Long-term behaviour of the Charnley offset
advertisement

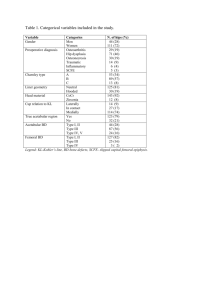
Long-term behaviour of the Charnley offset-bore acetabular cup Theologos T. Ioannidis, Nikolas Zacharakis, Evangelos A. Magnissalis, George Eliades, George Hartofilakidis From the University of Athens and the Research Centre for Biomaterials, Athens, Greece e report the long-term radiological results of 58 total hip arthroplasties (THA) using the Charnley offset-bore acetabular socket. Wear was measured at four sites and radiolucent lines and possible migration were recorded. Four cups were retrieved at revision and were examined using light microscopy, SEM and X-ray microanalysis. At a mean follow-up of seven years the mean wear in the DeLee and Charnley zone I was 0.4 mm and in zone II 0.26 mm. The wear rate was 0.06 and 0.04 mm/year, respectively. Progression of radiolucent lines was seen in five cases (8.6%). Three sockets (5.2%) were revised because of aseptic migration at a mean follow-up of 9.8 years and one socket for infection at two years. The offset-bore acetabular cup had excellent wear behaviour and a low migration and revision rate. We recommend that it should be considered in THA since the use of small cups is increasing, particularly in revision cases. W J Bone Joint Surg [Br] 1998;80-B:48-53. Received 12 June 1997; Accepted 5 August 1997 The Charnley extra small socket with a face diameter of 1 35 mm has an offset bore so that the cavity for the femoral head is placed eccentrically. The thickness of ultra-highmolecular-weight polyethylene (UHMWPE) is approximately 10 mm in the upper weight-bearing part, equal to that of conventional sockets, and then decreases to a few millimetres in the lower part (Fig. 1). We have used this acetabular component since 1976, T. T. Ioannidis, MD, Associate Professor N. Zacharakis, MD, Registrar G. Hartofilakidis, MD, FACS, Emeritus Professor of Orthopaedics Department of Orthopaedics, University of Athens, KAT Hospital, Kifissia 14561, Greece. E. A. Magnissalis, PhD, Bioengineer, Quality Control Section G. Eliades, DDS, D Odont, Head, Quality Control Section Research Centre for Biomaterials, Athens 16562, Greece. Correspondence should be sent to Professor G. Hartofilakidis at 21 Fotiou Patriarchou Street, Athens 11471, Greece. ©1998 British Editorial Society of Bone and Joint Surgery 0301-620X/98/18057 $2.00 48 mainly in patients with neglected high and low dislocations undergoing primary total hip arthroplasty (THA) as well as in a few revision cases. We now report the long-term results regarding acetabular wear, radiolucent lines, cup migration and the rate of loosening. Four retrieved acetabular sockets have also been examined by light microscopy and SEM and by X-ray microanalysis. Patients and Methods Between 1973 and 1992 a total of 702 THAs were performed by the senior authors (GH and TTI) using the 1 Charnley low-friction arthroplasty (LFA) technique. Since 1976, 72 offset-bore sockets have been used in 54 patients. Seven cases have been lost to follow-up. In six hips (four patients) the immediate postoperative radiographs were either missing or of very poor quality and they were excluded. One Girdlestone procedure, performed because of infection in the second postoperative year, was also excluded. This left 58 hips (42 patients) in the study with a mean follow-up of seven years (3 to 19). Most of the cases 2,3 were high dislocations (Table I). All the patients were women with a mean age of 48.4 years (23 to 68). In 44 hips (75.9%) offset-bore sockets had been used in combination with the cotyloplasty technique which has 2,3 been previously reported. This entails fracture of the floor of the original acetabulum, bone grafting, and controlled medialisation of the cemented cup. The current and immediate postoperative radiographs were evaluated independently by two examiners using a Vernier micrometer calliper with the 22.25 mm LFA femoral head as a guide for the correction of magnification. There were almost no interobserver differences in the measurements. When there were such differences they were small and the mean value was used. The thickness of the UHMWPE was measured according to Charnley and 4 5 Halley and Wroblewski at 30, 45, 90 and 150° from the upper rim of the cup. The mean value of wear at 30° and 45° was adopted as the zone-1 measurement so that the results corresponded to the three radiological zones of 6 DeLee and Charnley. The annual wear rate was calculated. We recorded the presence of radiolucent lines in the three 6 7 zones of DeLee and Charnley according