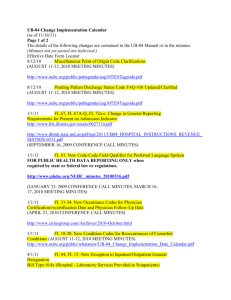
UB-04 LOCATORS NUMERICAL ORDER Form Locators Page
advertisement

UB-04 LOCATORS NUMERICAL ORDER Page Form Locators FL 01 - Billing Provider Name, Address and Telephone Number FL 02 - Billing Provider’s Designated Pay-to Address FL 03a - Patient Control Number FL 03b - Medical/Health Record Number FL 04 - Type of Bill FL 05 - Federal Tax Number FL 06 - Statement Covers Period (From - Through) FL 07 - Reserved for Assignment by the NUBC FL 08 - Patient Name/Identifier FL 09 - Patient Address FL 10 - Patient Birth Date FL 11 - Patient Sex FL 12 - Admission/Start of Care Date FL 13 - Admission Hour FL 14 - Priority (Type) of Admission or Visit FL 15 - Point of Origin for Admission or Visit FL 16 - Discharge Hour FL 17 - Patient Discharge Status FL 18-28 - Condition Codes FL 29 - Accident State FL 30 - Reserved for Assignment by the NUBC FL 31-34 - Occurrence Codes and Dates FL 35-36 - Occurrence Span Codes and Dates FL 37 - Reserved for Assignment by the NUBC FL 38 - Responsible Party Name and Address (Claim Addressee) FL 39-41 - Value Codes and Amounts FL 42 - Revenue Codes FL 43 - Revenue Description/IDE Number/Medicaid Drug Rebate FL 44 - HCPCS/Accommodation Rates/HIPPS Rate Codes FL 45 - Service Date FL 46 - Service Units FL 47 - Total Charges FL 48 - Non-covered Charges FL 49 - Reserved for Assignment by the NUBC FL 50 - Payer Name FL 51 - Health Plan Identification Number FL 52 - Release of Information Certification Indicator FL 53 - Assignment of Benefits Certification Indicator FL 54 - Prior Payments - Payer FL 55 - Estimated Amount Due - Payer FL 56 - National Provider Identifier - Billing Provider FL 57 - Other (Billing) Provider Identifier FL 58 - Insured’s Name FL 59 - Patient’s Relationship to Insured FL 60 - Insured’s Unique Identifier FL 61 - Insured’s Group Name FL 62 - Insured’s Group Number FL 63 - Treatment Authorization Code FL 64 - Document Control Number (DCN) FL 65 - Employer Name (of the Insured) FL 66 - Diagnosis and Procedure Code Qualifier (ICD Version Indicator) FL 67 - Principal Diagnosis Code and Present on Admission Indicator BCNEPA/FPH/FPLIC Billing Manual November 2012 3 3 4 4 5 8 9 10 10 11 11 11 12 12 13 13 16 16 18 22 22 22 26 27 27 28 36 65 66 67 68 69 69 70 70 70 71 71 72 72 73 73 74 75 75 76 76 77 77 78 78 79 Page 1 Form Locators Page FL 67A-Q - Other Diagnosis Code and Present on Admission Indicator FL 68 - Reserved for Assignment by the NUBC FL 69 - Admitting Diagnosis Code FL 70a-c - Patient’s Reason for Visit FL 71 - Prospective Payment System (PPS/DRG) Code FL 72a-c - External Cause of Injury (ECI) Code and POA Indicator FL 73 - Reserved for Assignment by the NUBC FL 74 - Principal Procedure Code and Date FL 74a-e - Other Procedure Codes and Dates FL 75 - Reserved for Assignment by the NUBC FL 76 - Attending Provider Name and Identifiers FL 77 - Operating Physician Name and Identifiers FL 78-79 - Other Provider name and Identifiers FL 80 - Remarks Field FL 81 - Code-Code Field BCNEPA/FPH/FPLIC Billing Manual November 2012 83 83 84 85 86 87 87 88 88 89 89 91 92 94 95 Page 2 Form Locator 01 Data Element Billing Provider Name, Address and Telephone Number Definition: The name and service location of the provider submitting the bill. Required Yes Reporting Name and Address, Telephone, Country Code Required Telephone UB-04: Required 004010/004010A1: Situational. Required when this information is different than that contained in the Submitter PER segment (Loop ID-1000A). 005010: Situational. Required when this information is different than that contained in the Submitter PER segment (Loop ID-1000A). County Code UB-04: Situational. Required when the address is outside the United States of America. 004010/004010A1: Situational. Required when the address is outside of the U.S. 005010: Situational. Required when the address is outside of the U.S. Field Attributes 1 Field 4 Lines Notes The Billing Address must be a street address. Post Office Box or Lock Box addresses are to be sent in the Pay-To-Address field of Form locator 02, if necessary. Form Locator 01 uses the full nine-digit ZIP. 25 Positions Alphanumeric Left-justified Enter the information provided on the appropriate line: Line 1 Provider Name Line 2 Street Address Line 3 City (Positions 1-12 Left-justified), State (Positions 14-15), and Zip Code (Positions 17-25) Line 4 Telephone (Positions 1-10); Fax (Positions 13-22); Country Code (Positions 24-25); Use the alpha-2 country codes from Part 1 of ISO 3166) Form Locator 02 Data Element Billing Provider’s Designated Pay-to Address Definition: The address that the provider submitting the bill intends payment to be sent if different than FL 01. Required If Applicable Reporting UB-04: Situational. Required when the address for payment is different than that of the Billing Provider in Form Locator 01. 00410/004010A1: Situational. Required if the Pay-to Provider is a different entity than the Billing Provider. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 3 Form Locator 02 005010: Situational. Required when the address for payment is different than that of the Billing Provider. (Note: The purpose of Loop ID-2010AB has changed from previous versions. Loop ID-2010AB only contains address information when different from the Billing Provider Address. There are no applicable identifiers for Pay-To Address information.) Field Attributes 1 Field 4 Lines Notes Enter the information provided on the appropriate line: 25 Positions Alphanumeric Left-justified Line 1 Pay-to Name Line 2 Street Address or Post Office Box Line 3 City (Positions 1-16, Left-justified), State (Positions 18-19), and Zip Code (Positions 21-25) Line 4 NOT USED. Reserved for Assignment by the NUBC. Address may include post office box or street name and number, city, state and ZIP Code. Form Locator 02 uses a 5-digit ZIP Code. Form Locator 03a Data Element Patient Control Number Definition: Patient’s unique (alphanumeric) number assigned by the provider to facilitate retrieval of the individual’s account of services (accounts receivable) containing the financial billing records and any postings of payment. Required Yes Reporting UB-04; 004010/004010A1; 00510 Required Field Attributes 1 Field 1 Line Notes To enable providers to reconcile payments against the account receivable for the patient, it is a requirement that payers include the patient control number on the payment check, remittance advice or voucher. 24 Positions Alphanumeric Left-justified Form Locator 03b Data Element Medical/Health Record Number Definition: The number assigned to the patient’s medical/health record by the provider. Required No BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 4 Form Locator 03b Reporting UB-04: Situational. Required when the provider needs to identify for future inquiries, the actual medical record of the patient. 004010/004010A1, 005010: Situational. Required when the provider needs to identify for future inquiries, the actual medical record of the patient identified in either Loop ID2010BA or Loop ID-2010CA for this episode of care. Field Attributes 1 Field 1 Line 24 Positions Notes The medical/health record number references a file that contains the history of treatment. It should not be substituted for the Patient Control Number (FL 03a), which is assigned by the provider to facilitate retrieval of the individual financial record, which is typically associated with an episode of care. Alphanumeric Left-justified Form Locator 04 Data Element Type of Bill Definition: A code indicating the specific type of bill (e.g., hospital inpatient, outpatient, replacements, voids, etc.). The first digit is a leading zero (Do not include the leading zero on electronic claims). The fourth digit defines the frequency of the bill for the institutional and electronic professional claim. Required Yes Reporting Required Field Attributes 1 Field (2 Components) 1 Line 4 Positions Alphanumeric Left-justified (all positions fully coded) Notes The “x” in the following tables (first component) represents a placeholder for the frequency code (second component). Inpatient and Outpatient Designation The matrix which follows contains general guidelines on what constitutes an “inpatient” or “outpatient” claim according to the first three digits of Type of Bill (TOB). Inpatient Part B Only – Type of Bill 012x and 022x The general designations for TOBs 012x and 022x are “OP”. Medicare will pay, under Part B for physician services and for non-physician medical and other health services when furnished by a participating hospital or SNF to an inpatient of the facility when patients are not eligible or entitled to Part A benefits or the patient has exhausted their Part A benefits. This is done when the patients are not eligible or entitles to, or have exhausted, their Part A benefits. Such services are billed on these two bill types. Inpatient/Outpatient General Designation/ Exception # on FL04 Type of Bill 000x-010x 011x 012x 013x 014x 015x-017x 018x Reserved for Assignment by NUBC Hospital Inpatient (Including Medicare Part A) Hospital Inpatient (Medicare Part B only) Hospital Outpatient Hospital - Laboratory Services Provided to Non-patients Reserved for Assignment by NUBC Hospital - Swing Beds BCNEPA/FPH/FPLIC Billing Manual November 2012 IP OP/1, 3 OP OP/6 IP Page 5 Form Locator 04 Inpatient/Outpatient General Designation/ Exception # on FL04 Type of Bill 019x-020x 021x 022x 023x 024x-027x 028x 029x-031x 032x 033x 034x 035x-040x 041x 042x 043x 044x-064x 065x 066x 067x-070x 071x 072x 073x 074x 075x 076x 077x 078x 079x 080x 081x 082x 083x 084x 085x 086x 087x-088x 089x 090x-999x Reserved for Assignment by NUBC Skilled Nursing - Inpatient (Including Medicare Part A) Skilled Nursing - Inpatient (Medicare Part B) Skilled Nursing - Outpatient Reserved for Assignment by NUBC Skilled Nursing - Swing Beds Reserved for Assignment by NUBC Home Health - Inpatient (plan of treatment under Part B only) Home Health - Outpatient (plan of treatment under Part A, Including DME under Part A Home Health - Other (for medical and surgical services not Under a plan of treatment) Reserved for Assignment by NUBC Religious Non-Medical Health Care Institutions - Hospital Inpatient Reserved for Assignment by NUBC Religious Non-Medical Health Care Institutions - Outpatient Services Reserved for Assignment by NUBC Intermediate Care - Level I Intermediate Care - Level II Reserved for Assignment by NUBC Clinic - Rural Health Clinic - Hospital Based or Independent Renal Dialysis Center Clinic - Freestanding Clinic - Outpatient Rehabilitation Facility (ORF) Clinic - Comprehensive Outpatient Rehabilitation Facility (CORF) Clinic - Community Mental Health Center Clinic - Federally Qualified Health Center (FQHC) (Effective 4/1/10) Licensed Freestanding Emergency Medical Facility (Effective 7/1/12) Clinic - Other Reserved for Assignment by NUBC Hospice (non-hospital based) Hospice (hospital based) Ambulatory Surgery Center Free Standing Birthing Center Critical Access Hospital Residential Facility Reserved for Assignment by NUBC Special Facility - Other Reserved for Assignment by NUBC IP/2, 4 OP/1, 3 OP IP/3 OP/1 OP/1 OP/1 IP OP IP/3 IP/3 OP OP OP OP OP OP OP OP OP OP/1 OP/1 OP OP OP IP/3 IP or OP* - *Effective 7/1/13, the general designation is OP only. Exceptions to Inpatient/Outpatient general Designation by Data Element/Form Locator: Exc. # 1 Data Element FL12 - Admission/Start of Care Date Usage Note in 005010 837: Required on inpatient claims. BCNEPA/FPH/FPLIC Billing Manual November 2012 Usage Requirement by Type of Bill Required on all inpatient claims (IP) and 012x, 022x, 032x, 033x, 034x, 081x and 082x. Page 6 Form Locator 04 Exceptions to Inpatient/Outpatient general Designation by Data Element/Form Locator: Data Element FL13 - Admission Hour Usage Note in 00510 837: Selection of the appropriate qualifier Is designated by the NUBC Billing Manual. Usage Requirement by Type of Bill Required on all inpatient claims (IP) except for 021x. 3 FL69 - Admitting Diagnosis: Usage Note in 00510 837: Required when claim involves an inpatient admission. Required on 012x, 022x and inpatient claims (IP) except 028x, 065x, 066x, 086x. 4 FL16 - Discharge Hour: Usage Note in 00510 837: Required on all final inpatient claims. Required on inpatient claims (IP) with a Frequency Code of 1, 4 or 7, except for 021x. 5 FL70a-c - Patient’s Reason for Visit: Usage Note in 00510 837: Required when claim involves outpatient visits. Not required on any claim except for 013x, 085x and 078x when: Exc. # 2 a) Priority (Type) of Admission/Visit Codes 1,2, or 5 are reported AND b) Revenue Codes 045x, 0516, 0526, or 0762 are reported. May be reported on all other 013x, 078x and 085x types of bills at submitter’s discretion when this information provides additional information to support medical necessity. See FL70 a-c for more information. 6 FL15 – Point of Origin for Admission or Visit Required on all claims except 014x. Usage Note in 00510 837: Required for all inpatient and outpatient services. Type of Bill Frequency Codes: 0 1 2 3 4 5 6 7 8 9 A B C Non-Payment/Zero Admit Through Discharge Claim (a) Interim - First Claim Interim - Continuing Claim (b) Interim - Last Claim (b) Late Charge(s) Only Reserved for assignment by the NUBC Replacement of Prior Claim (a) Void/Cancel of Prior Claim (a) Final Claim for a Home Health PPS Episode Admission/Election Notice Hospice/CMS Coordinated Care Demonstration/Religious Non-Medical Health Care Institution/Centers of Excellence Demonstration/Provider Partnerships Demonstration Hospice Change of Provider Notice BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 7 Form Locator 04 Type of Bill Frequency Codes: D E F G H I J K L M N O P Q R-W X Y Z Hospice/CMS Coordinated Care Demonstration/Religious Non-Medical Health Care Institution/Centers of Excellence Demonstration/Provider Partnerships Demonstration Void/Cancel Hospice Change of Ownership Beneficiary Initiated Adjustment Claim CWF Initiated Adjustment Claim CMS Initiated Adjustment Intermediary Adjustment Claim (Other than QIO or Provider) Initiated Adjustment Claim - Other OIG Initiated Adjustment Claim Reserved for assignment by the NUBC MSP Initiated Adjustment Claim Reserved for assignment by the NUBC Nonpayment/Zero Claims QIO Adjustment Claim Claim Submitted for Reconsideration Outside of Timely Limits Reserved for assignment by the NUBC Void/Cancel a Prior Abbreviated Encounter Submission Replacement of Prior Abbreviated Encounter Submission New Abbreviated Encounter Submission Footnotes for Frequency Codes (a) The developers of the Professional and Dental Health Care Claim Implementation Guides have indicated that this code is acceptable for use in those transactions. (b) Do not use for Medicare inpatient hospital PPS claims. (For second and subsequent interim bills use code 7, and see Condition Code D3 (FL18-FL28). Form Locator 05 Data Element Federal Tax Number Definition: The number assigned to the provider by the federal government for tax reporting purposes. Also known as a tax identification number (TIN) or employer identification number (EIN). To identify affiliated subsidiaries using federal tax “sub-ID” (see note below). Required Yes Reporting Required Field Attributes 1 Field Upper Line, 4 positions (sub-ID - optional) Alphanumeric Left-justified Lower Line, 10 positions (include hyphen) Alphanumeric Left-justified Notes Upper line is the federal tax sub-ID number as assigned by the provider. To be used by providers that assign a unique identifying number for their affiliated subsidiaries, e.g., hospital psychiatric pavilion. Lower line is the federal tax number entered as: NN-NNNNNNN. For electronic claims, do not use the hyphen when reporting federal tax ID. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 8 Form Locator 06 Data Element Statement Covers Period (From-Through) Definition: The beginning and ending service dates of the period included on this bill. Required Yes Reporting Required: UB-04, 004010/004010A1, 005010 Field Attributes 2 Field 1 Line 6 Positions (two six-digit dates) Numeric Right-justified (all positions fully coded) Notes 1. For all services received on a single day, use the same date for “From” and “Through”. 2. Enter both dates as month, day, and year (MMDDYY). Example: 010112 3. The “From” date should not be confused with the Admission Date (FL12). The Statement Covers Period From date in Form Locator 6 (“From” Date) is distinctly different than the Admission Date in Form Locator 12. The dates may coincide in some circumstances, but should not be confused. It is also not a requirement that the Admission Date Fall in between the “From” Date and the Statement Covers Period “Through” date. Any edit that requires that the two dates match is invalid. In addition, an edit that compares the number of days in the Statement Covers Period to any other data element (e.g., total accommodation days reported in the revenue code section) is inherently flawed. The Admission Date is purely the date the patient was admitted as an inpatient to the facility (or indicates the start of care date for home health and hospice). It is reported on all inpatient claims regardless of whether it is an initial, interim, or final bill. The Statement Covers Period indentifies the span of service dates included in a particular bill. The “From” Date is the earliest date of service on the bill. Summary The billing process for providers is easier if the correct distinctions and validation edits are properly applied. Some edits are forcing the Admission Date, Procedure Date and “From” date to be identical. Maintaining the distinction alleviates any special routines that providers must now undertake in order to circumvent a flawed edit. The same issues and methodology apply to the 837 institutional claim, which has distinct data segments and qualifiers to properly distinguish Admission Date and Statement Covers Period dates. 2012 Update The Admission Date and Statement Covers Period on claims are two distinctly different data elements: The Admission Date (Form Locator 12) is purely the date the patient was admitted as an inpatient to the facility ( or indicates the start of care date for home health and hospice). It is reported on all inpatient claims regardless of whether it is an initial, interim, or final bill. The Statement Covers period (“From” and “Through” dates in FL 6) identifies the span of service dates included in a particular bill. The From Date is the earliest date of service on the bill. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 9 Form Locator 07 Data Element Reserved for Assignment by the NUBC. Definition: Required Reporting Not Used Field Attributes 1 Field 2 Lines 7 Positions (upper line) 8 Positions (lower line) Form Locator 08 Data Element Patient Name/Identifier Definition: Last name, first name and middle initial of the patient and the patient identifier as assigned by the payer. Required Yes Reporting Patient Name UB-04: Required 004010/004010A1: Required If the patient is the subscriber, the name is reported in Loop ID 2010BA. If the patient is not the subscriber, the name is reported in Loop ID 2010CA. 005010: Required If the patient is the subscriber, the name is reported in Loop ID 2010BA. If the patient is not the subscriber but has a unique identifier assigned by the destination payer, the name is reported in Loop ID 2010BA. If the patient is not the subscriber and cannot be identified by a unique identifier assigned by the destination payer, the name is reported in Loop ID 2010CA. Reporting Patient ID UB-04: Report if number is different from the subscriber/insured’s ID (FL 60). 