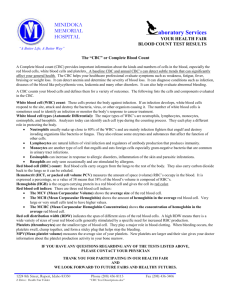
CBC Interpretation: Red & White Blood Cell Analysis
advertisement

The CBC: More Information Than You Thought JoAnn Deasy, PA-C. MPH San Francisco, CA jadeasy@sbcglobal.net Adjunct Lecturer Touro PA Program California Emergency Physicians Group Complete Blood Cell Count (CBC) Information • RBC, WBC & Platelets • Correct interpretation requires knowledge of the clinical significance of results as well as knowledge of the instruments producing the results Learning Objectives • Recognize information that can be gleaned from the electronic complete blood cell count (CBC) regarding red blood cells, white blood cells and platelets • Discuss how findings on the peripheral smear complement the electronic CBC • Correlate findings on the CBC to disease states Electronic Counters • Virtually all laboratories now use automated hematology instruments to generate the CBC • The Coulter Counter (Beckman) introduced automation in 1968 – 1977 platelets – 1983 leukocyte differential • Continued innovation in electronic hematology counters generating more reportable parameters 1 Electronic Counter Analytic Parameters • Excellent performance – WBC and RBC count – Hemoglobin concentration – Mean corpuscular volume (MCV) • Less satisfactory – Certain componets of the leukocyte differential count (LDC) – Platelet count at low concentrations • Caution Ordering a CBC • To diagnose anemia • To support a diagnosis of infection • To identify white blood cell disorders such as leukemia • To identify bleeding tendencies from low platelets • To determine the effects of chemotherapy and radiation therapy on blood cell production – Red cell distribution width (RDW) and mean platelet volume affected by time from blood draw to analysis 2 RED BLOOD CELL INFORMATION Red Blood Cell Information • Total RBC count • Hemoglobin / Hematocrit • RBC indices – Mean Corpuscular Volume (MCV) – Mean Corpuscular Hemoglobin (MCH) – Mean Corpuscular Hemoglobin Concentration (MCHC) – Red Cell Distribution Width (RDW) • Manual examination of peripheral smear RED BLOOD CELL COUNT • Number of RBC per µL – 4.5 to 6 million • Gender dependent – Interpret in conjunction with hemoglobin, hematocrit and rbc indices • Regulation by erythropoetin in kidney – Stimulus to produce erythropoetin include hypoxia, anemia, high altitude Red Blood Cell count • Causes of decrease – Anemia • Special situation of thalassemia minor – Excessive IV fluids • Causes of increase – Dehydration – Polycythemia vera – Secondary polycythemia 3 HEMOGLOBIN and HEMATOCRIT • Hemoglobin (Hgb): Oxygen carrying pigment of the rbc and best measure of the oxygen carrying capacity of the rbc. – Measured in grams per 100 ml Rule of Threes • Checks for artifacts – Hct = 3X hgb Hgb 10.7 g/dL – Hgb = 3X rbc count Hct 17.8% • Hematocrit (Hct): Measures packed RBC volume – expressed as % per fluid volume of whole blood MEAN CORPUSCULAR VOLUME (MCV) RBC Indices • Very accurate • Measurement of the size of the cell – 80-100 fL = normocytic cells – <80 fL = microcytic cells – >100 fL = macrocytic cells 4 MEAN CORPUSCULAR HEMOGLOBIN (MCH) • Measure of the average amount of hgb in an individual rbc – Reference range: 27-34 pg • Does not take into account the size of the rbc • Usefulness? – Small cells have less hemoglobin, large cells more, so variation in MCH tracks along with MCV. Adds little information independent of the MCV MCHC • Low MCHC = hypochromic • Normal MCHC = normochromic • High MCHC = hyperchromic MEAN CORPUSCULAR HGB CONCENTRATION (MCHC) • Relative value, average concentration of hgb in a red blood cell – Expressed as %, reference range 32-36% • or as g/dl of red cells (34 +/- 2 g/dl) • Very few conditions cause elevated MCHC – Spherocytosis – Cold agglutinin • Decreased MCHC – Iron deficiency, anemia of chronic disease, sideroblastic anemia RDW Red Cell Distribution Width • Indicates cell size variability - anisocytosis • Reference range: 11-14.5% • Elevated RDW: – Considerable variation in size of cells • RDW may be useful in separating IDA and thalassemia minor – Limited by wide distribution of RDW values within a given disease 5 EXAMINATION of PERIPHERAL SMEAR Peripheral Smear Examination of RBCs • Complements rbc indices and RDW • Size • Morphology – Shape and staining characteristics USING CBC to EVALUATE ANEMIA 1. Check hemoglobin/hematocrit – – 14-18 gms/100 ml men 12-16 gms/100 ml women DIFFERENTIAL DIAGNOSIS of MICROCYTIC ANEMIA • Iron deficiency anemia • Thalassemia • Anemia of chronic disease 2. Check MCV and classify anemia – – – Microcytic Normocytic Macrocytic • Sideroblastic anemias • Lead poisoning • Copper deficiency 6 Microcytic and Normocytic Anemias NORMOCYTIC ANEMIAS • Anemia of Chronic Disease • Hemolytic Anemia (or macrocytic) • Spherocytosis • Microcytic and normocytic anemias next step is to order iron studies MACROCYTIC ANEMIAS MCV > 100 Lab Findings in Microcytic Anemias Test MCV RDW Ferritin Iron TIBC % Sat Iron Def Thalassemia Low High Low Low Inc Low Low Normal Nl or Inc Normal Normal Normal Chronic Low or nl Normal Nl or Inc Low Low or nl Nl or low • • • • • • • • Alcohol Abuse and liver disease Vitamin B 12 Deficiency Folic Acid Deficiency Hemolytic Anemia Drug effects Hypothyroidism Myelodysplasia Idiopathic refractory sideroblastic anemia 7 Tests 16 year old Latin American girl comes to the office with her mother because mom thinks her daughter acts tired. Daughter says she feels fine. ROS is negative except for poor dietary habits (mostly fast food) and for history of heavy menses. Menses lasts 7 days. Menarch age 10. She has never had a pelvic examination. She is a junior in high school and says school is “boring” but she gets “okay” grades. Iron Studies Iron TIBC Ferritin 12 487 0 50-175 250-460 11-122 µg/dL µg/dL ng/mL WBC RBC Hgb Hct MCV MCH MCHC RDW Result 6.2 3.38 5.8 19.2 68 17.2 28.8 17.9 Reference Range 4.0-10.8 F 4.2-5.4 F 12-16 F 37-47 80-99 27-31 33-37 11.5-14.5 x103 x106 g/dL % fl pg % % 3+ microcytosis, 2+ anisocytosis, 3+ poikilocytosis, 3+ hypochromasia 36 year old Filipino woman comes to the office for a routine physical examination. Her past medical history includes mild anemia, that was never specifically diagnosed and was not treated. She reports having heavy menses. Her physical examination is unremarkable. 8 WBC RBC Hgb Hct MCV MCH MCHC RDW 4.9 6.21 10.7 34.8 56 17.2 30.6 14.3 4.8-10.8 F 4.2-5.4 F 12-16 F 37-47 80-99 27-31 33-37 11.5-14.5 x103 x106 g/dL % fl pg % % 3+microcytosis, 3+ hypochromasia moderate # target cells Further Studies Iron TIBC Ferritin 94 387 90 50-175 250-460 11-122 µg/dL µg/dL ng/mL Hemoglobin Electrophoresis Hgb A 89.5 95.8-98.5% Hgb F 2.8 0.0-2.0% Hgb A2 7.7 1.8-4.2 23 year old man with vague symptoms WBC RBC Hgb Hct MCV MCH MCHC RDW 3.8 3.91 10.7 32.7 84 27.3 33 13.5 4.0-10.8 M 4.7-6.1 M 14-18 M 42-52 80-99 27-31 33-37 11.5-14.5 x103 x106 g/dL % fl pg % % Iron TIBC Ferritin 22 