibrillation. N Engl J Med 1987;317:257–61. Maggioni AP, Zuanetti G, Franzosi MG, et al., on behalf of the GISSI-2 Investigators. Prevalence and prognostic significance of ventricular arrhythmias after acute myocardial infarction in the fibrinolytic era: GISSI-2 results. Circulation 1993;87:312–22. Cryer PE, Haymond MW, Santiago JV, Shah SD. Norepinephrine and epinephrine release and adrenergic mediation of smokingassociated hemodynamic and metabolic events. N Engl J Med 1976; 295:573–7. Wald N, Howard S, Smith PG, Kjeidsen K. Association between atherosclerotic diseases and carboxyhemoglobin levels in tobacco smokers. BMJ 1973;1:761–5. Zimmerman M, McGeachie J. The effect of nicotine on aortic endothelium: a quantitative ultrastructural study. Atherosclerosis 1987;63:33–41. Reinders JH, Brinkman HJ, van Mourik JA, de Groot PG. Cigarette smoke impairs endothelial cell prostacyclin production. Atherosclerosis 1986;6:15–23. Manning AS, Hearse DJ. Reperfusion-induced arrhythmias: mechanisms and prevention. J Mol Cell Cardiol 1984;16:497–518. Hale SL, Lange R, Alker KJ, Kloner RA. Correlates of reperfusion ventricular fibrillation in dogs. Am J Cardiol 1984;53:1397–400. Hagar JM, Kloner RA. Reperfusion arrhythmias: experimental and clinical aspects. The Age of Reperfusion 1990;2:1–5. Solomon SD, Ridker PM, Antman EM. Ventricular arrhythmias in trials of thrombolytic therapy for acute myocardial infarction: a meta-analysis. Circulation 1993;88:2575–81. The MIAMI Trial Research Group. Metoprolol In Acute Myocardial Infarction (MIAMI): a randomized placebo-controlled international trial. Eur Heart J 1985;6:199 –226. The First International Study of Infarct Survival (ISIS-1) Collaborative Group. Mechanisms for the early mortality reduction produced by Downloaded From: https://content.onlinejacc.org/ on 09/30/2016 JACC Vol. 43, No. 10, 2004 May 19, 2004:1765–72 29. 30. 31. 32. 33. beta-blockade started early in myocardial infarction: ISIS-1. Lancet 1988;1:921–3. Gacioch GM, Topol EJ. Sudden paradoxic clinical deterioration during angioplasty of the occluded right coronary artery in acute myocardial infarction. J Am Coll Cardiol 1989;14:1202–9. Barbash GI, Reiner J, White HD, et al. Evaluation of paradoxic beneficial effects of smoking in patients receiving thrombolytic therapy for acute myocardial infarction: mechanism of the ‘smokers paradox’ from the GUSTO-I trial, with angiographic insights. J Am Coll Cardiol 1995;26:1222–9. Bolli R, Patel BS, Jeroudi MO, et al. Demonstration of free radical generation in ‘stunned’ myocardium of intact dogs with the use of spin trap alpha-phenyl N-tert-butyl nitrone. J Clin Invest 1988;82:476 –85. Lederman SN, Wenger TL, Harrell FE, et al. Effects of different paced heart rates on canine coronary occlusion and reperfusion arrhythmias. Am Heart J 1987;113:1365–9. Miyazawa K, Fukuyama H, Komatsu E, et al. Effects of propranolol on myocardial damage resulting from coronary artery occlusion followed by reperfusion. Am Heart J 1986;111:519 –24. APPENDIX Calculation of predicted risk using patient data and logistic regression coefficients. To calculate the odds of risk of VT/VF during the procedure for an individual undergoing primary PCI: exp ([⫺5.7521] ⫹ [0.6690 ⫻ current smoker] ⫹ [⫺0.8504 ⫻ beta-blocker therapy in emergency room] ⫹ [0.6576 ⫻ RCA as infarct-related artery] ⫹ [0.9676 ⫻ time from symptom onset to emergency room arrival ⱕ180 min] ⫹ [0.7243 ⫻ initial TIMI flow grade 0]). In the equation, the risk variables in a patient undergoing primary PCI are entered as: present ⫽ 1; absent ⫽ 0. The predicted risk (probability) of VT/VF during primary angioplasty is calculated as: odds/(1 ⫹ odds).