004010/004010A1: Required If the patient is the subscriber, the identifier is reported in Loop ID 2010BA. If the patient is not the subscriber, the identifier is reported in Loop ID 2010CA. 005010: Required when the patient name has been mapped to Loop ID 2010BA. Not Used when the patient name has been mapped to Loop ID 2010CA. Field Attributes 1 Field 2 Lines 2 Subfields Alphanumeric Left-justified Subfield a: Patient Identifier (19positions) Subfield b: Patient Name (29 positions) Notes On the paper UB-04 form, use a comma or space to separate last and first names. No space should be left between a prefix and a name as in MacBeth and McEnroe. Titles (such as Sir, Msgr, Dr.) should not be recorded in this data element. Record hyphenated names with the hyphen as in Smith-Jones, Rebecca. To record suffix of a name, write the last name, leave a space and write the suffix, then write the first name as in Snyder Iii, Harold, or Addams Jr., Glen. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 10 Form Locator 09 Data Element Patient Address Definition: The mailing address of the patient. Enter the complete mailing address including street number and name or post office box number or RFD; city name; state name; ZIP code. Required Yes Reporting UB-04 Required 004010/004010A1, 005010: Required. Reported in the same Loop ID (2010BA or 2010CA) that the Patient Name has been mapped to. Field Attributes 1 Field 2 Lines 5 Subfields Subfield a: Street Address (40 Positions) Subfield b: City (30 Positions) Subfield c: State (2 Positions) Subfield d: ZIP Code (9 Positions) Subfield e: Country Code (2 Positions) Alphanumeric Left-justified Notes Form Locator 10 Data Element Patient Birth Date Definition: The date of birth of the patient. Required Yes Reporting UB-04 Required 004010/004010A1, 005010: Required. Reported in the same Loop ID (2010BA or 2010CA) that the Patient Name has been mapped to. Field Attributes 1 Field 1 Line 8 Positions Notes For paper claims only, if full birth date is unknown, indicate zeros for all eight digits. Enter: “MMDDYYY” Numeric Right-justified (all positions fully coded) Form Locator 11 Data Element Patient Sex Definition: The sex of the patient as recorded at admission, outpatient service, or start of care. Required Yes Reporting UB-04 Required 004010/004010A1, 005010: Required. Reported in the same Loop ID (2010BA or 2010CA) that the Patient Name has been mapped to. Field Attributes 1 Field Left-justified 1 Line 1 Position Alphanumeric Form Locator 11 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 11 Notes M = Male F = Female U = Unkown Form Locator 12 Data Element Admission/Start of Care Date Definition: The start date for this episode of care. For inpatient services, this is the date of admission. For other (home health) services, it is the date the episode of care began. Required Yes Reporting UB-04: Required on all inpatient claims (“IP”), 012x, 022x, 032x, 033x, 034x, 081x,and 082x. 004010/004010A1: Required 00510: Required on inpatient claims, home health claims and hospice claims. Field Attributes 1 Field 1 Line 6 Positions Right-justified (all positions fully coded) Notes Enter the admission date as month, day and year (MMDDYY). The Admission/Start of Care Date is a discrete data element and should not be confused with the Statement Covers Period “From” date on Form Locator 06. Numeric Form Locator 13 Data Element Admission Hour Definition: The code referring to the hour during which the patient was admitted for inpatient care. Required Yes (Inpatient only) Reporting UB-04: Required on all inpatient claims except for Type of Bill 021x. 004010/004010A1: This segment is required on all inpatient claims. 005010: Selection of the appropriate qualifier is designated by the NUBC Billing Manual. (Therefore, required on inpatient claims except for Type of Bill 021x as noted above.) Field Attributes 1 Field Alphanumeric Notes Code Structure Code Time - A.M. 00 12:00 - 12:59 Midnight 01 01:00 - 01:59 02 02:00 - 02:59 03 03:00 - 03:59 04 04:00 - 04:59 05 05:00 - 05:49 06 06:00 - 06:59 07 07:00 - 07:59 08 08:00 - 08:59 09 09:00 - 09:59 10 10:00 - 10:59 11 11:00 - 11:59 1 Line 2 Positions Left-justified (all positions fully coded, unless blank) Code 12 13 14 15 16 17 18 19 20 21 22 23 Time - P.M. 12:00 - 12:59 Noon 01:00 - 01:59 02:00 - 02:59 03:00 - 03:59 04:00 - 04:59 05:00 - 05:59 06:00 - 06:59 07:00 - 07:59 08:00 - 08:59 09:00 - 09:59 10:00 - 10:59 11:00 - 11:59 Form Locator 14 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 12 Data Element Priority (Type) of Admission or Visit Definition: A code indicating the priority of this admission/visit. Required Yes Reporting UB-04: Required on inpatient and outpatient services. 004010/004010A1: Required when patient is being admitted to the hospital for inpatient services. 005010: Required on inpatient and outpatient services. Field Attributes 1 Field Alphanumeric Notes See codes below Code Definition 1 Line Left-justified 1 Position 1 Emergency The patient requires immediate medical intervention as a result of severe, life threatening or potentially disabling conditions. 2 Urgent The patient requires immediate attention for the care and treatment of a physical or mental disorder. 3 Elective The patient’s condition permits adequate time to schedule the services. 4 Newborn Use of this code necessitates the use of special Source of Admission Codes (Form Locator 15). 5 Trauma Visit to trauma center/hospital as licensed or designated by the state or local government authority authorized to do so, or as verified by the American College of Surgeons and involving a trauma activation. (Use Revenue Code 068x to capture trauma activation charges.) 6-8 9 Reserved for assignment by NUBC Information not Available Information not available. Form Locator 15 Data Element Point of Origin for Admission or Visit Definition: A code indicating the point of patient origin for this admission or visit. Required Yes (Inpatient, SNF, Home Health and Hospice) If Applicable (Outpatient) Reporting UB04: Required on all bill types except 014x. 004010/004010A1: Required for all inpatient admissions. Required on Medicare outpatient registrations for diagnostic testing services. 005010: Required for all inpatient and outpatient services. (Therefore required on all bill types marked “IP” and “OP” per FL 04 except for bill type 014x, which is equivalent to the UB-or requirement.) Form Locator 15 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 13 Field Attributes 1 Field Alphanumeric 1 Line Left-justified 1 Position Notes The updated and revised code list has been designed to focus on patients’ place or point of origin rather than the source of a physician order or referral. A physician order or referral is implicit in any admission or visit. By modifying the definitions of the codes in this manner, the ambiguity in the code structure has been eliminated; all of the codes become mutually exclusive. The point of origin is the direct source for the particular facility. I. Transfers - From an Another Facility While at another acute care hospital/facility, the patient is seen by the emergency room physicians. The patient is then transferred to our facility. The patient arrives at our facility through the emergency room. Point of Origin Code 4 - Transfer from a Hospital (Different Facility) II. Transfers - Skilled Nursing Facility A resident from a skilled nursing facility is taken to an acute care hospital for medical care. Point of Origin Code 5 - Transfer from a Skilled Nursing Facility III. Transfer by Law Enforcement or Court A patient arrives at the health care facility accompanied by policy. Point of Origin Code 8 - Court/Law Enforcement Description Code 1 2 3 4 5 6 7 Inpatient: The patient was admitted to this facility. Outpatient: The patient presented to this facility for outpatient services. Examples: Includes patients coming from home, or workplace and patients receiving care at home (such as home health services). Clinic or Physician’s Inpatient: The patient was admitted to this facility. Office Outpatient: The patient presented to this facility for outpatient services. Reserved for assignment by the NUBC (Discontinued effective 10/1/07) Transfer from a Hospital Inpatient: The patient was admitted to this facility as a hospital transfer (Different Facility) from an acute care facility where he or she was an inpatient or outpatient. Outpatient: The patient was transferred to this facility as an outpatient from an acute care facility. Usage Note: Excludes Transfers from Hospital Inpatient in the Same Facility (See Code D). Transfer from a Skilled Inpatient: The patient was admitted to this facility as a transfer from a Nursing Facility (SNF) SNF, ICF or ALF where he or she was a resident. Intermediate Care Outpatient: The patient was referred to this facility for outpatient or referenced Facility (ICF) or Assisted diagnostic services from a SNF, ICF or ALF where he or she was Living Facility (ALF) a resident. Transfer from Another Inpatient: The patient was admitted to this facility as a transfer from Health Care Facility another type of health care facility not defined elsewhere in this code list. Outpatient: The patient presented to this facility for services from another health care facility not defined elsewhere in this code list. Reserved for assignment by the NUBC. (Discontinued effective 7/1/10) Non-Health Care Facility Point of Origin BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 14 Form Locator 15 Code 8 Description Court/Law Enforcement Inpatient: Outpatient: 9 Information Not Available Inpatient: Outpatient: A B C D Transfer From Another Home Health Agency Transfer from One Distinct Inpatient: Unit of the Hospital to another Distinct Unit of the Same Hospital Resulting in a Outpatient: Separate Claim to the Payer E Transfer from Ambulatory Inpatient: Surgery Center Outpatient: F Transfer from a Hospice Facility Inpatient: Outpatient: G-Z The patient was admitted to this facility upon the direction of a court of law, or upon the request of a law enforcement agency representative. The patient was referred to this facility upon the direction of a court of law, or upon the request of a law enforcement agency representative for outpatient or referenced diagnostic services. The patient’s Point of Origin is not know. The patient’s Point of Origin is not know. Reserved for assignment by the NUBC (Discontinued effective 10/1/07) Discontinued Effective 7/1/10. (Replaced with Condition Code 47 FL 18-28) Discontinued Effective 7/1/10 The patient was admitted to this facility as a transfer from hospital inpatient within this hospital resulting in a separate claim to the payer. The patient received outpatient services in this facility as a transfer from within this hospital resulting in a separate claim to the payer. Usage Note: For purposes of this code, “Distinct Unit” is defined as a unique unit or level of care at the hospital requiring the issuance of a separate claim to the payer. Examples could include observation services, psychiatric units, rehabilitation units, a unit in a critical access hospital, or a swing bed located in an acute hospital. The patient was admitted to this facility as a transfer from an ambulatory surgery center. The patient presented to this facility for outpatient or referenced diagnostic services from an ambulatory surgery center. The patient was admitted to this facility as a transfer from a hospice facility. The patient presented to this facility for outpatient or referenced diagnostic services from a hospice facility. Reserved for assignment by the NUBC Code Structure for Newborn 1-4 5 6 7-9 Born Inside this Hospital Born Outside of this Hospital BCNEPA/FPH/FPLIC Billing Manual November 2012 Reserved for assignment by the NUBC. (Discontinued Effective 10/1/07) A baby born inside this Hospital. A baby born outside of this Hospital. Reserved for assignment by the NUBC. Page 15 Form Locator 16 Data Element Discharge Hour Definition: Code indicating the discharge hour of the patient from inpatient care. Required Yes (Inpatient, SNF, Home Health and Hospice) If Applicable (Outpatient) Reporting UB-04: Required on inpatient claims (“IP”) with a Frequency Code of 1 or 4, except for Type of Bill 021x. 004010/004010A1, 005010: Required on all final inpatient claims. Field Attributes 1 Field Alphanumeric Notes Code Structure Code 00 01 02 03 04 05 06 07 08 09 10 11 1 Line 2 Positions Left-justified (all positions fully coded, unless blank) Time - A.M. 12:00 - 12:59 Midnight 01:00 - 01:59 02:00 - 02:59 03:00 - 03:59 04:00 - 04:59 05:00 - 05:49 06:00 - 06:59 07:00 - 07:59 08:00 - 08:59 09:00 - 09:59 10:00 - 10:59 11:00 - 11:59 Code 12 13 14 15 16 17 18 19 20 21 22 23 Time - P.M. 12:00 - 12:59 Noon 01:00 - 01:59 02:00 - 02:59 03:00 - 03:59 04:00 - 04:59 05:00 - 05:59 06:00 - 06:59 07:00 - 07:59 08:00 - 08:59 09:00 - 09:59 10:00 - 10:59 11:00 - 11:59 Form Locator 17 Data Element Patient Discharge Status Definition: A code indicating the disposition or discharge status of the patient at the end service for the period covered on this bill, as reported in FL6, Statement Covers Period. Required Yes (Inpatient, SNF, Home Health and Hospice) Not Required (Outpatient) Reporting Required for inpatient claims/encounters. Field Attributes 1 Field Numeric Notes The patient’s discharge status is required on all institutional claims. Identifying the appropriate code may often be confusing; judgment must be used in all cases. A basic rule of thumb is to code to the highest level of care that is known - -for example, an individual discharged to home with a home health plan of care is coded as 06, rather than 01. BCNEPA/FPH/FPLIC Billing Manual November 2012 1 Line Right-justified 2 Positions Page 16 Form Locator 17 Code Structure 01 02 03 04 05 06 07 08 09 10-19 20 21 22-29 30 31-39 40 41 42 43 44-49 50 51 52-60 Discharged to Home or Self Care (Routine Discharge) Usage Note: Includes discharge to home; home on oxygen if DME only; any other DME only; group home, foster care, independent living and other residential care arrangements; outpatient programs; such as partial hospitalization or outpatient chemical dependency programs. Discharged/transferred to a Short-Term General Hospital for Inpatient Care Discharged/transferred to Skilled Nursing Facility (SNF) with Medicare Certification in Anticipation of Skilled Care Usage Note: Medicare - Indicates that the patient is discharged/transferred to a Medicare certified nursing facility. For hospitals with an approved swing bed arrangement, use Code 61 - Swing Bed. For reporting other discharges/transfers to nursing facilities, see codes 04 and 64. Discharged/transferred to a Facility that Provides Custodial or Supportive Care Usage Note: Includes intermediate care facilities (ICFs) if specifically designated at the state level. Also used to designate patients that are discharged/transferred to a nursing facility with neither Medicare or Medicaid certification and for discharges/transfers to Assisted Living Facilities. Discharged/transferred to a Designated Cancer Center or Children’s Hospital Usage Note: Transfers to non-designated cancer hospitals should use Code 02. A list of (National Cancer Institute) Designated Cancer Centers can be found at http://www3.cancer.gov/cancercenters/centerslist.html. Discharged/transferred to Home Under Care of an Organized Home Health Service Organization in Anticipation of Covered Skilled Care Usage Note: Report this code when the patient is discharged/transferred to home with a written plan of care (tailored to the patient’s medical needs) for home care services. Not used for home health services provided by a DME supplier or from a Home IV provider for home IV services. Left Against Medical Advice or Discontinued Care Reserved for Assignment by the NUBC Admitted as an Inpatient to this Hospital Usage Note: For use only on Medicare outpatient claims. Applies only to those Medicare outpatient services that begin greater than three days prior to an admission. Reserved for Assignment by the NUBC Expired Discharged/transferred to Court/Law Enforcement Reserved for Assignment by the NUBC Still patient Usage Note: Used when patient is still within the same facility; typically used when billing for leave of absence days or interim bills. Reserved for Assignment by the NUBC Expired at Home Expired in a Medical Facility (e.g. hospital, SNF, ICF, or free standing hospice) Expired - Place Unknown Usage Note: For use only on Medicare and TRICARE claims for hospice care. Discharged/transferred to a Federal Health Care Facility Usage Note: Discharges and transfers to a government operated health facility such as a Department of Defense hospital, a Veteran’s Administration hospital or a Veteran’s Administration nursing facility. To be used whenever the destination at discharge is a federal health care facility, whether the patient lives there or not. Reserved for Assignment by the NUBC Hospice - Home Hospice - Medical Facility (Certified) Providing Hospice Level of Care Reserved for Assignment by the NUBC BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 17 Form Locator 17 Code Structure 61 62 63 64 65 66 67-69 70 71-99 Discharged/transferred to Hospital-Based Medicare Approved Swing Bed Usage Note: Medicare - Used for reporting patients discharged/transferred to a SNF level of care within the hospital’s approved swing bed arrangement. Discharged/transferred to an Inpatient Rehabilitation Facility (IRF) including Rehabilitation Distinct Part Units of a Hospital Discharged/transferred to a Medicare Certified Long Term Care Hospital (LTCH) Usage Note: For hospitals that meet the Medicare criteria for LTCH certification. Discharged/transferred to a Nursing Facility Certified under Medicaid but not Certified under Medicare Discharged/transferred to a Psychiatric Hospital or Psychiatric Distinct Part Unit of a Hospital Discharged/transferred to a Critical Access Hospital (CAH) Reserved for Assignment by the NUBC Discharged/transferred to another Type of Health Care Institution not Defined Elsewhere in this Code List (See Code 05) Reserved for Assignment by the NUBC Form Locator 18-28 Data Element Condition Codes Definition: A code(s) used to identify conditions or events relating to this bill that may affect processing. Required If Applicable Reporting UB-04, 004010/004010A1, 005010: Required when there is a Condition Code that applies to this claim. Field Attributes 11 Fields Alphanumeric Notes No specific date is associated with this code. Condition Codes should be entered in alphanumeric sequence. Codes assigned as Payer Codes are for internal use only by the payer: they are assigned by the payer and are not required to be communicated to another payer for COB, unless these Payer Codes are communicated to the other payers as part of their contracted working relationship. If all of the Condition Code fields are filled, use FL 81 Code-Code field with the appropriate qualifier code (A1) to indicate that a Condition Code is being reported. 