Use of Transparent Plastic Tubular Retractor in Surgery for Deep
advertisement

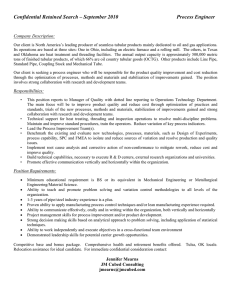
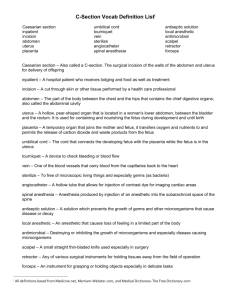
254 - Salvin Galley - 01 Surgical Overview SURGICAL TECHNOLOGY INTERNATIONAL XIX Use of Transparent Plastic Tubular Retractor in Surgery for Deep Brain Lesions: A Case Series SEBASTIAN R. HERRERA, M.D. NEUROSURGERY RESIDENT PELAGIA KOULOUMBERIS, M.D. NEUROSURGERY RESIDENT JOHN H. SHIN, M.D. NEUROSURGERY RESIDENT EDUARDO GOELLNER, M.D. NEUROSURGERY FELLOW MICHAEL CHAN, M.D. NEUROSURGERY RESIDENT KONSTANTIN V. SLAVIN, M.D. ASSOCIATE PROFESSOR DEPARTMENT OF NEUROSURGERY, UNIVERSITY OF ILLINOIS AT CHICAGO CHICAGO, ILLINOIS ABSTRACT B rain tissue retraction is frequently required to reach deep intra-axial lesions, and the quest for an ideal retractor that would protect the underlying brain tissue continues. Despite the availability of multiple retractors, the incidence of brain retraction injury remains high and has been reported to be 5% to 10%. A recently developed transparent tubular retractor appears to provide several advantages in surgery for deep intra-axial tumors and intracerebral hematomas. We used a new commercially available transparent tubular retractor in 16 craniotomies. Fourteen of these patients were operated upon for deep tumors and cysts, including two intraventricular tumors and two for deep intracerebral hemorrhages. In all patients, the tubular retractor was directed toward the lesion through a small corticotomy and guided by a navigation system. Each lesion was completely removed through the retractor's lumen. In all cases, the tubular retractors provided excellent visualization of the underlying pathology and facilitated its surgical removal, dissection, and hemostasis. The tubular nature of the retractor allowed the rotation and changing the angle of approach without putting extra pressure on the brain tissue, which inevitably occurs when malleable or other ribbontype retractors are used. There were no hematomas on routine postoperative CT scans in this series. Trans-1- 254 - Salvin Galley - 01 Use of Transparent Plastic Tubular Retractor in Surgery for Deep Brain Lesions: A Case Series HERRERA/SHIN/CHAN/KOULOUMBERIS/GOELLNER/SLAVIN parent tubular retractors provide a unique means of deep visualization and even force distribution at the retracted brain tissue. Although these retractors were originally designed for the removal of deep subcortical tumors, they may be used to access and evacuate intracerebral hematomas. In our experience, the use of tubular retractors allows one to achieve safe access to deep intracerebral lesions and decreases the rate of retraction-related complications. INTRODUCTION The issue of brain retraction has been repeatedly discussed in the neurosurgical literature. The damaging effect of the pressure put on the brain tissue during surgical exploration of various intracranial pathological processes is well known, with the incidence of postoperative intracerebral hemorrhages reaching 10% or greater, and therefore we and others routinely use multiple avenues aimed at the minimization of such potentially harmful retraction. 1 Among others, these include the development of approaches around the brain tissue, the release of cerebrospinal fluid by decompressing Figure 1. Schematic illustration of the tubular retractor assembly (left), the retractor itself (center), and the introducer (right). the cisterns or through a lumbar drain, the administration of diuretic and hyperosmotic agents, hyperventilation, and so on.2,3 However, all these measures do not eliminate the need for brain retraction, particularly if one has to reach deep intra-axial lesions such as neoplasms, vascular malformations, and hematomas. For this purpose, there are many commercially available retraction systems but most of them have their unique setbacks. For example, the standard flat malleable and tapered retractors do not confor m to the cur vature of the retracted tissue and are known to cause petechial hemorrhages along the retractor edge, presumably due to a sharp gradient of pressure between the retracted and surrounding tissues. To overcome this problem, several authors recently recommended using tubular retractor systems, some of which are designed for frame-based stereotactic applications (COMPASS; Compass, Inc., Rochester, MN) and some are adapted from extracranial applications (METRx; Medtronic, Minneapolis, MN). 