230 300 50-175 250-460 11-122 µg/dL µg/dL ng/mL 9 TOTAL WBC COUNT • Leukocytosis = >11,000 WBC per / µL – Myeloproliferative disorders – Infection (especially bacterial) White Blood Cell Information from the CBC • Absent in 15-30% of cases – Tissue necrosis • Leukopenia = < 4,500 / µL Total WBC Count (4,500-11,000 / µl) Leukocyte (WBC) Differential – Relative and Absolute – Viral infection usually leukopenia or normal wbc – Drugs • Examples: clozaril, chemotherapeutic agents – Autoimmune disease – Aplastic anemia Automated Leukocyte Differential Count (LDC) • Movement to report only absolute values • Monocyte and basophil counts less reliable • Does not count bands or other immature granulocytes • When LDC abnormal and/or flags an eyecount differential should be performed – Diagnosis of certain infections – Leukemia – Anemia ABSOLUTE DIFFERENTIAL • • • • • • WBC PMNS LYMPHOCYTES MONOCYTES EOSINOPHILS BASOPHILS 6000 /µL 60% 28% 8% 3% 1% 6000 /µL 3600 (2000-6900) 1680 (600-3400) 480 (0-900) 180 (0-700) 60 (0-100) 10 Neutrophilia Neutropenia • Causes • Primary – Myeloid leukemia • Secondary – Bacterial infections • Associated bandemia – Tissue necrosis – Trauma – Drugs – glucocorticosteroids, epinephrine – Infection • Viral including HIV • Severe bacterial infections – Drugs – Autoimmune neutropenia – Chronic idiopathic neutropenia • Risk of Infection with Neutropenia (2000-6800/μL) – Minimal risk with ANC < 1500 – Moderate risk with ANC <1000 – Severe risk with ANC <500 Eosinophilia • Allergy – Hayfever, asthma – Drug hypersensitivity reactions CASE STUDIES • Parasitic infestation (non-protozoan) • Sarcoidosis and collagen vascular diseases • Malignancy (1%) – Hodgkin’s disease 11 20 YEAR OLD with SORE THROAT WBC Patient 1 Patient 1 Normal Patient 2 Patient 2 Absolute absolute 20,000 14,000 PMNs 93% LYMPHs 7% MONOs EOS BASO 0 0 0 18000 1400 20006800 10004000 100-800 0-200 24% 3360 70% 9800 5% 1% 0 700 140 42 YEAR OLD WOMAN with FEVER (103F) and LOW BACK PAIN WBC PMNs BANDS METAMYELOCYTES LYMPHOCYTES 7,410/μL 95% 5% 7,410 / µL 72% 20% 7% 1% APPENDICITIS – WBC COUNT Patient Ruptured WBC Count Neutrophilia 5 year old 18 year old 25 year old 27 year old 52 year old 30 year old Yes Yes No No No No 28,000 22,000 23,000 11,600 8,870 5,560 Yes Yes Yes Yes No No 65 year old man with fatigue and lymphadenopathy WBC PMNs BANDS LYMPHOCYTES MONOCYTES EOSINOPHILS BASOPHILS 40,000 / µl 15% 0 83% 1% 1% 0 (4,500-11,000) (45-70%) (0-5%) (25-44%) (0-12%) (1-8%) (0-2%) 12 PLATELET INFORMATION • Platelet count – Thrombocytopenia < 150,000 mm3 – Thrombocytosis > 600,000 mm3 • Mean platelet volume (MPV) – Indicates size (reference range 7.4-10.4 fl) • Thrombocytopenia and: – Large platelets → peripheral destruction – Small platelets → production defect SUMMARY - PEARLS New Parameters on Automated CBC Coming • Available newer machines can measure retiuclocytes and enumerate NRBCs • In the near future: – Extended differential count • Bands and other immature granulocytes, inc blasts • Atypical lymphocytes • Erythroblasts – Immature reticulocyte fraction – Fragmented red blood cells QUESTIONS ? • The automated CBC provides accurate, useful information re: rbc,wbc and platelets and newer technology will yield even more parameters • When anemia is present classify by MCV and then order further studies • WBC count and platelet count may direct you to consider or dismiss conditions, but there is no substitute for astute clinical judgment. 13