1 Line 2 Positions All positions fully coded Code Structure 01 02 03 04 05 06 07 08 Military Service Related Condition is Employment Related Patient Covered by Insurance Not Reflected Here Information Only Bill Lien Has Been Filed ESRD Patient in First 30 Months of Entitlement Covered by Employer Group Health Insurance Treatment of Non-terminal Condition for Hospice Patient Beneficiary Would Not Provide Information Concerning Other Insurance Coverage BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 18 Form Locator 18-28 Code Structure 09 10 11 12-16 17 18 19 20 21 22 23 24 25 26 27 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 45 46 47 48 49 50 51 52 53-55 56 57 58 59 60 61 62-65 66 67 68 69 70 Neither Patient nor Spouse is Employed Patient and/or Spouse is Employed but no EGHP Exists Disabled Beneficiary but No LGHP Payer Codes Patient is Homeless Maiden Name Retained Child Retains Mother’s Name Beneficiary Requested Billing Billing for Denial Notice Patient on Multiple Drug Regimen Home Care Giver Available Home IV Patient Also Receiving-HHA Services Patient is Non-U.S. Resident VA Eligible Patient Chooses to Receive Services in a Medicare Certified Facility Patient Referred to a Sole Community Hospital for a Diagnostic Laboratory Test Patient and/or Spouse’s EGHP is Secondary to Medicare Disabled Beneficiary and/or Family Member’s LGHP is Secondary to Medicare Qualifying Clinical Trials Patient is Student (Full Time - Day) Patient is Student (Cooperative/Work Study Program) Patient is Student (Full Time - Night) Patient is Student (Part Time) Reserved for assignment by the NUBC General Care Patient in a Special Unit Ward Accommodation at Patient Request Semi-Private Room Not Available. Note: Required when billing to indicate member not liable for private room difference. Private Room Medically Necessary. Note: Required when billing to indicate member not liable for private room difference. Same Day Transfer Partial Hospitalization Continuing Care not Related to Inpatient Hospitalization Continuing Care not Provided Within Prescribed Post-discharge Window Inpatient Admission Changed to Outpatient Ambiguous Gender Category Non-availability Statement on File Transfer from Another Home Health Agency (Effective 7/1/10) Psychiatric Residential Treatment Centers for Children and Adolescents (RTCs) Product Replacement within Product Lifecycle Product Replacement for Known Recall of a Product Attestation of Unrelated Outpatient Nondiagnostic Services (Effective 4/1/11) Out of Hospice Service Area (Effective 7/1/12) Reserved for assignment by the NUBC Medical Appropriateness SNF Readmission Terminated Medicare Advantage Enrollee Non-primary ESRD Facility Day Outlier Cost Outlier Payer Code Provider does not Wish Cost Outlier Payment Beneficiary Elects not to use Life Time Reserve (LTR) Days Beneficiary Elects to use Life Time Reserve (LTR) Days IME/DGME/N&AH Payment Only Self Administered Anemia Management Drug BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 19 Form Locator 18-28 Code Structure 71 72 73 74 75 76 77 78 79 80 81-99 A0 A1 A2 A3 A4 A5 A6 A7-A8 A9 AA(a) AB(a) AC(a) AD(a) AE(a) AF(a) AG(a) AH(a) AI AJ AK AL AM AN AO-AZ B0 B1 B2 B3 B4 B5-B0 BP BQ-C0 C1 C2 C3 C4 C5 C6 C7 C8-CZ Full Care in Unit Self Care in Unit Self Care Training Home Home - 100 Percent Reimbursement Back-up in Facility Dialysis Provider Accepts or is Obligated/Required due to a Contractual Arrangement or Law to Accept Payment by a Primary Payer as Payment in Full New Coverage not Implemented by Managed Care Plan CORF Services Provided Offsite Home Dialysis - Nursing Facility Reserved for assignment by the NUBC TRICARE External Partnership Program EPSDT/CHAP (Early and Periodic Screening Diagnosis and Treatment) Physically Handicapped Children’s Program Special Federal Funding Family Planning Disability Vaccines/Medicare 100% Payment Reserved for assignment by the NUBC Second Opinion Surgery Abortion Performed due to Rape Abortion Performed due to Incest Abortion Performed due to Serious Fetal Genetic Defect, Deformity, or Abnormality Abortion Performed due to a Life Endangering Physical Condition Abortion Performed due to Physical Health of Mother that is not Life Endangering Abortion Performed due to Emotional/psychological Health of the Mother Abortion Performed due to Social or Economic Reasons Elective Abortion Sterilization Payer Responsible for Co-payment Air Ambulance Required Specialized Treatment/bed Unavailable - Alternate Facility Transport Non-emergency Medically Necessary Stretcher Transport Required Preadmission Screening Not Required Reserved for assignment by the NUBC Medicare Coordinated Care Demonstration Claim Beneficiary is Ineligible for Demonstration Program Critical Access Hospital Ambulance Attestation Pregnancy Indicator Admission Unrelated to Discharge on Same Day Reserved for assignment by the NUBC Gulf Oil Spill of 2010 (Effective 4/20/10) Reserved for assignment by the NUBC Approved as Billed Automatic Approval as Billed Based on Focused Review Partial Approval Admission/Services Denied Post Payment Review Applicable Admission Pre-authorization Extended Authorization Reserved for assignment by the NUBC (a) Code is acceptable for use in Professional Health Care Claim Implementation Guide (ASC X12N/005010X222) BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 20 Form Locator 18-28 Code Structure D0 D1 D2 D3 D4 D5 D6 D7 D8 D9 DA-DQ DR DS-DZ E0 E1-FZ G0 G1-GZ H0 H1 H2 H3 H4 H5 H6-LZ M0-MZ N0-OZ P0 P1 P2-P6 P7 P8-PZ Q0-UT UU UV-VZ W0 W1 W2(a) W3(a) W4(a) W5(a) W6-ZZ Changes to Service Dates Changes to Charges Changes in Revenue Codes/HCPCS/HIPPS Rate Codes Second or Subsequent Interim PPS Bill Change in clinical codes (ICD) for Diagnosis and/or Procedure Codes Cancel to Correct Insured’s ID or Provider ID Cancel Only to Repay a Duplicate or OIG Overpayment Change to Make Medicare the Secondary Payer Change to Make Medicare the Primary Payer Any Other Change Reserved for assignment by the NUBC Disaster Related Reserved for assignment by the NUBC Change in Patient Status Reserved for assignment by the NUBC Distinct Medical Visit Reserved for assignment by the NUBC Delayed Filing; Statement of Intent Submitted Reserved for assignment by the NUBC Discharge by a Hospice Provider for Cause (Effective 1/1/09) Reoccurrence of GI Bleed Comorbid Category (Effective 1/1/11) Reoccurrence of Pneumonia Comorbid Category (Effective 1/1/11) Reoccurrence of Pericarditis Comorbid Category (Effective 1/1/11) Reserved for assignment by the NUBC Reserved for payer assignment Reserved for assignment by the NUBC Reserved for Public Health Data Reporting Do Not Resuscitate Order (DNR) Reserved Public Health Data Reporting Direct Inpatient Admission from Emergency Room (Effective 7/1/10) Reserved Public Health Data Reporting Reserved for assignment by the NUBC Payer Code Reserved for assignment by the NUBC United Mine Workers of America (UMWA) Demonstration Indicator Reserved for assignment by the NUBC Duplicate of Original Bill Level I Appeal Level II Appeal Level III Appeal Reserved for assignment by the NUBC (a) Code is acceptable for use in Professional Health Care Claim Implementation Guide (ASC X12N/005010X222) BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 21 Form Locator 29 Data Element Accident State Definition: The accident state filed contains the two-digit state abbreviation where the accident occurred. Required If Applicable Reporting UB-04, 005010: Required when the services reported on this claim are related to an auto accident and the accident occurred in a country or location that has a state, province, or sub-country code named in X12 code source 22 (ISO 3166-2 Codes for the representation of names of countries and their subdivisions). 004010/004010A1: Not Used Field Attributes 1 Field 2 Positions 1 Line Alphanumeric Left-justified Notes Form Locator 30 Data Element Reserved for Assignment by the NUBC. Definition: Reporting Not Used Field Attributes 1 Field 2 Lines 13 Positions (lower line) 11 Positions (upper line) Alphanumeric Left-justified Form Locator 31-34 Data Element Occurrence Codes and Dates Definition: The code and associated date defining a significant event relating to this bill that may affect payer processing. Required If Applicable Reporting UB-04, 004010/004010A1, 005010: Situational. Required when there is an Occurrence Code that applies to this claim. Field Attributes 4 Fields 2 Lines 2 Positions Alphanumeric Left-justified (all positions fully coded) Notes Enter all dates as month, day, and year (MMDDYY) 4 Fields 2 Lines 6 Positions Numeric Right-justified Occurrence Codes should be entered in alphanumeric sequence (numbered codes precede alpha codes). BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 22 Form Locator 31-34 Code Structure 01 02 03 04 05 06 07-08 09 10 11 12 13-15 16 17 18 19 20 21 22 23 24 25 26 27 Accident/Medical Coverage No Fault Insurance Involved -Including Auto Accident/Other Accident/Tort Liability Accident/Employment Related Accident/No Medical or Liability Coverage Crime Victim Start of Infertility Treatment Cycle Last Menstrual Period Code indicating accident-related injury for which there is medical payment coverage. Provide the date of accident/injury. Code indicating the date of an accident including auto or other where state has applicable no fault liability laws (i.e., legal basis for settlement without admission of proof of guilt). Code indicating the date of an accident resulting from a third party’s action that may involve a civil court process in an attempt to require payment by the third party, other than no fault liability. Code indicating the date of an accident allegedly relating to the an accident allegedly relating to the patient’s employment. Code indicating accident related injury for which there is no medical payment or third-party liability coverage. Provide the date of accident/injury. Code indicating the date on which the medical condition resulted from alleged criminal action committed by one or more parties. Reserved for assignment by the NUBC. Code indicating the start date of infertility treatment cycle. Code indicating the date of the last menstrual period; ONLY applies when patient is being treated for maternity-related condition. Onset of Symptoms/ Code indicating the date the patient first became aware of the Illness symptoms/illness. Date of Onset for a (HHA Claims Only) Code denotes date the patient/beneficiary becomes a Chronically Dependent Chronically Dependent Individual (CDI). This is the first month of the 3 Individual month period immediately before eligibility under respite care benefit. Reserved for assignment by the NUBC Date of Last Therapy Code denotes last day of therapy services (e.g. physical therapy, occupational therapy, speech therapy). Date Outpatient Code denotes date an occupational therapy plan was established Occupational Therapy or last reviewed. Plan Established or Last Reviewed Date of Retirement The date of retirement for the patient/beneficiary. Patient/Beneficiary Date of Retirement The date of retirement for the patient’s spouse. Spouse Date Guarantee of Code indicates date on which the provider began claiming Medicare Payment Began payment under the guarantee of payment provision. Date UR Notice Code indicating the date of receipt by the provider of the UR Committee’s Received finding that the admission or future stay was not medically necessary. Date Active Care Code indicates the date covered level of care ended in a SNF or Ended general hospital, or date on which active care ended in a psychiatric or tuberculosis hospital, or date on which patient was released on a trial basis from a residential facility. Code not required when Condition Code 21 is used. Payer Code Date Insurance Denied Code indicating the date the denial of coverage was received by the health care facility from any insurer. Date Benefits Code indicating the date on which coverage (including Worker’s Terminated by Primary Compensation benefits of no-fault coverage) is no longer available to the Payer patient. Date SNF Bed Became Code indicating the date on which a SNF bed became available to Available(Inpatient) hospital inpatient who requires only SNF level of care. Date of Hospice Code indicating the date of certification or re-certification of the Certification or hospice benefit periods. Re-Certification BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 23 Form Locator 31-34 Code Structure 28 29 30 31 32 33 34 35 36 37 38 39 40 41 42 Date Comprehensive Code indicating the date a comprehensive outpatient rehabilitation Outpatient plan was established or last reviewed. Rehabilitation Plan Established or Last Reviewed Date Outpatient Code indicating the date a physical therapy plan was established Physical Therapy Plan or last reviewed. Established or Last Reviewed Date Outpatient Speech Code indicating the date a speech pathology plan was established Pathology Plan or last reviewed. Established or Last Reviewed Date Beneficiary The date of notice provided by the hospital to the patient that inpatient Notified of Intent to care is not longer required. Bill (Accommodations) Date Beneficiary The date of notice provided to the beneficiary that requested care Notified of Intent to (diagnostic procedures or treatments) may not be reasonable or Bill (Procedures or necessary. Treatments) First Day of the Code indicates the first day of coordination for benefits that are Coordination Period are secondary to benefits payable under an employer’s group health for ESRD Beneficiaries plan. Required only for ESRD beneficiaries. Covered by EGHP Date of Election of Code indicates the date the guest elected to receive extended Extended Care care services (used by Religious Non-Medical only). Facilities Date Treatment Started Code indicates the initial date services by the billing provider for for Physical Therapy physical therapy. Date of Inpatient Code indicates the date of discharge for inpatient hospital stay in which Hospital Discharge for the patient received a covered transplant procedure when the hospital Covered Transplant is billing for immunosuppressive drugs. Patients Note: When the patient received both a covered and a non-covered transplant, the covered transplant predominates. Date of Inpatient Code indicates the date of discharge for the inpatient hospital stay Hospital Discharge for in which the patient received a non-covered transplant procedure Non-Covered when the hospital is billing for immunosuppressive drugs. Transplant Patient Date Treatment Started Date the patient was first treated at home for IV therapy (Home IV for Home IV Therapy providers - Bill Type 085x). Date Discharged on a Date the patient was discharged from the hospital on a continuous Continuous Course of course of IV therapy. (Home IV providers - Bill Type 085x). IV Therapy Schedule Date of The scheduled date the patient will be admitted as an inpatient to the Admission hospital. (This code may only be used on an outpatient claim). Date of First Test for The date on which the first outpatient diagnostic test was performed as Pre-Admission Testing part of a PAT program. This code may only be used if a date of admission was scheduled before the administration of the test(s). Date of Discharge Use only when the “Through” date in Locator 06 (Statement Covers Period) is not the actual discharge date and the frequency code in Locator 04 is that of a final bill. For final bill for hospice care, enter the date the Medicare beneficiary terminated his election of hospice care. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 24 Form Locator 31-34 Code Structure 43 44 45 46 47 48-49 50 Scheduled Date of Canceled Surgery Date Treatment Started Occupational Therapy Date Treatment Started for Speech Therapy Date Treatment Started for Cardiac Rehabilitation Date Cost Outlier Status Begins Assessment Date 51 Date of Last Kt/V Reading 52 Medical Certification/ Recertification Date (Effective 1/1/11) 53 54 55 56-69 70-99 A0 A1 A2 A3 A4 A5-AZ B0 B1 B2 B3 B4-BZ C0 C1 C2 C3 C4-DQ DR DS-DZ E0 E1-E3 E4-EZ F0 The date for which outpatient surgery was scheduled. The date services were initiated by the billing provider for occupational therapy. The date services were initiated by the billing provider for speech therapy. The date services were initiated by the billing provider for cardiac rehabilitation. Code indicates that this is the first day after the day the Cost Outlier threshold is reached. Payer Codes Code indicating an assessment date as defined by the assessment instrument applicable tot this provider type (e.g., Minimum Data Sets (MDS) for skilled nursing). (Effective 1/1/11) For in-center hemodialysis patients, this is the date of the last reading taken during the billing period. For peritoneal dialysis patients (and home hemodiaysis patients, this date may be before the current billing period but should be within 4 months of the date of service. (Effective 07/01/10) The date of the most recent non-hospice medical certification or recertification of the patient. Use Occurrence Code 27 for Date of Hospice Certification of Recertification. Reserved for assignment by the NUBC Last date of a physician follow-up with the patient. Physician Follow-up Date (Effective 1/1/11) Date of Death Report his code when patient discharge status codes 20 (expired), 40 (Effective 10/1/12) (expired at home), 41 (expired in a medical facility, or 42 (expired – place unknown) are used. Reserved for assignment by the NUBC See instructions in Form Locators 35-36 Occurrence Span Codes and Dates Reserved for assignment by the NUBC Birth Date - Insured A The birth date of the individual in whose name the insurance is carried. Effective Date - Insured A code indicating the first date insurance is in force. A Policy Benefits Exhausted Code indicating the last date for which benefits are available and Payer A after which no payment can be made to Payer A. Split Bill Date Date patient became eligible due to medically needy spend down (sometimes referred as “Split Bill Date”). Reserved for assignment by the NUBC Reserved for assignment by the NUBC Birth Date - Insured B The birth date of the individual in whose name the insurance is carried. Effective Date - Insured A code indicating the first date insurance is in force. B Policy Benefits Exhausted Code indicating the last date for which benefits are available and after Payer B which no payment can be made by Payer B. Reserved for assignment by the NUBC Reserved for assignment by the NUBC Birth Date - Insured C The birth date of the individual in whose name the insurance is carried. Effective Date - Insured A code indicating the first date insurance is in force. C Policy Benefit Exhausted Code indicating the last date for which benefits are available and after Payer C which no payment can be made by Payer C. Reserved for assignment by the NUBC Reserved for Disaster Related Occurrence Code Reserved for assignment by the NUBC Reserved for assignment by the NUBC Discontinued 3/1/07 Reserved for assignment by the NUBC Reserved for assignment by the NUBC BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 25 F1 Discontinued 3/1/07 Form Locator 31-34 Code Structure F2 F3 F4-FZ Discontinued 3/1/07 Discontinued 3/1/07 Reserved for assignment by the NUBC G0 G1-G3 G4-LZ M0-ZZ Reserved for assignment by the NUBC Discontinued 3/1/07 Reserved for assignment by the NUBC See instructions in Form Locators 35-36 Occurrence Span Codes and Dates Form Locator 35-36 Data Element Occurrence Span Codes and Dates Definition: A code and the related dates that identify an event that relates to the payment of the claim. Required Reporting UB-04, 004010/004010A1, 005010: Situational. Required when there is an Occurrence Span Code that applies to this claim. Field Attributes 2 Fields (codes) 2 Lines 2 Positions Alphanumeric Left-justified (all positions fully coded) Notes These codes identify occurrences that happened over a span of time. Enter all dates as month, day, and year (MMDDYY). 