4,5 Both of these tubular retractors are metal and do not allow visualization of the retracted tissue, creating another limitation for their wider acceptance. Here we present the technical aspects of a novel transparent tubular retractor that was specifically designed for intracranial applications and is commercially available worldwide. TECHNICAL TECHNICALDESCRIPTION DESCRIPTION Figure 2: Intraoperative photograph illustrating the simultaneous use of bipolar forceps and suction through the tubular retractor during tumor or hematoma removal. -2- According to its labeling, the ViewSite tubular brain retractor (Vycor Medical, Bohemia, NY) is specifically designed for intracranial applications. It is available in a variety of sizes representing different lengths and diameters suitable for different surgical procedures. It is made out of a 254 - Salvin Galley - 01 Surgical Overview SURGICAL TECHNOLOGY INTERNATIONAL XIX transparent plastic material and is individually packed in a sterile wrap, intended for a single use only. Each retractor assembly consists of two parts—the retractor and the introducer (Fig. 1). The retractor itself has a slightly tapered cylindrical shape with a circular or ovoid cross-section. Its outer edge is slightly wider and has a black outline over the clear plastic structure. The outer part of the retractor is attached to a flat plate (tab) that may be used for attachment to any of the widely used retraction arms or serve as a handle for manual insertion and manipulation. The introducer is also made of a transparent plastic material. It snugly fits into the retractor and sticks out a few millimeters from the distal opening of the retractor cylinder, tapering down to a very narrow flat surface that serves as a dissector when the retractor assembly is inserted into the brain. The distal tip of the introducer has a very small opening that allows the egress of cerebrospinal fluid or blood during the insertion process, and may also accommodate the tip of a pointing instrument when this retractor is used in association with an image-guidance system. The assembly is inserted into the brain through a small corticotomy either at the brain surface or in the depth of a cortical sulcus after the coagulation of superficial cerebral vessels and the sharp penetration of the pial membrane. The image-guidance probe may be used to facilitate the insertion of the retractor and confirm the direction of retractor advancement. The tapered shape of the assembly allows a smooth dissection of the brain tissue between the cerebral surface and the underlying deep lesion. The surface of the dissection corridor may be continuously monitored by visual observation due to transparent nature of the assembly. Once the lesion is reached, the introducer is removed and the opening in the distal end of the retractor allows one to obtain visualization of the surgical field without either absorption of light by the black surface of some retractors or reflection of light from metal surfaces of others. The direction of the retractor may then be adjusted during the course of lesion resection by changing the angulation of the device. Once the resection is completed, the retractor is removed by gently sliding out of the brain while checking Figure 3. Intraoperative photograph illustrating the manual control of the retractor by an assistant. the walls of the retraction corridor for bleeding. CLINICAL MATERIAL CLINICAL MATERIAL We started using transparent tubular retractors in May of 2007. Here we present our impressions from the first 16 consecutive uses of this device in intracranial surgical interventions. In two patients, a craniotomy was performed for the evacuation of deep intracerebral hematoma and one for drainage of a deep cyst, whereas thirteen other patients had intra-axial neoplasms. Of these, six were metastatic tumors, five were deep gliomas, and two were gangliogliomas. Figure 4: Intraoperative photograph illustrating the use of a tubular retractor in conjunction with a selfretaining retractor arm. -3- 254 - Salvin Galley - 01 Use of Transparent Plastic Tubular Retractor in Surgery for Deep Brain Lesions: A Case Series HERRERA/SHIN/CHAN/KOULOUMBERIS/GOELLNER/SLAVIN We used two models of the ViewSite retractor, 17 mm wide × 5 cm long and 21 mm wide × 5 cm long in eight cases each. The size of the retractor was chosen during the surgery based on the size of the underlying pathological process. Each of these retractors has an ovoid cross-section with width/height ratios of 17 mm × 11 mm and 21 mm × 15 mm, respectively. Both of these sizes allow the free manipulation of bipolar forceps, tumor forceps, and one or two suction tips by a surgeon and assistant working simultaneously (Fig. 2). The length of the retractor channel (5 cm) allows the reach of deep lesions when the retractor is inserted completely with its outer surface touching the cortex. In cases of more superficial lesions, the retractor may be inserted partially and held in place by an assistant (Fig. 3) or by a flexible arm of the retractor (Fig. 4). Intraoperative computer-assisted stereotactic image-guided navigation was used for the precise localization of the deep intracerebral lesion in all cases. In 10 cases, microsurgical dissection of the tumor tissue was perfor med with the assistance of an operative microscope; in three other tumors, the cyst and both hematomas, loupe magnification was used. In all cases, the lesions were removed without complications. Nine