to McCoy et al THE JOURNAL OF BONE AND JOINT SURGERY LONG-TERM BEHAVIOUR OF THE CHARNLEY OFFSET-BORE ACETABULAR CUP 49 Results Clinically, all 42 patients (58 hips) had well-functioning THAs and were rated high on the Merle d’Aubigné and 1 Postel scale as modified by Charnley (Figs 2 and 3). Radiological analysis showed no wear in five (8.6%) and minimal wear in three (5.2%) of our acetabular cups. In the rest, the mean wear in zone I was 0.4 mm and in zone II 0.26 mm. In zone III it was not possible to calculate wear since any wear in the other two zones results in enlargement of the apparent radiological ‘thickness’ of this area. The annual wear rate was 0.06 mm in zone I and 0.04 mm in zone II. There was a significant wear rate (> 0.13 mm/ annum) in only 12 THAs (20.7%). The most common site for maximal penetration in a single socket was the zone at 90° (44.8% of the sockets) followed by that at 45° (24.1%) and at 30° (17.2%). Details are given in Tables III to V. Table I. Details of the underlying pathology of the 58 THAs Fig. 1 The offset-bore acetabular socket. with grades from 0 to 4. Migration in the horizontal and vertical direction was measured using the interteardrop line as a guide and 2 mm as the lower limit. Progression of the lines was also noted. Analysis of the articular surface of the four retrieved implants included macroscopic inspection using a magnifying lens, light microscopy, SEM and wavelength-dispersive X-ray microanalysis (JXA 733 Super probe, Jeol Ltd, Tokyo, Japan). Table II gives the details of the retrieved implants. Congenital hip disease High dislocation Low dislocation Dysplasia Revision THA 44 8 3 3 Table II. Details of the examined retrieved acetabular sockets Number Months in situ Side Age at first operation (yr) 1 2 3 4 187 63 28 81 L L L L 40 30 41 66 Anteroposterior radiographs of a 37-year-old woman with high dislocation of the right hip preoperatively (a) and 19 years after THA with an offset-bore acetabular component (b). The clinical and radiological results were satisfactory and there was no migration. The direction of maximum penetration was found at 90° with total penetration of 1.46 mm (0.076 mm per annum). Fig. 2a VOL. 80-B, NO. 1, JANUARY 1998 Fig. 2b 50 T. T. IOANNIDIS, N. ZACHARAKIS, E. A. MAGNISSALIS, Fig. 3b Fig. 3c Table III. The mean wear (mm) in all three DeLee and Charnley zones for 58 TKAs at a mean follow-up of 84.4 months Wear I II III G. HARTOFILAKIDIS Anteroposterior radiographs of a 47-year-old woman with bilateral high dislocation. Figure 3a – Before operation. Figure 3b – Six years and four months after THA of the right hip with an offset-bore acetabular component combined with cotyloplasty. There was no migration. The direction of maximum penetration was found at 30°, with total penetration of 0.12 mm (0.018 mm per annum). Figure 3c – Six years and five months after THA of the left hip with an offset-bore acetabular component and a cotyloplasty. There was no migration. The direction of maximum penetration was found at 90°, with total penetration of 0.32 mm (0.049 mm per annum). Fig. 3a Zone G. ELIADES, Mean Table V. Incidence of maximum penetration in the measured sites for 58 TKAs Number % 10 14 26 17.2 24.1 44.8 Minimal wear* 3 5.2 No wear 5 8.6 SD -0.4 -0.26 0.09* 0.58 0.68 0.66 * apparent thickening Table IV. The mean annual wear rate (mm per annum) for all three zones for 58 TKAs Zone Mean wear rate I (30° to 45°) II (90°) III (150°) -0.06 -0.04 -0.02* Location (degrees) 30 45 90 * both the actual wear and the intersite differences were very small and undiscernible * apparent increase THE JOURNAL OF BONE AND JOINT SURGERY LONG-TERM BEHAVIOUR OF THE CHARNLEY OFFSET-BORE ACETABULAR CUP Table VI. Acetabular demarcation 7 according to McCoy et al Grade Number % 0 1 2 3 4 19 27 4 3 5 32.8 46.6 6.9 5.2 8.6 51 abular cup with the longest follow-up (187 months). There were scratches, gouges, shredding and pitting mainly at the upper load-bearing regions. Lower regions had polishing of the machining marks. SEM and X-ray microanalysis findings revealed crystalline formations in the lower region of the articular surfaces (Fig. 4). These crystals differed in appearance and composition from the adjacent area and were characterised by the presence of calcium and phosphorus. There was no significant demarcation around the cup; 46 7 (79.4%) were in grades 0 to 1 according to McCoy et al, (Table VI). Only five hips (8.6%) showed migration; in three it was progressive and they were subsequently revised. Two others were revised because of aseptic loosening of the stem. In both, the