4 Fields (dates) 2 Lines 6 Positions Numeric Right-justified Enter Occurrence Span Codes in alphanumeric sequence starting with code 70 and ending with ZZ (numbered codes precede alpha codes). If FL 35a&b and FL 36a&b have been filled and additional occurrence span codes are required, use FL 81 with the appropriate qualifier code (A3) to indicate that an Occurrence Span Code is being reported. Code Structure 70 71 72 73 74 75 Qualifying Stay Dates For SNF Use Only The from/through date of at least a 3 day inpatient hospital stay that qualifies the resident for Medicare payment of SNF services billed. Code can be used only by SNF for billing. Prior Stay Dates The from/through dates given by the patient of any hospital stay that ended within 60 days of this hospital or SNF admission. First/Last Visit Dates The from/through dates of outpatient services. For use on outpatient bills (Outpatient only) only where the entire billing record is not represented by the actual from/through service dates of Locator 06 (Statement Covers Period). Benefit Eligibility The inclusive dates during which TRICARE medical benefits are available Period to a sponsor’s beneficiary as shown on the beneficiary’s identification card. Non-Covered Level of The from/through dates of a period at a non-covered level of care Care/Leave of Absence or leave of absence in an otherwise covered stay, excluding any Dates period reported by Occurrence Span Code 76, 77, or 79 below. SNF Level of Care The from/through dates of a period of SNF level of care during BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 26 Dates an inpatient hospital stay. (Inpatient only) Form Locator 35-36 Code Structure 76 Patient Liability 77 Provider Liability Period SNF Prior Stay Dates 78 79 80 81 82-99 M0 Payer Code Prior Same-SNF Stay Dates for Payment Ban Purposes Antepartum Days at Reduced Level of Care (Effective 7/1/12) The from/through dates of a period of non-covered care for which the hospital is permitted to charge the Medicare beneficiary. Code should be used only where the QIO or intermediary has approved such charges in advance and patient has been notified in writing at least three days prior to the “from” date of this period. The from/through dates of a period of non-covered care for which the provider is liable; utilization is charged. The from/through dates given by the patient of any SNF or nursing home stay that ended within 60 days of this hospital or SNF admission. The from/through dates of a prior same-SNF stay indicating a patient resided in the SNF prior to, and if applicable, during a payment ban period up until their discharge to a hospital. (Effective 1/1/09) This code and corresponding dates indicate the from and through dates of an antepartum hospital stay where the level of care is non-acute. Reserve for assignment by the NUBC The first and last days that were approved where not all of the stay was approved. (Use when Condition Code C3 is used in Locators 18-28). M1 Code indicates the from/through dates of a period of non-covered care that is denied due to lack of medical necessity or as custodial care for which the provider is liable. The beneficiary is not charged with utilization. The provider may not collect Part A or Part B deductible or coinsurance from the beneficiary. M2 Inpatient Respite Dates The from/through dates of a period of inpatient respite care. M3 ICF Level of Care The from/through dates of a period of intermediate level of care during an inpatient hospital stay. M4 Residential Level of The from/through dates of a period of residential level of care during an Care inpatient hospital stay. M5-MQ Reserved for assignment by the NUBC MR Reserved for Disaster Related Occurrence Span Code MS-ZZ Reserved for assignment by the NUBC QIO/UR Approved Stay Dates Provider Liability - No Utilization Form Locator 37 Data Element Reserved for Assignment by the NUBC Reporting Not Used Field Attributes 1 Field 2 Lines 8 Positions Alphanumeric Left-justified Form Locator 38 Data Element Responsible Party Name and Address (Claim Addressee) Definition: The name and address of the party to whom the bill is being submitted. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 27 Required Required Form Locator 38 Reporting UB-04: Use to print the name and mailing address of the party deemed responsible for the bill (health plan, patient, etc.) if a window envelope is utilized. 004010/004010A1: Situational 005010: Not Used Field Attributes 1 Field Alphanumeric Notes Address may include post office box or street name and number, city, state and ZIP code. Hospitals should abbreviate state in the address according to the post office stand abbreviations appearing in the instructions for Locator 01. If a nine-digit ZIP code is used, it should be entered XXXXX-XXXX. 5 Lines Left-justified 40 Positions Form Locator 39-41 Data Element Value Codes and Amounts Definition: A code structure to relate amounts or values to identify data elements necessary to process this claim as qualified by the payer organization. Required If Applicable Reporting UB-04, 004010/004010A1, 005010: Situational. Required when there is a Value Code that applies to this claim. Field Attributes 3 Fields (codes) 4 Lines 2 Positions Alphanumeric Left-justified (all positions fully coded) Notes Whole numbers or non-dollar amounts are right-justified to the left of the dollars/cents delimiter. Enter value codes in alphanumeric sequence. Fields 39a through 41a must be completed before the b fields, etc. If all of the Value Code fields are filled, use FL 81 Code-Code field with the appropriate qualifier code (A4) to indicate that a Value Code is being reported. 3 Fields (amounts) 4 Lines 9 Positions Numeric Right-justified (see Notes) Code Structure 01 02 03 04 05 Most Common To provide for the recording of hospital’s most common semi-private Semi-Private Rate rate. Note: Required when billing private room revenue codes. Hospital has No Semi- Entering this code requires $0.00 amount. Private Rooms Reserved for assignment by the NUBC Professional Code indicates the amount shown is the sum of technical and professional Component Charges charges, which are combined, billed. Medicare uses this information in which are Combined internal processes and also in the CMS notice of utilization sent to the Billed patient to explain that Part B co-insurance applies to the professional component. (Used only by some all inclusive rate hospitals.) Professional Amount shown is the combined billed charges (technical and professional); Component Included in however the provider is submitting a separate professional bill to the health Charges and also Billed plan. For use on Medicare or TRICARE bills and all Medicaid bills if state BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 28 Separate to Carrier specifies need for this information. Form Locator 39-41 Code Structure 06 07 08 09 10 11 12 13 14 15 16 17-20 21 22 23 24 25 26 27 28 Blood Deductible Total cash blood deductible. If appropriate, enter Medicare Part A or Part B blood deductible amount. (To report other than the blood deductible, that is to report the program deductible, see Value Codes (FL 39-41) A1, B1 and C1. Reserved for assignment by the NUBC Life Time Reserve Lifetime reserve amount charged in the year of admission. Amount in the First Note: For Medicare, use this code only for Part A bills. For Part B Calendar Year Coinsurance use Value Codes (FL 39-41) A2, B2 and C2. Coinsurance Amount Coinsurance amounts charged in the year of admission. in the First Calendar Year Lifetime Reserve Lifetime reserve amount charged in the year of discharge where the bill Amount in the Second spans two calendar years. Calendar Year Coinsurance Amount Coinsurance amount charged in the year of discharge where the inpatient in the Second Calendar bill spans two calendar years. Year Working Aged Amount shown reflects that portion of a payment from a higher priority Beneficiary/Spouse employer group health insurance made on behalf of an aged beneficiary. With Employer Group For Medicare purposes the provider is billing Medicare as the secondary Health Plan payer (based on MSP development) for covered services on this bill. ESRD Beneficiary in a Amount shown is that portion of a payment from a higher priority employer Medicare Coordination group health insurance payment made on behalf of an ESRD beneficiary Period with an that the provider is applying to Medicare covered services on this bill. Employer Group Health Plan No-Fault, Including Amount shown is that portion from a higher priority no-fault insurance, Auto/Other including auto/other made on behalf of the patient or insured. Worker’s Amount shown is that portion of payment from a higher priority worker’s Compensation compensation insurance made on behalf of the patient or insured. For Medicare beneficiaries the provider should apply this amount to Medicare covered services on this bill. PHS, or Other FederalAmount shown is that portion of a payment from a higher priority Public Agency Health Service or the Federal Agency made on behalf of a Medicare beneficiary that the provider is applying to Medicare covered services on this bill. Payer Code Catastrophic Medicaid-eligibility requirements to be determined at state level. Surplus Medicaid-eligibility requirements to be determined at state level. Recurring Monthly Medicaid-eligibility requirements to be determined at state level. Income Medicaid Rate Code Medicaid-eligibility requirements to be determined at state level. Offset to the PatientPrescription drugs paid for out of a long-term care facility Payment Amount resident/patient’s funds in the billing period submitted (Statement Prescription Drugs Covers Period). Offset to the PatientHearing and ear services paid for out of a long-term care facility Payment Amount resident/patient’s funds in the billing period submitted (Statement Hearing and Ear Covers Period). Services Offset to the PatientVision and eye services paid for out of a long-term care facility Payment Amount resident/patient’s funds in the billing period submitted (Statement Vision and Eye Covers Period). Services Offset to the PatientDental services paid for out of a long-term care facility Payment Amount resident/patient’s funds in the billing period submitted (Statement Dental Services Covers Period). BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 29 Form Locator 39-41 Code Structure 29 30 31 32 33 34 35 36 37 38 39 40 41 42 43 44 Offset to the PatientPayment Amount Chiropractic Services Preadmission Testing Chiropractic services paid for out of a long-term care facility resident/patient’s funds in the billing period submitted (Statement Covers Period). This code reflects charges for preadmission outpatient diagnostic services in preparation for a previously scheduled admission. Patient Liability Approved amount to charge the beneficiary for non-covered Amount accommodations, diagnostic procedures or treatments. Multiple Patient When more than one patient is transported in a single ambulance Ambulance Transport trip, report the total number of patients transported. Offset to the PatientPodiatric services paid for out of a long-term care facility Payment Amount resident/patient’s funds in the billing period submitted (Statement Podiatric Services Covers Period). Offset to the PatientOther medical services paid for out of a long-term care facility Payment Amount resident/patient’s funds in the billing period submitted (Statement Other Medical Services Covers Period). Offset to the PatientHealth insurance premiums paid for out of a long-term care facility Payment Amount resident/patient’s funds in the billing period submitted (Statement Health Insurance Covers Period). Premiums Reserved for assignment by the NUBC Units of Blood The total number of units of whole blood or packed red cells Furnished furnished to the patient, regardless of whether the hospital charges for blood or not. Blood Deductible Units The number of unreplaced deductible units of packed red cells furnished for which the patient is responsible. If all deductible units furnished have been replaced, no entry is made. Units of Blood The total number of units of whole blood or packed red cells Replaced furnished to the patient that have been replaced by or on behalf of the patient. New Coverage not Amount shown is for inpatient charges covered by the HMO. (Use this code Implemented by HMO when the bill includes inpatient charges for newly covered services that are (for inpatient service) not paid by the HMO.) Note: Condition Codes 04 and 78 should also be reported. Black Lung Code indicates the amount shown is that portion of a higher priority Black Lung (federal program) payment made on behalf of a Medicare beneficiary. VA (Veteran’s Code indicates the amount shown is that portion of a higher priority Administration) VA payment made on behalf of a Medicare beneficiary and that you are applying to Medicare as secondary payer for covered Medicare services on this claim. Disabled Beneficiary Code indicates the amount shown is that portion of a higher priority Under Age 65 with LGHP payment made on behalf of a disabled beneficiary that you are LGHP applying to covered Medicare charges on this bill. Amount Provider Report the amount the provider was obligated to accept from a primary Agreed to Accept frompayer when the amount is less than charges but higher than or equal to the Primary Payer when payment received. Secondary payment may be due. this Amount is less than Note: The following value codes report the actual amounts paid: 12-16, Charges but Higher 41-43, and 47. Value Code 44 should always be equal to, or, greater than than Payment the amounts indicated in the value codes indicated immediately above. Received BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 30 Form Locator 39-41 Code Structure 45 46 47 made 48 49 50 51 52 53 54 55 Accident Hour The hour when the accident occurred that necessitated medical treatment. Enter the appropriate code indicated below right justified to the left of the dollar/cents delimiter. 00 12:00 - 12:59 (midnight) 13 01:00 - 01:59 01 01:00 - 01:59 14 02:00 - 02:59 02 02:00 - 02:59 15 03:00 - 03:59 03 03:00 - 03:59 16 04:00 - 04:59 04 04:00 - 04:59 17 05:00 - 05:59 05 05:00 - 05:59 18 06:00 - 06:59 06 06:00 - 06:59 19 07:00 - 07:59 07 07:00 - 07:59 20 08:00 - 08:59 08 08:00 - 08:59 21 09:00 - 09:59 09 09:00 - 09:59 22 10:00 - 10:59 10 10:00 - 10:59 23 11:00 - 11:59 11 11:00 - 11:59 12 12:00 - 12:59 (Noon) Number of Grace Days Following the QIO determination. This is the number of days determined by the QIO (medical necessity reviewer) as necessary to arrange for the patient’s post-discharge care. Any Liability Insurance Amount shown is that portion from a higher priority liability insurance on behalf of a Medicare beneficiary that the provider is applying to Medicare or Blue Cross covered services on this bill. Note: The decimal is implied and refers to the dollar and cents delimiter. Hemoglobin Reading The most recent hemoglobin reading taken before the start of this billing period. For patients just starting, use the most recent value prior to the onset if treatment. Whole numbers, i.e., two digits are to be right justified to the left of the dollar/cents delimiter; decimals, i.e., one digit, is to be reported to the right. Hematocrit Reading The most recent hematocrit reading taken before the start of this billing period. For patients just starting, use the most recent value prior to the onset if treatment. Whole numbers, i.e., two digits are to be right justified to the left of the dollar/cents delimiter; decimals, i.e., one digit, is to be reported to the right. Physical Therapy Visit Report the number of physical therapy visits provided from the onset of treatment from this billing provider through this billing period. Report the number in the dollar portion of the form locator right justified to the left of the dollar/cents delimiter. Occupational Therapy Report the number of occupational therapy visits provided from the onset of Visits treatment from this billing period. Report the number in the dollar portion of the locator right justified to the left of the dollar/cents delimiter. Speech Therapy Visits Report the number of speech therapy visits provided from the onset of treatment by this billing provider through this period. Report the number in the dollar portion of the locator right justified to the left of the dollar/cents delimiter. Cardiac Rehabilitation The number of cardiac rehabilitation visits from the onset of treatment Visits from the billing provider through this billing period. Report the number in the dollar portion of the locator right justified to the left of the dollar/cents delimiter. Newborn Birth Weight Actual birth weight or weight at time of admission for an extramural birth. in Grams Required on all claims with Type of Admission of 4 and on other claims as required by state law. Eligibility Threshold The amount at which a health care facility determines the eligibility BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 31 for Charity Care threshold for charity care. Form Locator 39-41 Code Structure 56 Skilled Nurse-Home Visit Hours (HHA only) 57 Home Health AideHome Visit Hours (HHA only) 58 Arterial Blood Gas (PO2/PA2) 59 Oxygen Saturation (O2 SAT/Oximetry) 60 HHA Branch MSA 61 Place of Residence Where Service is Furnished (HHA and Hospice) Payer Codes Medicaid Spend Down The dollar amount that was used to meet the recipient’s spend down Amount liability for this claim. Peritoneal Dialysis The number of hours of peritoneal dialysis provided during the billing period. Count only the hours spent in the home. Exclude travel time. Report in whole hours, right justify to the left of the dollar/cent delimiter. (Round to the nearest whole hour.) EPO-Drug Number of units of EPO administered and/or supplied relating to the billing period. Report amount in whole units right justified to the left of the dollar/cents delimiter. State Charity Care Code indicates the percentage of charity care eligibility for the patient. Percent Report the whole number right justified to the left of the dollar/cents delimiter and fractional amounts to the right. For example, a rate of 10.5% is shown as: 1050 Payer Codes Covered Days The number of days covered by the primary payer as qualified by the 62-65 66 67 68 69 The number of home visit hours of skilled nursing provided during the billing period. Count only hours spent in the home. Exclude travel time. Report in whole hours, right justified to the left of the dollar/cents delimiter. (Round to the nearest whole hour). The number of hours of home health aide services provided during the billing period. Count only the hours spent in the home. Exclude travel time. Report in whole hours, right justified to the left of the dollar/cents delimiter. (Round to the nearest whole hour). Arterial blood gas value at beginning of each reporting period for oxygen therapy. This value or the value in Value Code 59 will be required on the initial bill for oxygen therapy and on the fourth month’s bill. Report right justified in the cents area rounded to the nearest whole number (report 2 digits). Example: A value of 56.5 should be reported as 000000 57, i.e., with the 57 reported in the cents area. Oxygen saturation at the beginning of each reporting period for oxygen therapy. This value or the value in Value Code 58 will be required on the initial bill for oxygen therapy and on the fourth month’s bills. Report right justified in the cent area. Round to the nearest whole percent (report 2 digits). Example: 93.5 percent should be reported as 000000 94, i.e., with 94 being reported in the cents area. A value of 100 percent would be reported as 000001 00. MSA in which HHA branch is located. Report MSA when branch location is different than the HHA’s. Report the MSA number in dollar portion of the form locator right justified to the left of the dollar/cents delimiter. MSA or Core Based Statistical Area (CBSA) number (or rural state code) of the place of residence where the home health or hospice service is delivered. Report the number in dollar portion of the form locator right justified to the left of the dollar/cents delimiter. 