of the thirteen tumors were removed totally and four subtotally. In one of the cases, a ventricular catheter was inserted into the ventricular cavity through the retractor prior to its removal. This catheter was subsequently connected to a ventriculoperitoneal shunt. Postoperative computed tomography (CT) scans are routinely obtained in all our patients that undergo craniotomy. The hematoma evacuation and tumor resection were thereby confirmed in each case. There were no instances of postoperative hematoma in any of the cases reported here. Furthermore, tumor resection was confir med by postoperative magnetic resonance imaging (MRI) in all cases except one, who could not have MRI due to implanted cardiac pacemaker. DISCUSSION DISCUSSION New developments in brain retraction technology are dictated by the need to reduce risks and complications in elective brain surgery. Much has been written about the detrimental effects of excessive cerebral retraction but to date the ideal system that would make such retraction absolutely safe still does not exist.2,3 Recently, an attractive idea was introduced to replace standard flat or curved “blade” retractors with the tubular or cylindrical models. The pioneering work of Kelly and colleagues resulted in the development of cylindrical retractors that would be attached to a stereotactic apparatus to facilitate volumetric resection of intra-axial tumors.5 A similar device was later introduced by Otsuki et al., and then by Ross and by Barlas for use with a Leksell frame.6–8 Recently, Greenfield et al. suggested using cylindrical retractors designed for minimally invasive spine interventions for intracranial applications.4 Although revolutionary in thinking, neither of these two developments created an ideal retraction system, partially because the bulk of the retractor is its metal or hard plastic texture and the lack of transparency of the retractor walls resulted in limited acceptance of these devices by the neurosurgical community. At the same time, another pioneering innovation was aimed at developing a nonmetal transparent retraction device. Ogura et al. suggested using a transparent polyester film rolled into a cylinder to retract the brain tissue en route to the intracranial lesion.9 The limitations of this approach include difficulty in inserting the film-based retractor into the brain and the need for additional retractors to aim and hold the film in place. The tubular retractor described in this chapter combines the benefits of these two principles. It has enough sturdiness to be advanced to the target, with or without an image-guidance approach, and at the same time is less traumatic and completely transparent. We used two sizes of the retractor that were available at that time. Currently, the product line includes 12 sizes of ViewSite device with four transverse (larger) diameters (12 -4- mm, 17 mm, 21 mm, and 28 mm) and three lengths (3 cm, 5 cm, and 7 cm). This choice of retractors adds more versatility and would significantly increase their applicability in a variety of neurosurgical interventions. CONCLUSIONS CONCLUSIONS Transparent tubular retractors provide a unique means of deep visualization and even force distribution of the retracted brain tissue. Although these retractors were originally designed for the removal of deep subcortical tumors, they may be used to access and evacuate intracerebral hematomas. In our experience, the use of tubular retractors allows one to achieve safe access to deep intracerebral lesions and decrease the rate of retraction-related complications. STI REFERENCES REFERENCES 1. Fukumachi A, Koizumi H, Nukui H. Postoperative intracerebral hemorrhages: a survey of computed tomographic findings after 1074 intracranial operations. Surg Neurol 1985;23:575–80. 2. Andrews RA, Bringas JR. A review of brain retraction and recommendations for minimizing intraoperative brain injury. Neurosurgery 1993;33:1052–64. 3. Zhong J, Dujovny M, Perlin AR, et al. Brain retractor injury. Neurol Res 2003; 25:831–8. 4. Greenfield JP, Cobb WS, Tsouris AJ, Schwartz TH. Stereotactic minimally invasive tubular retractor system for deep brain lesions. Neurosurgery 2008;63(ONS Suppl 2):ONS 334–40. 5. Kelly PJ, Goerss SJ, Kall BA. The stereotaxic retractor in computer-assisted stereotaxic microsurgery. Technical note. J Neurosurg 1988;69:301–6. 6. Barlas O. A simple stereotactic retractor for use with the Leksell system. Neurosurgery 1994;34:380–1. 7. Otsuki T, Jokura H, Yoshimoto T. Stereotactic guiding tube for open-system endoscopy: a new approach for the stereotactic endoscopic resection of intra-axial brain tumors. Neurosurgery 1990;27:326–30. 8. Ross DA. A simple stereotactic retractor for use with the Leksell stereotactic system. Neurosurgery 1993;32:475–6. 9. Ogura K, Tachibana E, Aoshima C, Sumitomo M. New microsurgical technique for intraparenchymal lesions of the brain: transcylinder approach. Acta Neurochir (Wien) 2006;148:779–85.