well-fixed acetabular cup showed excessive wear (> 1.13 mm). Revisions were performed at a mean of 9.8 years postoperatively (4 to 16). Macroscopic and microscopic changes in the retrieved 8,9 implants were similar to those previously reported. Discoloration and plastic deformation of the UHMWPE were observed macroscopically along the upper rim of the acet- The longevity of a THA depends on many factors, some of which are ‘surgeon-dependent’. Since UHMWPE debris has now been recognised to be a major factor in loosening of the prosthesis the acetabular part of an implant has 10-12 recently become the focus of attention. The thickness of the UHMWPE also plays an important role in its wear. It has been reported that thickness of 5 mm or less in metal13 backed sockets could lead to catastrophic results. This can be regulated by choosing the appropriate acetabular cup Fig. 4a Fig. 4b Discussion SEM and X-ray area scan images of crystalline formations observed at the lower region of retrieved components. Figure 4a – Backscattered electron image for composition (BEI-COMPO) showing crystalline formations of different composition from the surrounding polyethylene area. Figure 4b – Calcium area scan of image in Figure 4a. Figure 4c – Phosphorus area scan of image in Figure 4a (magnification 200; scale bar 100 m). Fig. 4c VOL. 80-B, NO. 1, JANUARY 1998 52 T. T. IOANNIDIS, N. ZACHARAKIS, E. A. MAGNISSALIS, and head diameter. In certain conditions and in some revision situations, a ‘shallow’ cup of a small diameter must be used, but even with a 22.2 mm head, the thickness of UHMWPE becomes critical. The offset cup gives almost standard thickness of UHMWPE in the upper weight1 bearing part of the socket. 14 Dennis and Halley have presented a preliminary report of nine cases in which this design of small acetabular cup was used and, recently, the first well-documented study on 15 54 THAs was reported from Wrightington Hospital. This gives a rate of 35% for no wear in a mean follow-up of 8.1 years which differs from our figure of 8.6, with a mean follow-up of seven years (or 13.7% if minimal wear is included). Our finding, however, of an annual wear rate of 0.06 and 0.04 mm per annum for zones I and II, respectively, is comparable with the Wrightington figure of 0.04 mm per annum overall. Many of our patients have the common underlying pathology of congenital hip disease and are a young and active group with a mean age of 48.4 years. Wear of UHMWPE depends on many factors such as the 16 mechanical roughness finish of the femoral head, the surface preparation of the UHMWPE, the method of sterilisation, the shelf life of the implant and finally the thick10 ness of the plastic. Implants of the non-conforming designs have been found to be more susceptible to 10,17-19 wear, but fatigue wear is unusual owing to the conformity of the two contacting surfaces. Our findings add to the evidence that conformity plays a very important role in the wear behaviour of UHMWPE 15 and agree with those of Izquierdo-Avino et al . The wear rates are considerably lower than the historically reported figures for the conventional Charnley acetabular cup which G. ELIADES, G. HARTOFILAKIDIS 4,5,7,20-25 range from 0.07 to 1.15 mm per annum. Another important aspect is the effect of cup thickness on the surrounding mantle of acrylic cement (PMMA). 26 Oh showed that the strain in the cement mantle rose in model sockets when the thickness fell from 5 to 2 mm and 27 Pedersen et al reported an increase of 400% in tension and 200% in compression stresses in the cement mantle when the UHMWPE thickness was reduced from 14.5 to 3.5 mm as the simulated head diameter changed from 22 to 44 mm. The fact that our group of patients is relatively young, active and that their common pathology requires a technically demanding operation makes these findings more significant. Crystalline calcium-phosphorus formations observed in the analysed retrieved sockets may be related to the deposition of bone debris or to some interaction with biological fluids on the unloaded lower region of the sockets. While their origin is still under investigation, their limited area is believed to be indicative of an enhanced articular conformity. Our follow-up is relatively short and therefore we are unable to guarantee the long-term advantage of the offset cup, but so far we have had no evidence of deterioration in performance in cups that have been reviewed at 15 years. The use of small cups is increasing not only in neglected cases of congenital hip disease but also in revision cases with problems of bone loss. The offset-bore socket should be considered as an excellent alternative. No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article. References 1. Charnley J. Low friction arthroplasty of the hip: theory and practice. Berlin, etc: Springer-Verlag, 1979:20-5. 