70-79 80(a) payer. 81(a) Non-Covered Days 82(a) Co-insurance Days 83(a) Days of care not covered by the primary payer. The inpatient Medicare days occurring after the 60th day and before the 91st day or inpatient SNF/Swing Bed days occurring after the 20th and before the 101st day in a single spell of illness. Lifetime Reserve Days Under Medicare, each beneficiary has a lifetime reserve of 60 additional days of inpatient hospital services after using 90 days of inpatient hospital services during a spell of illness. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 32 84-99 Reserved for assignment by the NUBC. (a) Do not use on v. 004010/004010A1 837 electronic claims (use Claim Quantity in Loop ID 2300 / QTY01 instead). Form Locator 39-41 Code Structure A0 Special ZIP Code Reporting Deductible Payer A Five digit ZIP Code of the location from which the beneficiary is initially placed on board the ambulance. A1(b) The amount assumed by the provider to be applied to the patient’s policy/program deductible amount involving the indicated payer. Note: Report Medicare blood deductibles under Value Code 06. Required for Blue Cross claims when billing for balance after Medicare. A2(b) Coinsurance Payer A The amount assumed by the provider to be applied toward the patient’s coinsurance amount involving the indicated payer. Note: For Medicare, use this code only for reporting Part B coinsurance amounts. For Part A coinsurance amounts use Value Codes 8-11. Required for Blue Cross claims when billing for balance after Medicare. A3 Estimated The amount estimated by the provider to be paid by the indicated payer; Responsibility Payer A it is not the actual payment. A4 Covered SelfThe covered charge amount for self-administrable drugs administered to the Administrable Drugs - patient in an emergency situation (e.g., diabetic coma). For use with Emergency Revenue Code 0637. A5 Covered SelfThe amount included in covered charges for self-administrable drugs administrable Drugs - administered to the patient because the drug was not self-administrable in the not Self-administrable form and situation in which it was furnished to the patient. in the form and For use with Revenue Code 0637. Situation Furnished to Patient A6 Covered SelfThe amount assumed by the provider to be applied toward the patient’s Administrable Drugs - co-payment amount involving the indicated payer. Diagnostic Study and Other A7(b) Co-payment Payer A The amount assumed by the provider to be applied toward the patient’s co-payment amount involving the indicated payer. A8 Patient Weight Weight of patient in kilograms. Report this data only when the health plan has a predefined change in reimbursement that is affected by weight. For newborns, use Value Code 54. A9 Patient Height Height of patient in centimeters. Report this data only when the health plan has a predefined change in reimbursement that is affected by height. AA Regulatory Surcharges, The amount of regulatory surcharges, assessments, allowances or Assessments, health care related taxes pertaining to the indicated payer. Allowances or Health Care Related Taxes Payer A AB Other Assessments or The amount of other assessments or allowances (e.g., medical Allowances (e.g., education) pertaining to the indicated payer. Medical Education) Payer A AC-AZ Reserved for assignment by the NUBC B0 Reserved for assignment by the NUBC B1(b) Deductible Payer B The amount assumed by the provider to be applied to the patient’s policy/program deductible amount involving the indicated payer. Note: Medicare blood deductibles should be reported under Value Code 06. B2(b) Coinsurance Payer B The amount assumed by the provider to be applied toward the patient’s coinsurance amount involving the indicated payer. For Part A coinsurance amounts use Value Codes 08-11. B3 Estimated The amount estimated by the provider to be paid by the indicated payer; Responsibility Payer B it is not the actual payment. B4-B6 Reserved for assignment by the NUBC BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 33 (b) This code is to be used only on paper claims. For electronic 837 claims, use Loop ID 2320 CAS segment (Claim Adjustment Group Code “PR”). Form Locator 39-41 Code Structure B7(b) B8-B9 BA BB BC-C0 C1(b) C2(b) C3 C4-C6 C7(b) C8-C9 CA CB CC-D2 D3 D4 D5 D6-DQ DR DS-DZ E0 E1 E2 E3 E4-E6 E7 E8-E9 Co-payment Payer B The amount assumed by the provider to be applied toward the patient’s co-payment amount involving the indicated payer. Reserved for assignment by the NUBC Regulatory Surcharges, The amount of regulatory surcharges, assessments, allowances or health Assessments, care related taxes pertaining to the indicated payer. Allowances or Health Care Related Taxes Payer B Other Assessments or The amount of other assessments or allowances (e.g., medical Allowances (e.g., education) pertaining to the indicated payer. Medical Education) Payer B Reserved for assignment by the NUBC Deductible Payer C The amount assumed by the provider to be applied to the patient’s policy/program deductible amount involving the indicated payer. Note: Medicare Blood deductibles should be reported under Value Code 06. Coinsurance Payer C The amount assumed by the provider to be applied toward the patient’s coinsurance amount involving the indicated payer. For Part A coinsurance amounts use Value Codes 08-11. Estimated The amount estimated by the provider to be paid by the indicated payer; Responsibility Payer C it is not the actual payment. Reserved for assignment by the NUBC Co-payment Payer C The amount assumed by the provider to be applied toward the patient’s co-payment amount involving the indicated payer. Reserved for assignment by the NUBC Regulatory Surcharges, The amount of regulatory surcharges, assessments, allowances Assessments, or health care related taxes pertaining to the indicated payer. Allowances or Health Care Related Taxes Payer C Other Assessments or The amount of other assessments or allowances (e.g., medical Allowances (e.g., education) pertaining to the indicated payer. Medical Education) Payer C Reserved for assignment by the NUBC. Patient Estimated The amount estimated by the provider to be paid by the Responsibility indicated patient. Clinical Trial Number 8-digit, numeric National Library of Medicine/National Institutes of Health Assigned by NLM/NIH assigned clinical trail number. Last Kt/V Reading Result of the last Kt/V reading. For in-center hemodialysis patients, this is the last reading taken during the billing period. For peritoneal dialysis patients (and home hemodialysis patients), this may be before the current billing period but should be within 4 months of the date of service. Note: Only report on FL 04 Type of Bill 072x. (Effective 07/01/10) Reserved for assignment by the NUBC Reserved for Disaster Related Value Code Reserved for assignment by the NUBC Reserved for assignment by the NUBC Discontinued 3/1/07 Discontinued 3/1/07 Discontinued 3/1/07 Reserved for assignment by the NUBC Discontinued 3/1/07 Reserved for assignment by the NUBC BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 34 EA Discontinued 3/1/07 EB Discontinued 3/1/07 EC-EZ Reserved for assignment by the NUBC (b) This code is to be used only on paper claims. For electronic 837 claims, use Loop ID 2320 CAS segment (Claim Adjustment Group Code “PR”). Form Locator 39-41 Code Structure F0-F3 F4-F6 F7 F8-F9 FA-FB FC Patient Paid Amount FD FE-G0 G1-G3 G4-G6 G7 G8 G9 GA GB GC-OZ P0-PZ Q0-Y0 Y1 Y2 Y3 Y4 Y5-ZZ Discontinued 3/1/07 Reserved for assignment by the NUBC Discontinued 3/1/07 Reserved for assignment by the NUBC Discontinued 3/1/07 The amount the provider has received from the patient toward payment of this bill. (Effective 7/1/08) Credit Received from The amount the provider has received from a medical device manufacturer the Manufacturer for a as credit fro a replaced device. (Effective 7/1/08) Replaced Medical Device Reserved for assignment by the NUBC Discontinued 3/1/07 Reserved for assignment by the NUBC Discontinued 3/1/07 Facility where Inpatient MSA or Core Based Statistical Area (CBSA) number (or rural state code) of Hospice Service is the facility where inpatient hospice service is delivered. Report the number in Delivered dollar portion of the form locator right justified to the left of the dollar/cents delimiter. Reserved for assignment by the NUBC Discontinued 3/1/07 Discontinued 3/1/07 Reserved for assignment by the NUBC Reserved for PUBLIC HEALTH DATA REPORTING Reserved for assignment by the NUBC Part A Demonstration This is the portion of the payment designated as reimbursement for Payment Part A services under the demonstration. This amount is instead of the traditional prospective DRG payment (operating and capital) as well as any outlier payments that might have been applicable in the absence of the demonstration. No deductible or coinsurance has been applied. Payments for operating IME and DSH which are processed in the traditional manner are also not included in this amount. Part B Demonstration This is the portion of payment designed as reimbursement for Part B Payment services under the demonstration. No deductible or coinsurance has been applied. Part B Coinsurance This is the amount of Part B coinsurance applied by the intermediary to this claim. For demonstration claims this will be a fixed copayment unique to each hospital and DRG (or DRG/procedure group). Conventional Provider This is the amount Medicare would have reimbursed the provider for Payment Amount for Part A services if there had been no demonstration. This should include Non-Demonstration the prospective DRG payment (both capital as well as operational) as well Claims as any outlier payment, which would be applicable. It does not include any pass through amounts such as that for direct medical education nor interim payments for operating IME and DSH. Reserved for assignment by the NUBC BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 35 Form Locator 42 Data Element Revenue Code Definition: Codes that identify specific accommodation, ancillary service or unique billing calculations or arrangements. Required Yes Reporting UB-04, 004010/004010A1, 005010: Required Field Attributes 1 Field Alphanumeric 23 Lines (a) 4 Positions Left-justified (all positions filled) (a) The 23rd line contains an incrementing page count and total number of pages for the claim on each page, creation date of the claim on each page, and a claim total for covered and non-covered charges on the final claim page only indicated using Revenue Code 0001. (b) On a multiple page UB-04, all of the (claim level) information is repeated on each page: only the line items in the revenue code section will vary. Notes Revenue Code categories are four digits with an “x” in the fourth position to denote the subcategory number. The subcategory number provides a more detailed list generally ranging from “0” through “9”. When reporting the revenue code on the claim, the fourth position must include one of the numeric choices available in that category. The reporting of an “x” is not appropriate. The “0” in many cases denotes the “General” category and can be used in lieu of other more specific subcategories (“1” through “9”) if the health plan has no need for a more specific revenue code subcategory. Health plans receiving such detail, without a need for that detail, should accept the subcategory and treat it as though it was reported at the “General” level. Nonetheless, it is recommended that providers use the more detailed subcategory when applicable/available rather than revenue codes that end in “0” (General) or “9” (Other); to do otherwise may cause processing delays for the claim. Each service should be assigned a revenue code. For inpatient services involving multiple services for the same item providers should aggregate the services under the assigned revenue code and then report the total number of units that represent those services. For outpatient services providers should report the corresponding HCPCS code for the service along with the date of service as well as the revenue code. If multiple services are provided on the same day for like services, that is, those with the same HCPCS, the provider should aggregate the like services for each day and report the date along with a number of units provided, as well as the revenue code. The exception is for Evaluation and management (E/M) HCPCS. For E/M HCPCS, report each of these separately but also use Condition Code “G0” to indicate a Distinct Medical Visit. Services provided on different days should be listed separately along with the date of service, units and revenue code. Revenue codes should be listed in ascending numeric order, by date of service BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 36 (outpatient). The exception is Revenue Code 0001 - Total Charge, which is used on paper claims only and is reported on Line 23 of the last page of the claim. Form Locator 42 Notes The Standard Abbreviation is intended for use in the provider’s Charge Description Master and is not reported on electronic claims. The HCPCS usage notations in the revenue code section (FL42) are provided for general guidance only; they do not represent hard and fast rules. Actual application may vary depending on certain circumstances. Revenue Code Changes from UB-92 In the process of developing the UB-04, the “9 - Other” revenue subcategory codes were reviewed for necessity, clarity and redundancy. As a result several “9” codes were re-designated as reserved for assignment by the NUBC because the “0 - General Classification” codes are sufficient. Specific revenue codes removed from UB-92 include 0599, 0709, 0719, 0749, 0759, 0779, 0789 and 0799. For clarity, RC 0392 was added to UB-04 to distinguish “Processing and Storage” from “Other” (RC 0399). In addition, any unused code in UB-92 has been specifically designated as “RESERVED” in UB-04. These changes are not reflected in any UB-92 update. As noted on FL42, the changes are effective 3/1/07 (for UB-04 claims). 0001 TOTAL CHARGE Report Revenue Code 0001 on paper claims only. No allowed on electronically submitted claims. 0002 to 0009 RESERVED 001x RESERVED FOR INTERNAL PAYER USE 002x HEALTH INSURANCE - PROSPECTIVE PAYMENT SYSTEM (HIPPS) This revenue code is used to denote that a HIPPS rate code is being reported in FL44. Sub-Category 0 RESERVED 1 RESERVED 2 Skilled Nursing Facility - PPS 3 Home Health - PPS 4 Inpatient Rehab Facility - PPS 5-9 RESERVED 003x to 009x 010x Standard Abbreviation SNF PPS (RUG) HH PPS (HRG) REHAB PPS (CMG) RESERVED ALL INCLUSIVE RATE Flat fee charge incurred on either a daily basis or total stay basis for service rendered. Charge may cover room and board plus ancillary services and board only. Sub-Category 0 All Inclusive Room and BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation All INCL R & B/ANC Unit Days HCPCS N Page 37 Board plus Ancillary. 1 All Inclusive Room and Board. 2-9 RESERVED All INCL R & B Days N Form Locator 42 011x ROOM & BOARD - PRIVATE (ONE BED) Routine service charges for accommodations in a private room (1 bed). Sub-Category 0 General Classification 1 Medical/Surgical/GYN 2 Obstetrics (OB) 3 Pediatric 4 Psychiatric 5 Hospice 6 Detoxification 7 Oncology 8 Rehabilitation 9 Other Standard Abbreviation ROOM-BOARD/PVT MED-SURG-GY/PVT OB/PVT PEDS/PVT PSYCH/PVT HOSPICE/PVT DETOX/PVT ONCOLOGY/PVT REHAB/PVT OTHER/PVT Unit Days Days Days Days Days Days Days Days Days Days HCPCS N N N N N N N N N N Unit Days Days Days Days Days Days Days Days Days Days HCPCS N N N N N N N N N N Unit Days Days Days Days Days Days Days Days Days Days HCPCS N N N N N N N N N N Note: Most health plans require private rooms be separately identified. 012x ROOM & BOARD - SEMI-PRIVATE (Two Beds) Routine service charges for accommodations in a semi-private room (2 beds). Sub-Category 0 General Classification 1 Medical/Surgical/GYN 2 Obstetrics (OB) 3 Pediatric 4 Psychiatric 5 Hospice 6 Detoxification 7 Oncology 8 Rehabilitation 9 Other 013x Standard Abbreviation ROOM-BOARD/SEMI MED-SURG-GY/SEMI OB/SEMI-PVT PEDS/SEMI-PVT PSYCH/SEMI-PVT HOSPICE/SEMI-PVT DETOX/SEMI-PVT ONCOLOGY/SEMI REHAB/SEMI-PVT OTHER/SEMI-PVT ROOM & BOARD - THREE and FOUR BEDS Routine service charges incurred for rooms containing three or four beds. Sub-Category 0 General Classification 1 Medical/Surgical/GYN 2 Obstetrics (OB) 3 Pediatric 4 Psychiatric 5 Hospice 6 Detoxification 7 Oncology 8 Rehabilitation 9 Other BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation ROOM-BOARD/3 & 4 BED MED-SURG-GY/3 & 4 BED OB/3 & 4 BED PEDS/3 & 4 BED PSYCH/3 & 4 BED HOSPICE/3 & 4 BED DETOX/3 & 4 BED ONCOLOGY/3 & 4 BED REHAB/3 & 4 BED OTHER/3 & 4 BED Page 38 Form Locator 42 014x ROOM & BOARD - DELUXE PRIVATE Deluxe accommodations substantially in excess of private room services. Sub-Category 0 General Classification 1 Medical/Surgical/GYN 2 Obstetrics (OB) 3 Pediatric 4 Psychiatric 5 Hospice 6 Detoxification 7 Oncology 8 Rehabilitation 9 Other 015x Standard Abbreviation ROOM-BOARD/DLX PVT MED-SURG-GY/DLX PVT OB/DLX PVT PEDS/DLX PVT PSYCH/DLX PVT HOSPICE/DLX PVT DETOX/DLX PVT ONCOLOGY/DLX PVT REHAB/DLX PVT OTHER/DLX PVT Unit Days Days Days Days Days Days Days Days Days Days HCPCS N N N N N N N N N N Unit Days Days Days Days Days Days Days Days Days Days HCPCS N N N N N N N N N N ROOM AND BOARD - WARD Routine service charges for accommodations with five or more beds. Sub-Category 0 General Classification 1 Medical/Surgical/GYN 2 Obstetrics (OB) 3 Pediatric 4 Psychiatric 5 Hospice 6 Detoxification 7 Oncology 8 Rehabilitation 9 Other 016x Standard Abbreviation ROOM-BOARD/WARD MED-SURG-GY/WARD OB/WARD PEDS/WARD PSYCH/WARD HOSPICE/WARD DETOX/WARD ONCOLOGY/WARD REHAB/WARD OTHER/WARD ROOM AND BOARD - OTHER Any routine service charges for accommodations that cannot be included in the more specific revenue center codes. Sterile environment is a room and board charge to be used by hospitals that are currently separating this charge for billing. Sub-Category 0 General Classification 1-3 RESERVED 4 Sterile Environment 5-6 RESERVED 7 Self-Care 8 RESERVED 9 Other BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation R&B Unit Days HCPCS N R&B/STERILE Days N R&B/SELF Days N R&B/OTHER Days N Page 39 Form Locator 42 017x NURSERY Accommodation charges for nursing care to newborns and premature infants in nurseries. Sub-Category 0 General Classification 1 Newborn – Level I 2 Newborn – Level II 3 Newborn – Level III 4 Newborn – Level IV 5-8 RESERVED 9 Other Nursery Standard Abbreviation NURSERY NURSERY/LEVEL I NURSERY/LEVEL II NURSERY/LEVEL III NURSERY/LEVEL IV Unit Days Days Days Days Days HCPCS N N N N N NURSERY/OTHER Notes: If used in conjunction with other room charges (i.e., the mother’s room charges), the units for this revenue code is not included into the grand total, (i.e., revenue code 001 units). The levels of care correlate to the intensity of medical care provided to an infant and not the NICU facility certification level assigned by the state. Level I: Routine care of apparently normal full-term or pre-term neonates. (Newborn Nursery) Level II: Low birth-weight neonates who are not sick, but require frequent feeding, and neonates who require more hours of nursing than do normal neonates. (Continuing Care/Premature) Level III: Sick neonates, who do not require intensive care, but require 6-12 hours of nursing each day. (Intermediate Care) Level IV: Constant nursing and continuous cardiopulmonary and other support for severely ill infants. (Intensive Care) 018x LEAVE OF ABSENCE Charges for holding a room while the patient is temporarily away from the provider Sub-Category 0 General Classification 1 RESERVED 2 Patient Convenience 3 Therapeutic Leave 4 RESERVED 5 Nursing Home (for Hospitalization) 6-8 RESERVED 9 Other Leave of Absence Note: Standard Abbreviation Leave of Absence or LOA Unit Days HCPCS N LOA/PT CONV LOA/THERAPEUTIC Days Days N N LOA/NURS HOME Days N LOA/OTHER Days N This field requires the units field to be entered; however, the units must not be added to the grand total (i.e., revenue code 001). BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 40 Form Locator 42 019x SUBACUTE CARE Accommodations charges for subacute care to inpatients or skilled nursing facilities Sub-Category 0 General Classification 1 Subacute Care – Level I 2 Subacute Care – Level II 3 Subacute Care – Level III 4 Subacute Care – Level IV 5-8 RESERVED 9 Other Subacute Care Standard Abbreviation SUBACUTE SUBACUTE/LEVEL I SUBACUTE/LEVEL II SUBACUTE/LEVEL III SUBACUTE/LEVEL IV Unit Days Days Days Days Days HCPCS N N N N N SUBACUTE/OTHER Days N Usage Note: Revenue code 19X may be used in multiple types of bills. However, if Bill Type X7X is used in Form Locator 4, Revenue code 019X must be used Level I - Skilled Care: Minimal nursing intervention. Comorbidities do not complicate treatment plan. Assessment of vitals and body systems required 1-2 times per day. Level II - Comprehensive Care: Moderate nursing intervention. Active treatment of comorbidities. Assessment of vitals and body systems required 2-3 times per day. Level III - Complex Care: Moderate to extensive nursing intervention. Active medical care and treatment of comorbidities. Potential for comorbidities to affect the treatment plan. Assessment of vitals and body systems required 3-4 times per day. Level IV - Intensive Care: Extensive nursing and technical intervention. Active medical care and treatment of comorbidities. Potential for comorbidities to affect the treatment plan. Assessment of vitals and body systems required 4-6 times per day. 020x INTENSIVE CARE UNIT Routine service charges for medical or surgical care provided to patients who require a more intensive level of care that is rendered in the general medical or surgical unit. Sub-Category 0 General Classification 1 Surgical 2 Medical 3 Pediatric 4 Psychiatric 5 RESERVED 6 Intermediate ICU 7 Burn Care 8 Trauma 9 Other Intensive Care 021x Standard Abbreviation INTENSIVE CARE (ICU) ICU/SURGICAL ICU/MEDICAL ICU/PEDS ICU/PSYCH Unit Days Days Days Days Days HCPCS N N N N N ICU/INTERMEDIATE ICU/BURN CARE ICU/TRAUMA ICU/OTHER Days Days Days Days N N N N CORONARY CARE UNIT Routine service charges for medical care provided to patients with coronary illness who require a more intensive level of care than is rendered in the general medical or surgical unit. Sub-Category 0 General Classification 1 Myocardial Infarction 2 Pulmonary Care 3 Heart Transplant BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation CORONARY CARE (CCU) CCU/MYO INFARC CCU/PULMONARY CCU/TRANSPLANT Unit Days Days Days Days HCPCS N N N N Page 41 4 Intermediate CCU 5-8 RESERVED 9 Other Coronary Care CCU/INTERMEDIATE Days N CCU/OTHER Days N Report when a discrete coronary care unit exists for rendering such services. Form Locator 42 022x SPECIAL CHARGES Charges incurred during an inpatient stay or on a daily basis for certain services. Sub-Category 0 General Classification 1 Admission Charges 2 Technical Support Charge 3 U.R. Service Charge 4 Late Discharge, Medically Necessary 5-8 RESERVED 9 Other Special Charges Standard Abbreviation SPECIAL CHARGES ADMIT CHARGE TECH SUPPORT CHG UR CHARGE LATE DISCH/MED NEC Unit OTHER SPEC CHG HCPCS N N N N N N Some hospitals may prefer to identify the components of services rendered in greater detail and thus break out charges that normally would be considered part of routine services. 023x INCREMENTAL NURSING CHARGE Extraordinary charges for nursing services assessed in addition to the normal nursing charge associated with the typical room and board unit. Sub-Category 0 General Classification 1 Nursery 2 OB 3 ICU 4 CCU 5 Hospice 6-8 RESERVED 9 Other 024x Standard Abbreviation NURSING INCREM NUR INCR/NURSERY NUR INCR/OB NUR INCR/ICU NUR INCR/CCU NUR INCR/HOSPICE Unit Hours Hours Hours Hours Hours Hours HCPCS N N N N N N NUR INCR/OTHER Hours N ALL INCLUSIVE ANCILLARY A flat rate charge that is applied on a daily basis or on a total stay basis for ancillary services only. Sub-Category 0 General Classification 1 Basic 2 Comprehensive 3 Specialty 4-8 RESERVED 9 Other All Inclusive Ancillary Standard Abbreviation All INCL ANCIL All INCL BASIC All INCL COMP All INCL SPECIAL All INCL ANCIL/OTHER Unit HCPCS N N N N N Note: Revenue codes 0241, 0242 and 0243 are designed for use by Special Residential Facilities only. See Form Locator 4, Type of Bill 086x. Hospitals billing in this manner may wish to segregate these charges. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 42 Form Locator 42 025x PHARMACY (also see 063x, an extension of 025x) Charges for medication produced, manufactured, packed, controlled, assayed, dispensed and distributed under the direction of a licensed pharmacist. Sub-Category 0 General Classification 1 General Drugs 2 Non-Generic Drugs 3 Take Home Drugs 4 Drugs Incident to Other Diagnostic Services 5 Drugs Incident to Radiology 6 Experimental Drugs 7 Non-Prescription 8 IV Solutions 9 Other Pharmacy 026x Standard Abbreviation PHARMACY DRUGS/GENERIC DRUGS/NON-GENERIC DRUGS/TAKE HOME DRUGS/INCIDENT/DX Unit DRUGS/INCIDENT RAD DRUGS/EXPERIMT DRUGS/NONPSCRIPT IV SOLUTIONS DRUGS/OTHER HCPCS N Y-OP Y-OP Y-OP Y-OP Y-OP Y-OP Y-OP Y-OP Y-OP IV THERAPY Equipment charge or administration of intravenous solution by specially trained personnel to individuals requiring such treatment. Sub-Category 0 General Classification 1 Infusion Pump 2 IV Therapy/Pharmacy Services 3 IV Therapy/Drug/Supply Delivery 4 IV Therapy/Supplies 5-8 RESERVED 9 Other IV Therapy Standard Abbreviation Unit IV THERAPY IV THER/INFSN PUMP IV THER/PHARM/SVC IV THER/DRUG/SUPPLY/ DEL IV THER/SUPPLIES HCPCS Y-OP Y-OP Y-OP Y-OP Y-OP IV THERAPY/OTHER Y-OP Billing for Home IV providers, require the HCPCS code which describes the pump to be entered in FL 44. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 43 Form Locator 42 027x MEDICAL/SURGICAL SUPPLIES AND DEVICES (also see 062x, an extension of 027x) Charges for supply items required for patient care Sub-Category 0 General Classification 1 Non-Sterile Supply 2 Sterile Supply 3 Take Home Supplies 4 Prosthetic/Orthotic Devices 5 Pace Maker 6 Intraocular Lens 7 Oxygen - Take Home 8 Other Implants (a) 9 Other Supplies/Devices Standard Abbreviation MED-SUR SUPPLIES NON-STER SUPPLY STERILE SUPPLY TAKE HOME SUPPLY PROSTH/ORTH DEV PACE MAKER INTRA OC LENS 02/TAKE HOME SUPPLY/IMPLANTS SUPPLY/OTHER Unit HCPCS Devices Y (a) Implantables: That which is implanted, such as a piece of tissue, a tooth, a pellet of medicine, or a tube or needle containing a radioactive substance, a graft, or an insert. Also included are liquid and solid plastic materials used to augment tissues or to fill in areas traumatically or surgically removed. An object or material partially or totally inserted or grafted into the body for prosthetic, therapeutic, diagnostic purposes. Examples of Other Implants (not all9inclusive): Stents, artificial joints, shunts, grafts, pins, plates, screws, anchors, radioactive seeds. Experimental devices that are implantable and have been granted an FDA Investigational Device Exemption (IDE) number should be billed with revenue code 0624. 028x ONCOLOGY Charges for the treatment of tumors and related diseases Sub-Category 0 General Classification 1-8 RESERVED 9 Other Oncology 029x Standard Abbreviation ONCOLOGY Unit HCPCS ONCOLOGY/OTHER DURABLE MEDICAL EQUIPMENT (OTHER THAN RENAL) Charge for medical equipment that can withstand repeated use (excluding rental equipment) Sub-Category 0 General Classification 1 Rental 2 Purchase of New DME 3 Purchase of Used DME BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation DME DME-RENTAL DME-NEW DME-USED Unit HCPCS Y Y Y Page 44 4 Supplies/Drugs for DME 5-8 RESERVED 9 Other Equipment DME-SUPPLIES/DRUGS Y DME-OTHER Y Form Locator 42 030x LABORATORY Charges for the performance of diagnostic and routine clinical laboratory tests Sub-Category 0 General classification 1 Chemistry 2 Immunology 3 Renal Patient (Home) 4 Non-Routine Dialysis 5 Hematology 6 Bacteriology & Microbiology 7 Urology 8 RESERVED 9 Other Laboratory 031x Standard Abbreviation LAB CHEMISTRY TESTS IMMUNOLOGY TESTS RENAL HOME NON-RTNE DIALYSIS HEMATOLOGY TESTS BACT & MICRO TESTS UROLOGY TESTS Unit HCPCS Tests Tests Tests Tests Tests Tests Tests Y Y Y Y Y Y Y OTHER LAB TESTS Tests Y Standard Abbreviation PATHOLOGY LAB CYTOLOGY TESTS HISTOLOGY TESTS Unit Tests Tests Tests HCPCS Y Y Y BIOPSY TESTS Tests Y PATH LAB OTHER Tests Y LABORATORY PATHOLOGY Charges for diagnostic and routine laboratory tests on tissues and culture Sub-Category 0 General Classification 1 Cytology 2 Histology 3 RESERVED 4 Biopsy 5-8 RESERVED 9 Other Laboratory Pathology 032x RADIOLOGY - DIAGNOSTIC Charges for diagnostic radiology services including interpretation of radiographs and fluorographs Sub-Category 0 General Classification 1 Angiocardiology 2 Arthrography 3 Arteriography 4 Chest X-Ray 5-8 RESERVED 9 Other Radiology - Diagnostic BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation DX X-RAY DX X-RAY/ANGIO DX X-RAY/ARTHO DX X-RAY/ARTER DX X-RAY/CHEST Unit Tests Tests Tests Tests Tests HCPCS Y Y Y Y Y DX X-RAY/OTHER Tests Y Page 45 Form Locator 42 033x RADIOLOGY - THERAPEUTIC AND/OR CHEMOTHERAPY ADMINISTRATION Charges for therapeutic radiology services and chemotherapy administration to care and treat patients. Therapies also include injection and/or ingestion of radioactive substances. Excludes charges for chemotherapy drugs; report these under the appropriate revenue code (025x or 063x). Sub-Category 0 General Classification 1 Chemotherapy Administration - Injected 2 Chemotherapy Administration - Oral 3 Radiation Therapy 4 RESERVED 5 Chemotherapy Administration - IV 6-8 RESERVED 9 Other Radiology - Therapeutic Standard Abbreviation RADIOLOGY THERAPY RAD-CHEMO-INJECT RAD-CHEMOTHER-ORAL RAD-RADIATION Unit Tests Tests Tests Tests HCPCS Y Y Y Y RAD-CHEMOTHER-IV Tests Y RADIOLOGY OTHER Tests Y Usage note: When using 0331, 0332, or 0335 there must be use of Revenue Code 0636. 034x NUCLEAR MEDICINE Charges for procedures, tests, and radiopharmaceuticals performed by a department handling radioactive materials as required for diagnosis and treatment of patients. Sub-Category 0 General Classification 1 Diagnostic 2 Therapeutic 3 Diagnostic Radiopharmaceuticals 4 Therapeutic Radiopharmaceuticals 5-8 RESERVED 9 Other Nuclear Medicine Standard Abbreviation NUCLEAR MEDICINE NUC MED/DX NUC MED/RX NUC MED/DX RADIOPHARM NUC MED/RX RADIOPHARM Unit Tests Tests Tests Tests Tests HCPCS Y Y Y Y Y NUC MED/OTHER Tests Y Standard Abbreviation CT SCAN CT SCAN/HEAD CT SCAN/BODY Unit Tests Tests Tests HCPCS Y Y Y CT SCAN/OTHER Tests Y 035x CT SCAN Charges for computed tomographic scans of the head and other parts of the body Sub-Category 0 General Classification 1 CT - Head Scan 2 CT - Body Scan 3-8 RESERVED 9 CT- OTHER 036x OPERATING ROOM SERVICES Charges for services provided to patients by specifically trained nursing personnel who assist physicians in the performance of surgical and related procedures during and immediately following surgery. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 46 Sub-Category 0 General Classification 1 Minor Surgery 2 Organ Transplant Other than Kidney 3-6 RESERVED 7 Kidney Transplant 8 RESERVED 9 Other Operating Room Service Standard Abbreviation OR SERVICES OR/MINOR OR/ORGAN TRANS Unit HCPCS Y Y Y OR/KIDNEY TRANS Y OR/OTHER Y Form Locator 42 037x ANESTHESIA Charges for anesthesia services Sub-Category 0 General Classification 1 Anesthesia Incident to Radiology 2 Anesthesia Incident to Other Diagnostic Services 3 RESERVED 4 Acupuncture 5-8 RESERVED 9 Other Anesthesia Standard Abbreviation ANESTHESIA ANESTHE/INCIDENT RAD ANES/INCDNT OTHER DX Unit HCPCS Unit HCPCS Y Y Y Y Y Y Y Y ANESTHE/ACUPUNC ANESTHE/OTHER 038x BLOOD and BLOOD COMPONENTS Charges for blood and blood components Sub-Category 0 General Classification 1 Packed Red Cells 2 Whole Blood 3 Plasma 4 Platelets 5 Leukocytes 6 Other Components 7 Other Derivatives (Cryoprecipitate) 8 RESERVED 9 Other Blood Standard Abbreviation BLOOD & BLOOD COMP BLOOD/PKD RED BLOOD/WHOLE BLOOD/PLASMA BLOOD/PLATELETS BLOOD/LEUKOCYTES BLOOD/COMPONENTS BLOOD/DERIVATIVES Pints Pints Pints BLOOD/OTHER Y 039x ADMINISTRATION, PROCESSING, AND STORAGE FOR BLOOD AND BLOOD COMPONENTS Charges for administration, processing and storage of whole blood, red blood cells, platelets, and other blood components Sub-Category 0 General Classification 1 Administration (e.g., Transfusion) 2 Processing and Storage 3-8 RESERVED 9 Other Blood Handling Standard Abbreviation BLOOD/ADMIN/STOR BLOOD/ADMIN BLOOD/STORAGE BLOOD/ADMIN/STOR/OTHER Unit Pints Pints HCPCS Y Y Y Y 040x OTHER IMAGING SERVICES Charges for specialty imaging services for body structures BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 47 Sub-Category 0 General Classification 1 Diagnostic Mammography 2 Ultrasound 3 Screening Mammography 4 Position Emission Tomography 5-8 RESERVED 9 Other Imaging Services Standard Abbreviation IMAGE SERVICE DIAG MAMMOGRAPHY ULTRASOUND SCRN MAMMOGRAPHY PET SCAN OTHER IMAG SVS Unit Tests Tests Tests Tests Tests HCPCS Y Y Y Y Y Tests Y Form Locator 42 041x RESPIRATORY SERVICES Charges for respiratory services including administration of oxygen and certain potent drugs through inhalation or positive pressure and other forms of rehabilitative therapy. Sub-Category 0 General Classification 1 RESERVED 2 Inhalation Services 3 Hyperbaric Oxygen Therapy 4-8 RESERVED 9 Other Respiratory Services Standard Abbreviation RESPIRATORY SVC Unit HCPCS Treatment Y INHALATION SVC HYPERBARIC 02 Treatment Treatment Y Y OTHER RESPIR SVS Treatment Y 042x PHYSICAL THERAPY Charges for therapeutic exercises, massage and utilization of Effective Date properties of light, heat, cold, water, electricity and assist devices for diagnosis and rehabilitation of patients who have neuromuscular, orthopedic and other disabilities. Sub-Category 0 General Classification 1 Visit 2 Hourly 3 Group 4 Evaluation or Re-Evaluation 5-8 RESERVED 9 Other Physical Therapy Standard Abbreviation PHYSICAL THERP PHYS THERP/VISIT PHYS THERP/HOUR PHYS THERP/GROUP PHYS THERP/EVAL Unit HCPCS HCPCS Y HCPCS Y HCPCS Y HCPCS Y HCPCS Y OTHER PHYS THERP HCPCS Y 043x OCCUPATIONAL THERAPY Charges for therapeutic interventions to improve, sustain or restore an individual’s level of function in performance, of activities of daily living and work, including: therapeutic activities; therapeutic exercise; sensorimotor processing; psychosocial skills training; cognitive retraining; fabrication and application of orthotic devices; and training in the use of orthotic and prosthetic devices; adaptation of environments; and application of physical agent modalities. Sub-Category 0 General Classification 1 Visit 2 Hourly 3 Group 4 Evaluation or Re-Evaluation 5-8 RESERVED 9 Other Occupational Therapy Standard Abbreviation OCCUPATIONAL THER OCCUP THERP/VISIT OCCUP THERP/HOUR OCCUP THERP/GROUP OCCUP THERP/EVAL Unit HCPCS HCPCS Y HCPCS Y HCPCS Y HCPCS Y HCPCS Y OTHER OCCUP THER HCPCS Y Services are provided by a qualified occupational therapist. 044x SPEECH therapy - LANGUAGE PATHOLOGY Charges for services related to impaired functional communications skills. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 48 Standard Abbreviation Sub-Category 0 General Classification SPEECH THERAPY 1 Visit SPEECH THERP/VISIT 2 Hourly SPEECH THERP/HOUR 3 Group SPEECH THERP/GROUP 4 Evaluation or Re-Evaluation SPEECH THERP/EVAL 5-8 RESERVED 9 Other Speech Therapy OTHER SPEECH THERP Services are provided by a qualified speech therapist. Unit HCPCS HCPCS Y HCPCS Y HCPCS Y HCPCS Y HCPCS Y HCPCS Y Form Locator 42 045x EMERGENCY ROOM Charges for emergency treatment to those ill and injured persons who require immediate unscheduled medical or surgical care. Sub-Category 0 General Classification 1 EMTALA Emergency Medical Screening 2 ER Beyond EMTALA 3-5 RESERVED 6 Urgent Care 7-8 RESERVED 9 Other Emergency Room Standard Abbreviation EMERG ROOM ER/EMTALA ER/BEYOND EMTALA Unit Visit Visit Visit HCPCS Y Y Y URGENT CARE Visit Y OTHER EMER ROOM Visit Y Usage Notes: Report Patient’s Reason for Visit code in FL 70 in conjunction with this revenue code. (a) General classification code 0450 should not be used in conjunction with any subcategory. The sum of 0451 and 0452 is equivalent to 0450. (b) Stand-alone usage of 0451 is acceptable when no services beyond an initial screening/assessment are rendered. (c) Stand-alone usage of 0452 is not acceptable. 