2. Hartofilakidis G, Stamos K, Ioannidis TT. Low friction arthroplasty for old untreated congenital dislocation of the hip. J Bone Joint Surg [Br] 1988;70-B:182-6. 3. Hartofilakidis G, Stamos K, Karachalios T, Ioannidis TT, Zacharakis N. Congenital hip disease in adults: classification of acetabular deficiencies and operative treatment with acetabuloplasty combined with total hip arthroplasty. J Bone Joint Surg [Am] 1996;78-A: 683-92. 4. Charnley J, Halley DK. Rate of wear in total hip replacement. Clin Orthop 1975;112:170-9. 5. Wroblewski BM. Direction and rate of socket wear in Charnley lowfriction arthroplasty. J Bone Joint Surg [Br] 1985;67-B:757-61. 6. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop 1976;121:20-32. 7. McCoy TH, Salvati EA, Ranawat CS, Wilson PD Jr. A fifteen-year follow-up study of one hundred Charnley low-friction arthroplasties. Orthop Clin North Am 1988;19:467-76. 8. Rostoker W, Chao EYS, Galante JO. The appearances of wear on polyethylene: a comparison of in vivo and in vitro wear surfaces. J Biomed Mat Res 1978;12:317-35. 9. McKellop HA, Campbell P, Park SH, et al. The origin of submicron polyethylene wear debris in total hip arthroplasty. Clin Orthop 1995; 311:3-20. 10. Bartel DL, Bicknell VL, Wright TM. The effect of conformity, thickness and material on stresses in ultra-high molecular weight components for total joint replacement. J Bone Joint Surg [Am] 1986; 68-A:1041-51. 11. Collier JP, Mayor MB, Surprenant VA, et al. The biomechanical problems of polyethylene as a bearing surface. Clin Orthop 1990; 261:107-13. 12. Harris WH. The problem of osteolysis. Clin Orthop 1995;311: 46-53. 13. Berry DJ, Barnes CL, Scott RD, Cabanela ME, Poss R. Catastrophic failure of the polyethylene liner of uncemented acetabular components. J Bone Joint Surg [Br] 1994;76-B:575-8. 14. Dennis DA, Halley DK. Use of the Charnley mini-offset bore acetabular component in severe acetabular dysplasia: a preliminary report. Clin Orthop 1996;211:140-7. 15. Izquierdo-Avino RJ, Siney PD, Wroblewski BM. Polyethylene wear in the Charnley offset bore acetabular cup: a radiological analysis. J Bone Joint Surg [Br] 1996;78-B:82-4. 16. Saikko VO. Wear of the polyethylene acetabular cup: the effect of head material, head diameter, and cup thickness studied with a hip simulator. Acta Orthop Scand 1995;66:501-6. 17. Wright TM, Bartel DL. The problem of surface damage in polyethylene total knee components. Clin Orthop 1986;205:67-74. 18. Collier JP, Mayor MB, McNamara JL, Suprenant VA, Jensen RE. Analysis of the failure of 122 polyethylene inserts from uncemented tibial knee components. Clin Orthop 1991;273:232-42. THE JOURNAL OF BONE AND JOINT SURGERY LONG-TERM BEHAVIOUR OF THE CHARNLEY OFFSET-BORE ACETABULAR CUP 19. Wright TM, Rimnac CM, Stulberg SD, et al. Wear of polyethylene in total joint replacement: observations from retrieved PCA knee implants. Clin Orthop 1992;276:126-34. 20. Griffith MJ, Seidenstein MK, Williams D, Charnley J. Socket wear in Charnley low friction arthroplasty of the hip. Clin Orthop 1978; 137:37-47. 21. Cupic Z. Long-term follow-up of Charnley arthroplasty of the hip. Clin Orthop 1979;141:28-43. 22. Salvati EA, Wilson PD, Jolley MN, et al. A ten-year follow-up study of our first one hundred consecutive Charnley total hip replacements. J Bone Joint Surg [Am] 1981;63-A:753-66. 23. Wroblewski BM. 15-21-year results of the Charnley low-friction arthroplasty. Clin Orthop 1986;211:30-5. VOL. 80-B, NO. 1, JANUARY 1998 53 24. Wroblewski BM, McCullagh PJ, Siney PD. Quality of the surface finish of the head of the femoral component and the wear rate of the socket in long-term results of the Charnley low-friction arthroplasty. Proc Inst Mech Eng H 1992;206:181-3. 25. Isaac GH, Wroblewski BM, Atkinson JR, Dowson D. A tribological study of retrieved hip prostheses. Clin Orthop 1992;276:115-25. 26. Oh I. A comprehensive analysis of the factors affecting acetabular cup fixation and design in total hip replacement arthroplasty: a series of experimental and clinical studies. In: Hungerford DS, ed. The Hip. Proceedings of the Open Scientific Meeting of the Hip Society, St Louis, etc: CV Mosby 1983:129-77. 27. Pedersen DR, Crowninshield RD, Brand RA, Johnston RC. An axisymmetric model of acetabular components in total hip arthroplasty. J Biomech 1982;15:305-15.