046x PULMONARY FUNCTION Charges for tests that measure inhaled and exhaled gases and analysis of blood for tests that evaluate the patient’s ability to exchange oxygen and other gases. Sub-Category 0 General Classification 1-8 RESERVED 9 Other Pulmonary Function Standard Abbreviation PULMONARY FUNC Unit Test HCPCS Y OTHER PULMON FUNC Test Y 047x AUDIOLOGY Charges for the detection and management of communication handicaps centering in whole or in part on the hearing function Sub-Category 0 General Classification 1 Diagnostic 2 Treatment 3-8 RESERVED 9 Other Audiology BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation AUDIOLOGY AUDIOLOGY/DX AUDIOLOGY/RX Unit Test Test Test HCPCS Y Y Y OTHER AUDIOL Test Y Page 49 Services are provided by or through the supervision of a qualified audiologist. Form Locator 42 048x CARDIOLOGY Charges for cardiac procedures. Sub-Category 0 General Classification 1 Cardiac CATH LAB 2 Stress Test 3 Echocardiology 4-8 RESERVED 9 Other Cardiology Standard Abbreviation CARDIOLOGY CARDIAC CATH LAB STRESS TEST ECHOCARDIOLOGY Unit Test Test Test Test HCPCS Y Y Y Y OTHER CARDIOL Test Y Services provided are by staff from the cardiology department of the hospital or under arrangement. Services include such procedures such as: heart catheterization, coronary angiography, Swan-Ganz catheterization, and exercise stress test. 049x AMBULATORY SURGICAL CARE Charges for ambulatory surgery not covered by other categories. Sub-Category 0 General Classification 1-8 RESERVED 9 Other Ambulatory Surgical Care Standard Abbreviation AMBULTRY SURG Unit HCPCS HCPCS Y OTHER AMBL SURG HCPCS Y 050x OUTPATIENT SERVICES Charges for services rendered to an outpatient who is then admitted as an inpatient before midnight of the day following the date of service. Sub-Category 0 General Classification 1-8 RESERVED 9 Other Outpatient 051x Standard Abbreviation OUTPATIENT SVCS Unit Test HCPCS Y OTHER – O/P SERVICES Test Y CLINIC Clinic visit charges for providing diagnostic, preventative, curative, rehabilitative and education services to ambulatory patients. Sub-Category 0 General Classification 1 Chronic Pain Center 2 Dental Clinic BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation CLINIC CHRONIC PAIN CLINIC DENTAL CLINIC Unit Visit Visit Visit HCPCS Y Y Y Page 50 3 4 5 6 7 8 9 Psychiatric Clinic OB-GYN Clinic Pediatric Clinic Urgent Care Clinic* Family Practice Clinic RESERVED Other Clinic PSYCHIATRIC CLINIC OB-GYN CLINIC PEDIATRIC CLINIC URGENT CARE CLINIC FAMILY CLINIC Visit Visit Visit Visit Visit Y Y Y Y Y OTHER CLINIC Visit Y * Report the Patient’s Reason for Visit diagnosis codes for all Urgent Care Clinic visits. Form Locator 42 052x FREE-STANDING CLINIC Charges for the outpatient visit at a freestanding clinic. Sub-Category 0 General Classification 1 Clinic Visit by Member to RHC/FQHC 2 Home Visit by RHC/FQHC Practitioner 3 Family Practice Clinic 4 Visit by RHC/FQHC Practitioner to a Member in a Covered Part A Stay at SNF 5 Visit by RHC/FQHC Practitioner to a Member In a SNF (not in a Covered Part A Stay) or NF or ICF MR or Other Residential Facility 6 Urgent Care Clinic* 7 Visiting Nurse Service(s) to a Member’s Home when in a Home Health Shortage Area 8 Visit by RHC/FQHC Practitioner to Other Non-RHC/FQHC Site (e.g. Scene of Accident) 9 Other Free-Standing Clinic Standard Abbreviation FREESTAND CLINIC FS-RURAL/CLINIC FS-RURAL/HOME FS-FAMILY PRACT FR/STD FAMILY CLINIC Unit Visit Visit Visit Visit HCPCS Y Y Y Y FR/STD URGENT CLINIC RHC/FQHC/HOME/VIS NURSE RHC/FQHC/OTHER SITE Visit Y OTHER FS-CLINIC Visit Y RHC/FWHC/SNF/ NONCOVERED * Report the Patient’s Reason for Visit diagnosis codes for all Urgent Care Clinic visits. 053x OSTEOPATHIC SERVICES Charges for a structural evaluation of the cranium, entire cervical, dorsal and lumbar spine by a doctor of osteopathy. Sub-Category 0 General Classification 1 Osteopathic Therapy 2-8 RESERVED 9 Other Osteopathic Services Standard Abbreviation OSTEOPATH SVS OSTEOPATH RX Unit Visit Visit HCPCS Y Y OTHER OSTEOPATH Visit Y Generally, these services are unique to osteopathic hospitals and cannot be accommodated in any of the existing revenue codes. 054x AMBULANCE Charges for ambulance services necessary for the transport of the ill or injured who require medical attention at a health care facility Sub-Category 0 General Classification BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation AMBULANCE Unit Mile HCPCS Y Page 51 1 2 3 4 5 6 7 8 9 Supplies Medical Transport Heart Mobile Oxygen Air Ambulance Neonatal Ambulance Services Pharmacy EKG Transmission Other Ambulance BCNEPA/FPH/FPLIC Billing Manual November 2012 AMBUL/SUPPLY AMBUL/MED TRANS AMBUL/HEARTMOB AMBUL/OXYGEN AIR AMBULANCE AMBUL/NEONAT AMBUL/PHARMACY AMBUL/EKG TRANS OTHER AMBULANCE Item Mile Mile Unit Mile Mile Unit Unit Mile N Y Y Y Y Y Y Y Y Page 52 Form Locator 42 055x SKILLED NURSING Charges for nursing services that must be provided under the direct supervision of a licensed nurse to assure the safety of the patient and to achieve the medically desired result. This code may be used for nursing home services, CORFS, or a service charge for home health billing. Sub-Category 0 General Classification 1 Visit Charge 2 Hourly Charge 3-8 RESERVED 9 Other Skilled Nursing Standard Abbreviation SKILLED NURSING-HH SKILLED NURS-VISIT SKILLED NURS-HOUR Unit Visit Hour SKILLED NURS/OTHER HCPCS Y Y Y Y 056x HOME HEALTH (HH) - MEDICAL SOCIAL SERVICES Home Health (HH) charges for services such as counseling patients, interviewing patients and interpreting problems of social situation rendered to patients on any basis. Sub-Category 0 General Classification 1 Visit Charge 2 Hourly Charge 3-8 RESERVED 9 Other Medical Social Services Standard Abbreviation MED SOCIAL-HH MED SOC SERV-VISIT MED SOC SERV-HOUR Unit Visit Hour MED SOC SERV-OTHER HCPCS Y Y Y Y 057x HOME HEALTH (HH) AIDE Home Health (HH) charges for personnel (aides) that are primarily responsible for the personal care of the patient. Sub-Category 0 General Classification 1 Visit Charge 2 Hourly Charge 9 Other Home Health Aide Standard Abbreviation HH AIDE HH AIDE-VISIT HH AIDE-HOUR HH AIDE-OTHER Unit Visit Hour HCPCS Y Y Y Y 058x HOME HEALTH (HH) - OTHER VISITS Home Health agency charges for visits other than physical therapy, occupational therapy or speech therapy, requiring specific identification. Sub-Category 0 General Classification 1 Visit Charge 2 Hourly Charge 3 Assessment 4-8 RESERVED 9 Other Home Health Visit BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation HH-OTH VIS HH-OTH VIS/VISIT HH-OTH VIS/HOUR HH-OTH VIS/ASSESS Unit Visit Hour Visit HCPCS Y Y Y Y HH-OTH VIS/OTHER Visit Y Page 53 Form Locator 42 059x HOME HEALTH (HH) UNITS OF SERVICE Home Health (HH) charges for services billed according to the units of service provided. Sub-Category 0 General Classification 1-9 RESERVED Standard Abbreviation HH-SVCS/UNIT Unit Unit HCPCS Y 060x HOME HEALTH (HH) - OXYGEN Home Health agency charges for oxygen equipment, supplies or contents, excluding purchased equipment. If patient purchases a stationary oxygen system, an oxygen concentrator or portable equipment, current revenue codes 0292 or 0293 apply. DME (other than oxygen systems) is billed under revenue codes 0291, 0292, or 0293. Sub-Category 0 General Classification 1 Oxygen - Stat Equip/Supply/Content 2 Oxygen - Stat Equip/Supply<1 LPM 3 Oxygen - Stat Equip/Supply>4 LPM 4 Oxygen - Portable Add-on 5-8 RESERVED 9 Oxygen - Other Standard Abbreviation 02/HOME HEALTH 02/STAT/EQP/SUP/CONT 02/STAT/EQP/SUP< 1 LPM 02/STAT/EQP/SUP> 4 LPM 02/PORTABLE ADD-ON Unit HCPCS Y Ft/Lbs Y Mos Y Mos Y Mos Y 02/OTHER Y 061x MAGNETIC RESONANCE TECHNOLOGY (MRT) Charges for Magnetic Resonance Imaging (MRI) and Magnetic Resonance Angiography. Sub-Category Standard Abbreviation 0 General Classification MRT 1 MRI - Brain/Brainstem MRI/BRAIN 2 MRI - Spinal Cord/Spine MRI/SPINE 3 RESERVED 4 MRI - Other MRI/OTHER 5 MRA - Head and Neck MRA/HEAD AND NECK 6 MRA - Lower Extremities MRA/LOWER EXTRM 7 RESERVED 8 MRA - Other MRA/OTHER 9 Other MRT MRT/OTHER Note: If revenue code 619 is used, enter the type of MRI into the remarks field. Unit Tests Tests Tests HCPCS Y Y Y Tests Tests Tests Y Y Y Tests Tests Y Y 062x MEDICAL SURGICAL SUPPLIES - Extension of 027x Charges for supply items required for patient care. The category is an extension of 027x for reporting additional breakdown where needed. Subcategory code 1 is for providers that cannot bill supplies used for radiology procedures under radiology. Subcategory code 2 is for providers that cannot bill supplies used for other diagnostic procedures. Sub-Category 0 RESERVED (Use 0270 for General Classification) 1 Supplies Incident to Radiology 2 Supplies Incident to Other DX Services 3 Surgical Dressings 4 FDA Investigational Devices 5-9 RESERVED BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation Unit HCPCS MED SUR SUPL-INCDT RAD MED SUR SUPL-INCDT ODX SURG DRESSING FDA INVEST DEVICE HCPCS HCPCS HCPCS HCPCS Y Y Y Y Page 54 Form Locator 42 063x PHARMACY - Extension of 025x Charges for medication produced, manufactured, packaged, controlled, assayed, dispensed and distributed under the direction of a licensed pharmacist. The category is an extension of 025X for reporting additional breakdown where needed. Sub-Category 0 RESERVED (Use 0250 for General Classification) 1 Single Source Drug 2 Multiple Source Drug 3 Restrictive Prescription 4 Erythropoietin (EPO) <10,000 Units 5 Erythropoietin (EPO)>=10,000 Units 6 Drugs Requiring Detail Coding (a) 7 Self-Administrable Drugs (b) Standard Abbreviation Unit HCPCS DRUG/SINGLE DRUG/MULTIPLE DRUG/RESTRICT DRUG/EPO<10,000 Units DRUG/EPO>=10,000 Units DRUG/DETAIL CODE DRUG/SELF ADMIN HCPCS HCPCS HCPCS HCPCS HCPCS HCPCS HCPCS Y Y Y Y Y Y Y (a) Charges for drugs and biologicals (with the exception of radiopharmaceuticals, which are reported under Revenue Codes 0343 and 0344) requiring specific identification as required by the payer. If using a HCPCS to describe the drug, enter the HCPCS code in the appropriate HCPCS column. The specific service units reported should be in hundreds (100s), rounded to the nearest hundred; do not use a decimal. (b) Charges for self-administrable drugs not requiring detailed coding. Use Value Codes A4, A5, and A6 to indicate the dollar amount included in covered charges for self-administrable drugs. Amounts for non-covered self-administrable drugs should be charged using Revenue Code 0637 in the noncovered column. 064x HOME IV THERAPY SERVICES Charge for intravenous therapy services performed in the patient’s residence. For Home IV providers enter the HCPCS code for all equipment, and all types of covered therapy. Sub-Category 0 General Classification 1 Non-routine Nursing, Central Line 2 IV Site Care, Central Line (see note) 3 IV Start/Change, Peripheral Line 4 Non-routine Nursing, Peripheral Line 5 Training Patient/Care Giver, Central Line 6 Training, Disabled Patient, Central Line 7 Training, Patient/Care Giver, Peripheral Line 8 Training, Disabled Patient, Peripheral Line 9 Other IV Therapy Services Standard Abbreviation Unit IV THERAPY SVC NON RT NURSING/CENTRAL IV SITE CARE/CENTRAL IV STRT CARE/PERIPHRL NONRT NURSING/PERIPHRL TRNG PT/CAREGVR/CNTRL Hour TRNG DSBLPT/CENTRAL Hour TRNG/PT/CARGVR/PERIPHRL Hour TRNG/DSBLPT/PERIPHRL Hour OTHER IV THERAPY SVC HCPCS Y Y Y Y Y Y Y Y Y Y Note: Report units in one hour increments; Revenue code 0642 relates to the HCPCS code. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 55 Form Locator 42 065x HOSPICE SERVICES Charge for hospice care services for a terminally ill patient electing hospice services in lieu of other medical services for the terminal condition. Sub-Category Standard Abbreviation 0 General Classification HOSPICE 1 Routine Home Care HOSPICE/RTN HOME 2 Continuous Home Care HOSPICE/CTNS HOME 3-4 RESERVED 5 Inpatient Respite Care HOSPICE/IP RESPITE Days 6 General Inpatient Care Non-Respite HOSPICE/IP NON-RESPITE 7 Physician Services HOSPICE/PHYSICIAN 8 Hospice Room & Board - Nursing Facility HOSPICE/R&B NURS FAC 9 Other Hospice Service HOSPICE/OTHER Unit HCPCS Y Hours Y Hours Y Y Days Y HCPCS Y Days Y Y Note: To receive the continuous home car rate from Medicare use code 0652, a minimum of 8 hours of care, not necessarily consecutive, must be accompanied by a physician procedure code. Enter this information in the HCPCS column (Form Locator 44). This code is used by the hospice to bill for charges for physicians employed by the hospice or receiving compensation from the hospice for services rendered. The unit will be either days or hours depending on subcategory and billing contracts. 066x RESPITE CARE Charges for non-hospice respite care. Sub-Category 0 General Classification 1 Hourly Charge - Nursing 2 Hourly Charge/Aide/Homemaker/ Companion 3 Daily Respite Charge 4-8 RESERVED 9 Other Respite Care Standard Abbreviation RESPITE CARE RESPITE/NURSING RESPITE/AIDE/HMEMKR/ COMP RESPITE/DAILY Unit Hours Hours RESPITE/OTHER Hours HCPCS Day 067x OUTPATIENT SPECIAL RESIDENCE CHARGES Residence arrangements for patients requiring continuous outpatient care. Sub-Category 0 General Classification 1 Hospital Owned 2 Contracted 3-8 RESERVED 9 Other Special Residence Charge BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation OP SPEC RES OP SPEC RES/HOSP OWNED OP SPEC Unit Day OP SPEC RES/OTHER Day HCPCS Day Page 56 Form Locator 42 068x TRAUMA RESPONSE Charges representing the activation of the trauma team Sub-Category 0 Not Used 1 Level I Trauma 2 Level II Trauma 3 Level III Trauma 4 Level IV Trauma 5-8 RESERVED 9 Other Trauma Response Standard Abbreviation Unit HCPBS TRAUMA LEVEL I TRAUMA LEVEL II TRAUMA LEVEL III TRAUMA LEVEL IV Activation Activation Activation Activation TRAUMA OTHER Activation Usage Notes: 1. For use by trauma center/hospitals, licensed or designated by the state or local government authority authorized as a trauma center, or verified by the American College of Surgeons and as a facility with a trauma activation team. 2. Revenue Category 068x is used for patients for whom a trauma activation occurred. A trauma team activation/response is a “Notification of key hospital personnel in response to triage information from pre-hospital caregivers in advance of the patient’s arrival.” 3. Revenue Category 068x is for reporting trauma activation costs only. It is an activation fee and not a replacement or a substitute for the emergency room visit fee; if trauma activation occurs, there will normally be both a 045x and 068x revenue code reported. 4. Revenue Category 068x is not limited to admitted patients. 5. Revenue Category 068x must be used in conjunction with FL14 Priority (Type) of Admission/Visit Code 5 (“Trauma Center”), however FL 14 Code 5 can be used alone for trauma activations that lack pre-hospital notification. Only patients for whom there has been pre-hospital notification, who meet either local, state or American College of Surgeons field triage criteria, or are delivered by inter-hospital transfers, and are given the appropriate team response, can be billed the trauma activation fee charge. Patients who are “drive-by” or arrive without notification cannot be charged for activations, but can be classified as trauma under Type of Admission Code 5 for statistical and follow-up purposes. 6. Levels I, II, III, or IV refer to designations given to the trauma facility by the state or local government authority or as verified by the American College of Surgeons. 7. Subcategory 9 is for states or local authorities with levels beyond IV. 069x RESERVED 070x CAST ROOM Charge for services related to the application, maintenance and removal of casts. Sub-Category 0 General Classification 1-9 RESERVED BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation CAST ROOM Unit HCPCS Page 57 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 58 Form Locator 42 071x RECOVERY ROOM Room charge for patient recovery after surgery. Sub-Category 0 General Classification 1-9 RESERVED Standard Abbreviation RECOVERY ROOM Unit HCPCS N 072x LABOR ROOM/DELIVERY Charges for labor and delivery room services provided by specifically trained nursing personnel to patients, including prenatal care during labor, assistance during delivery, postnatal care in the recovery room and minor gynecologic procedures if they are performed in the delivery suite. Sub-Category 0 General Classification 1 Labor 2 Delivery Room 3 Circumcision 4 Birthing Center 4-8 RESERVED 9 Other Labor Room/Delivery Standard Abbreviation DELIVERY ROOM/LABOR LABOR DELIVERY ROOM CIRCUMCISION BIRTHING CENTER Unit HCPCS Days Days Each Days OTHER/DELIV/LABOR 073x EKG/ECG (ELECTROCARDIOGRAM) Charges for operation of specialized equipment to record variations in actions of the heart muscle for diagnosis of heart ailments. Sub-Category 0 General Classification 1 Holter Monitor 2 Telemetry 3-8 RESERVED 9 Other EKG/ECG Standard Abbreviation EKG/ECG HOLTER MONT TELEMETRY Unit Tests Tests Tests HCPCS Y Y Y OTHER EKG/ECG Tests Y 074x EEG (ELECTROENCEPHALOGRAM) Charges for operation of specialized equipment to measure impulse frequencies and differences in electrical potential in various areas of the brain to obtain data for use in diagnosing brain disorders. Sub-Category 0 General Classification 1-9 RESERVED Standard Abbreviation EEG Unit Tests HCPCS Y Unit Tests HCPCS Y 075x GASTRO - INTESTINAL (GI) SERVICES Charges for GI procedures not performed in the operating room. Sub-Category 0 General Classification 1-9 RESERVED BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation GASTRO-INTSTL SVS Page 59 Form Locator 42 076x SPECIALTY SERVICES Charges for patients requiring treatment room services or patients placed under observation. Sub-Category 0 General Classification 1 Treatment Room 2 Observation Hours (a) 3-8 RESERVED 9 Other Specialty Services Standard Abbreviation SPECIALTY SVC TREATMENT ROOM OBSERVATION Unit HCPCS Y OTHER SPECIALTY SVC Note: Observation services are those services furnished by a hospital on the hospital’s premises, including use of a bed and periodic monitoring by a hospital’s nursing or other staff, which are reasonable and necessary to evaluate an outpatient’s condition or determine the need for a possible admission to the hospital or as an inpatient. Such services are covered only when provided by the order of a physician or another individual authorized by State licensure law and hospital staff bylaws to admit patients to the hospital or to order outpatient tests. The reason for observation must be stated in the orders for observation. Payers should establish written guidelines, which identify coverage of observation services. (a) FL 70a-c – Patient’s Reason for Visit should be reported in conjunction with 0762. 077x PREVENTIVE CARE SERVICES Revenue Code used to capture preventive care services established by payers (e.g., vaccination). Sub-Category 0 General Classification 1 Vaccine Administration 2-9 RESERVED Standard Abbreviation PREVENT CARE SVCS VACCINE ADMIN Unit HCPCS Y Y Unit HCPCS Unit HCPCS Y 078x TELEMEDICINE Facility charges related to the use of telemedicine services Sub-Category 0 General Classification 1-9 RESERVED Standard Abbreviation TELEMEDICINE 079x EXTRA-CORPOREAL SHOCK WAVE THERAPY (Formerly Lithotripsy) Charges related to Extra-Corporeal Shock Wave Therapy (ESWT). Sub-Category 0 General Classification 1-9 RESERVED BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation ESWT Page 60 Form Locator 42 080x INPATIENT RENAL DIALYSIS Charges for the use of equipment designed to remove waste when the body’s own kidneys have failed. The waste may be removed directly from the blood (hemodialysis) or indirectly from the blood by flushing a special solution between the abdominal covering and the tissue (peritoneal dialysis). Sub-Category 0 General Classification 1 Inpatient Hemodialysis 2 Inpatient Peritoneal (Non-CAPD) 3 Inpatient Continuous Ambulatory Peritoneal Dialysis (CAPD) 4 Inpatient Continuous Cycling Peritoneal Dialysis (CCPD) 5-8 RESERVED 9 Other Inpatient Dialysis Standard Abbreviation RENAL DIALYSIS DIALY/INPATIENT DIALY/INPT/PER DIALY/IP/CAPD Unit HCPCS Sessions Sessions Sessions Sessions DIALY/INPT/CCPD Sessions DIALY/INPT/OTHER Sessions 081x ACQUISITION OF BODY COMPONENTS The acquisition and storage costs of body tissue, bone marrow, organs and other body components not otherwise identified used for transplantation. Sub-Category 0 General Classification 1 Living Donor 2 Cadaver Donor 3 Unknown Donor 4 Unsuccessful Organ Search - Donor Bank Charges 5-8 RESERVED 9 Other Donor Standard Abbreviation ORGAN ACQUISIT LIVING DONOR CADAVER DONOR UNKNOWN DONOR UNSUCCESSFUL SEARCH Unit OTHER DONOR HCPCS Y Y Y Y Y Y Notes: Living donor is a living person from whom an organ is collected and used for transplantation purposes. Cadaver is an individual pronounce dead according to medical and legal criteria, and whose organs may be harvested for transplantation. Unknown is used whenever the status of the individual source cannot be determined. Use the other category whenever the organ is non-human. Revenue Code 0814 is used only when costs incurred for an organ search do not result in an eventual organ acquisition and transplantation. 082x HEMODIALYSIS - OUTPATIENT OR HOME A waste removal process, performed in an outpatient or home setting, necessary when the body’s own kidneys have failed. Waste is removed directly from the blood. Sub-Category 0 General Classification 1 Hemodialysis/Composite or Other Rate 2 Home Supplies 3 Home Equipment 4 Maintenance - 100% 5 Support Services 6-8 RESERVED 9 Other Outpatient Hemodialysis BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation HEMO/OP or HOME HEMO/COMPOSITE HEMO/HOME/SUPPL HEMO/HOME/EQUIP HEMO/HOME/100% HEMO/HOME/SUPSERV Unit HCPCS Y Sessions Y Sessions Y Sessions Y Sessions Y Sessions Y HEMO/OTHER/OP Sessions Y Page 61 Form Locator 42 083x PERITONEAL DIALYSIS - OUTPATIENT OR HOME Charges for a waste removal process performed in an outpatient or home setting, necessary when the body’s own kidneys have failed. Waste is removed indirectly by flushing a special solution between the abdominal covering and the tissue. Sub-Category 0 General Classification 1 Peritoneal/Composite or Other Rate 2 Home Supplies 3 Home Equipment 4 Maintenance - 100% 5 Support Services 6-8 RESERVED 9 Other Outpatient Peritoneal Dialysis Standard Abbreviation PERITONEAL/OP or HOME PERTNL/COMPOSITE PERTNL/HOME/SUPPL PERTNL/HOME/EQUIP PERTNL/HOME/100% PERTNL/HOME/SUPSERV Unit HCPCS Sessions Y Sessions Y Sessions Y Sessions Y Sessions Y Sessions Y PERTNL/HOME/OTHER Sessions Y 084x CONTINUOUS AMBULATORY PERITONEAL DIALYSIS (CAPD) - OUTPATIENT OR HOME Charges for continuous dialysis process performed in an outpatient or home setting which uses the patient’s peritoneal membrane as a dialyzer. Sub-Category 0 General Classification 1 CAPD/Composite or Other Rate 2 Home Supplies 3 Home Equipment 4 Maintenance - 100% 5 Support Services 6-8 RESERVED 9 Other Outpatient CAPD Standard Abbreviation CAPD/OP or HOME CAPD/COMPOSITE CAPD/HOME/SUPPL CAPD/HOME/EQUIP CAPD/HOME/100% CAPD/HOME/SUPSERV Unit Days Days Days Days Days Days HCPCS Y Y Y Y Y Y CAPD/HOME/OTHER Days Y 085x CONTINUOUS CYCLING PERITONEAL DIALYSIS (CCPD) - OUTPATIENT OR HOME Charges for continuous dialysis process performed in an outpatient or home setting which uses a machine to make automatic exchanges at night. Sub-Category 0 General Classification 1 CCPD/Composite or Other Rate 2 Home Supplies 3 Home Equipment 4 Maintenance - 100% 5 Support Services 6-8 RESERVED 9 Other Outpatient CCPD Standard Abbreviation CCPD/OP or HOME CCPD/COMPOSITE CCPD/HOME/SUPPL CCPD/HOME/EQUIP CCPD/HOME/100% CCPD/HOME/SUPSERV Unit Days Days Days Days Days Days HCPCS Y Y Y Y Y Y CCPD/HOME/OTHER Days Y Unit Test Test HCPCS Y Y 086x Magnetoencephalography (MEG) Effective 04/01/10 Sub-Category 0 General Classification 1 MEG 2-9 RESERVED Standard Abbreviation 087x RESERVED BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 62 Form Locator 42 088x MISCELLANEOUS DIALYSIS Charges for dialysis services not identified elsewhere. Sub-Category 0 General Classification 1 Ultrafiltration 2 Home Dialysis Aid Visit 3-8 RESERVED 9 Other Miscellaneous Dialysis Standard Abbreviation DIALY/MISC DIALY/ULTRAFILT HOME DIALYSIS AID VISIT Unit HCPCS Sessions Y Sessions Y Sessions Y DIALY/MISC/OTHER Sessions Y Note: Ultrafiltration is the process of removing excess fluid from the blood of dialysis patients by using a dialysis machine but without the dialysate solution. The designation is only used when the procedure is not performed as part of a normal dialysis session. 089x RESERVED 090x BEHAVORIAL HEALTH TREATMENT/SERVICES (also see 091x, an extension of 090x) Charges for prevention, intervention, and treatment services in the areas of mental health, substance abuse, developmental disabilities, and sexuality. Behavioral Health Care services are individualized, holistic, and culturally competent and may include on-going care and support and non-traditional services. Sub-Category 0 General Classification 1 Electroshock Treatment 2 Milieu Therapy 3 Play Therapy 4 Activity Therapy 5 Intensive Outpatient Services - Psychiatric 6 Intensive Outpatient Services - Chemical Dependency 7 Community Behavioral Health Program (Day Treatment) 8-9 RESERVED Standard Abbreviation BH/TREATMENTS BH/ELECTRO SHOCK BH/MILIEU THERAPY BH/PLAY THERAPY BH/ACTIVITY THERAPY BH/INTENS OP/PSYCH BH/INTENS OP/CHEM DEP Unit Visit Visit Visit Visit Visit Visit Visit HCPCS Y Y Y Y Y Y Y BH/COMMUNITY Visit Y Unit HCPCS Visit Visit Visit Visit Visit Visit Visit Visit Visit Y Y Y Y Y Y Y Y Y 091x BEHAVIORAL HEALTH TREATMENTS/SERVICES - Extension of 090x See Revenue Code 090x Standard Abbreviation Sub-Category 0 RESERVED (use 090 for General Classification) 1 Rehabilitation BH//REHAB 2 Partial Hospitalization - Less Intensive BH/PARTIAL HOSP 3 Partial Hospitalization - Intensive BH/PARTIAL INTENSV 4 Individual Therapy BH/INDIV RX 5 Group Therapy BH/GROUP RX 6 Family therapy BH/FAMILY RX 7 Bio Feedback BH/BIOFEED 8 Testing BH/TESTING 9 Other Behavioral Health Treatments BH/OTHER BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 63 Form Locator 42 092x OTHER DIAGNOSTIC SERVICES Charges for various diagnostic services specific to common screenings for disease, illness or medical condition. Sub-Category 0 General Classification 1 Peripheral Vascular Lab 2 Electomyelgram 3 Pap Smear 4 Allergy Test 5 Pregnancy Test 6-8 RESERVED 9 Other Diagnostic Service Standard Abbreviation OTHER DX SVCS PERI VASCUL LAB EMG PAP SMEAR ALLERGY TEST PREG TEST Unit HCPCS Tests Tests Tests Tests Tests Y Y Y Y Y OTHER DX SVCS Tests Y 093x MEDICAL REHABILITATION DAY PROGRAM Medical rehabilitation services as contracted with a payer and/or certified by the state. Services may include physical therapy, occupational therapy and speech therapy. Sub-Category 0 RESERVED 1 Half Day 2 Full Day 3-9 RESERVED Standard Abbreviation Unit HALF DAY FULL DAY Hours Hours HCPCS Note: The subcategories of 093x are designed as zero-bill revenue code (i.e., no dollars are reported in the Total Charge column (FL 47) for this revenue code) it should be used as a vehicle to supply program information as defined in the provider/payer contract. Therefore, zero would be reported in the Total Charge column and the number of hours provided would be reported in the Units field. The specific rehabilitation services would be reported under the applicable therapy revenue codes as normal. 094x OTHER THERAPEUTIC SERVICES (also see 095x, and extension of 094x) Charges for other therapeutic services not otherwise categorized. Sub-Category 0 General Classification 1 Recreational Therapy 2 Education/Training 3 Cardiac Rehabilitation 4 Drug Rehabilitation 5 Alcohol Rehabilitation 6 Complex Medical Equipment Routine 7 Complex Medical Equipment Ancillary 8 Pulmonary Rehabilitation 9 Other Therapeutic Service Standard Abbreviation OTHER RX SVCS RECREATION RX EDUC/TRAINING CARDIAC REHAB DRUG REHAB ALCOHOL REHAB CMPLX MED EQUIP/ROUT CMPLX MED EQUIP/ANC PULMONARY REHAB ADDITIONAL RX SVCS 095x OTHER THERAPEUTIC SERVICES (Extension of 094x) See Revenue Code 094x Standard Abbreviation Sub-Category 0 RESERVED (use 0940 for General Classification) 1 Athletic Training ATHLETIC TRAINING 2 Kinesiotherapy KINESIOTHERAPY 3-9 RESERVED BCNEPA/FPH/FPLIC Billing Manual November 2012 Unit HCPCS Visit Visit Visit Visit Visit Visit Visit Visit Visit Y Y Y Y Y Y Y Y Y Unit HCPCS Visit Visit Y Y Page 64 Form Locator 42 096x PROFESSIONAL FEES (also see 097x and 098x) Charges for medical professionals that the institutional health care provider along with the third party payer require the professional fee component to be billed on the UB. The professional fee component is separately identified by this revenue code. Generally used by Critical Access Hospitals (CAH) that bill both the technical and professional service components on the UB. Sub-Category 0 General Classification 1 Psychiatric 2 Ophthalmology 3 Anesthesiologist (MD) 4 Anesthetist (CRNA) 5-8 RESERVED 9 Other Professional Fee Standard Abbreviation PRO FEE PRO FEE/PSYCH PRO FEE/EYE PRO FEE/ANES MD PRO FEE/ANES CRNA Unit HCPCS Y Y Y Y PRO FEE/OTHER Y 097x PROFESSIONAL FEES (Extension of 096x) See Revenue Code 096x. Standard Abbreviation Sub-Category 0 RESERVED (use 0960 for General Classification) 1 Laboratory PRO FEE/LAB 2 Radiology - Diagnostic PRO FEE/RAD/DX 3 Radiology - Therapeutic PRO FEE/RAD/RX 4 Radiology - Nuclear Medicine PRO FEE/NUC MED 5 Operating Room PRO FEE/OR 6 Respiratory Therapy PRO FEE/RESPIR 7 Physical Therapy PRO FEE/PHYSI 8 Occupational Therapy PRO FEE/OCCUPA 9 Speech Pathology PRO FEE/SPEECH Unit HCPCS Y Y Y Y Y Y Y Y Y 098x PROFESSIONAL FEES (Extension of 096x and 097x) Charges for medical professionals that the institutional health care provider along with the third-party payer require the professional fee component to be billed on the UB. The professional fee component is separately identified by this revenue code. Generally used by Critical Access Hospitals (CAH). Sub-Category 0 RESERVED (use 0960 for General Category) 1 Emergency Room 2 Outpatient Services 3 Clinic 4 Medical Social Services 5 EKG 6 EEG 7 Hospital Visit 8 Consultation 9 Private Duty Nurse BCNEPA/FPH/FPLIC Billing Manual November 2012 Standard Abbreviation PRO FEE/ER PRO FEE/OUTPT PRO FEE/CLINIC PRO FEE/SOC SVC PRO FEE/EKG PRO FEE/EEG PRO FEE/HOS VIS PRO FEE/CONSULT FEE/PVT NURSE Unit HCPCS Y Y Y Y Y Y Y Y Y Page 65 Form Locator 42 099x PATIENT CONVENIENCE ITEMS Charges for items that are generally considered by the third-party payers to be strictly convenience items and therefore are not covered by many health plans. Sub-Category 0 General Classification 1 Cafeteria/Guest Tray 2 Private Linen Service 3 Telephone/Telecom 4 TV/Radio 5 Non-Patient Room Rentals 6 Late Discharge 7 Admission Kits 8 Beauty Shop/Barber 9 Other Convenience Items Standard Abbreviation PT CONVENIENCE CAFETERIA LINEN TELEPHONE TV/RADIO NONPT ROOM RENT LATE DISCHARGE ADMIT KITS BARBER/BEAUTY PT CONV/OTH Unit HCPCS Unit HCPCS 100x BEHAVIORAL HEALTH ACCOMMODATIONS Charges for routine accommodations at specified behavior health facilities. Sub-Category 0 General Classification 1 Residential Treatment - Psychiatric 2 Residential Treatment - Chemical Dependency 3 Supervised Living 4 Halfway House 5 Group Home 6-9 RESERVED Standard Abbreviation BH R&B BH R&B RES/PSYCH BH R&B RES/CHEM DEP Day Day BH R&B SUP LIVING BH R&B HALFWAY HOUSE BH R&B GROUP HOME Day Day Day 101x to 209x RESERVED 210x ALTERNATIVE THERAPY SERVICES Charges for therapies not elsewhere categorized under other therapeutic service revenue codes (042x, 043x, 044x, 091x, 094x, 095x) or services such as anesthesia or clinic (0374, 0511). Sub-Category 0 General Classification 1 Acupuncture 2 Acupressure 3 Massage 4 Reflexology 5 Biofeedback 6 Hypnosis 7-8 RESERVED 9 Other Alternative Therapy Service Standard Abbreviation ALTTHERAPY ACUPUNCTURE ACUPRESSURE MASSAGE REFLEXOLOGY BIOFEEDBACK HYPNOSIS Unit Session Session Session Session Session Session OTHER ALTTHERAPY Session HCPCS Notes: Alternative therapy is intended to enhance and improve standard medical treatment. These revenue code(s) would be used to report services in a separately designated alternative inpatient/outpatient unit. 211x to 309x RESERVED BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 66 Form Locator 42 310x ADULT CARE Charges for personal, medical, psycho-social, and/or therapeutic services in a special community setting for adults needing supervision and/or assistance with Activities of Daily Living (ADL). Sub-Category 0 RESERVED 1 Adult Day Care, Medical and SocialHourly 2 Adult Day Care, Social-Hourly 3 Adult Day Care, Medical and Social- Daily 4 Adult Day Care, Social-Daily 5 Adult Foster Care Daily 6-8 RESERVED 9 Other Adult Care Standard Abbreviation Unit ADULT MED/SOC HR Hour ADULT SOC HR ADULT MED/SOC DAY ADULT SOC DAY ADULT FOSTER DAY Hour Day Day Day HCPCS OTHER ADULT 311x to 999x RESERVED Form Locator 43 Data Element Revenue Description/IDE Number/Medicaid Drug Rebate Definition: The standard abbreviated description of the related revenue code categories included on this bill. (See FL 42 for description of each revenue code category.) FL 43 is also used to report Investigational Device Exemption (IDE) Numbers and information on Medicaid drug rebates. Required Yes - for paper bills only Reporting UB-04: Required (for paper bills only) 004010/004010A1, 005010: Not Used Field Attributes 1 Field 22 Lines* 24 Positions Alphanumeric Left-justified Notes The standard abbreviated description should correspond with the Revenue Codes as defined by the NUBC. * The 23rd line contains an incrementing page count and total number of pages for the claim on each page, creation date of the claim on each page, and a claim total for covered and non-covered charges on the final claim page only indicated with a Revenue Code of “0001”. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 67 Form Locator 44 Data Element HCPCS/Accommodation Rates/HIPPS Rate Codes Definition: 1. The Healthcare Common Procedure Coding System (HCPCS) applicable to ancillary service and outpatient bills. 2. The accommodation rate for inpatient bills. 3. Health Insurance Prospective Payment System (HIPPS) rate codes represent specific sets of patient characteristics (or case-mix groups) on which payment determinations are made under several prospective payment systems. Required See reporting Reporting HCPCS and HIPPS Rate Codes UB-04: Situational. Required for outpatient claims when an appropriate procedure or HIPPS code exists for this service line item. OR Required for inpatient claims when an appropriate HCPCS (drugs and/or biologics only) or HIPPS code exists for this service line item. 004010/004010A1: Situational 005010X223A2: Situational. Required for outpatient claims when an appropriate procedure code exists for this service line item. OR Required for inpatient claims when an appropriate HCPCS (drugs and/or Biologics only) or HIPPS code exists for this service line item. Accommodation Rates UB-04: Required when a room & board revenue code is reported. 004010/004010A1: Required when the associated revenue code is 100-219. 005010: Not Used. (Rationale: The rate can be computed by dividing the total charge by the number of units.) HCPCS Modifiers UB-04: Required when a modifier clarifies or improves the reporting accuracy of the associated procedure code. 004010/004010A1: Required when the Provider needs to convey additional clarification for the associated procedure code. 005010: Required when a (first, second, third or fourth) modifier clarifies or improves the reporting accuracy of the associated procedure code. Field Attributes 1 Field 22 Lines (a) 14 Positions (b) Numeric for Accommodation Rate; alphanumeric for HCPCS and HIPPS Rate Codes. Right-justified for Accommodation Rates; left-justified for HCPCS and HIPPS Rate Codes. Dollar values reported for Accommodation Rates must include whole dollars, the decimal, and the cents. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 68 Form Locator 44 Notes Field Attributes (a) The 23rd line contains an incrementing page count and total number of pages for the claim on each page, creation date of the claim on each page, and a claim total for covered and non-covered charges on the final claim page only indicated using Revenue Code 0001. (b) For HCPCS, the filed consists of 5 positions for the base code plus 8 positions for up to four HCPCS modifiers; thus, the field contains one extra/unused position. (c) HIPPS rate code are alphanumeric codes of 5 positions. Each code contains intelligence, with certain positions of the code indicating the case mix group itself, and other positions providing additional informational; the additional information varies amount HIPPS codes. HIPPS Rate Codes The Centers for Medicare and Medicaid services develops and publishes the HIPPS codes to establish a coding system for claims submission and claims payment under prospective payment systems. These codes represent the case mix classification groups that are used to determine payment rates under prospective payment systems. Case mix classification groups include, but may not be limited to, resource utilization groups (RUGs) for skilled nursing facilities, home health resource groups (HHRGs) for home health agencies, and case mix groups (CMGs) for inpatient rehabilitation facilities. HCPCS Modifiers (Level I and Level II) The UB-04 accommodates up to four modifiers, two characters each. Various CPT (Level I HCPCS) and Level II HCPCS codes may require the use of modifiers to improve the accuracy of coding. Consequently, reimbursement, coding consistency, editing and proper payment will benefit from the reporting of modifiers. Hospital should not report a separate HCPCS (five-digit code) instead of the modifier. When appropriate, report a modifier bas on the list indicated in the above section of the AMA publication. Form Locator 45 Data Element Service Date Definition: The date (MMDDYY) the outpatient service was provided. (Applies to Lines 1-22; Line 23 refers to the Creation Date (MMDDYY) of the bill (the date bill was created/printed)). This field is also used to report the assessment reference date when billing SNF PPS services (Type of Bill 021x). Required Required on outpatient claims Reporting Service Date UB-04: Required on outpatient claims. 004010/004010A1: Required on outpatient claims when revenue, procedure, HIEC or drug codes are reported in the SV2 segment. 005010: Required on outpatient service line where a drug is not being billed and the Statement Covers Period is greater than one day. OR Required on service lines where a drug is being billed and the payer’s adjudication is known to be impacted y the drug duration or the date the prescription was written. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 69 Form Locator 45 Reporting Assessment Date Require when this field is used to report the assessment reference date when billing SNF PPS services (Type of Bill 021x). 005010: Not Used Creation Date Required for Line 23 (Creation Date). Enter the date the bill was created or prepared for submission. Creation Date on Line 23 should be reported on all pages of the UB-04. Field Attributes Service Date: 1 Field 22 Lines Numeric Right-justified Data Element Service Units Definition: A quantitative measure of services rendered by revenue category to or for the patient to include items such as number of accommodation days, miles, pints f blood, renal dialysis treatments, etc. Required Yes Reporting UB-04, 004010/004010A1, 005010: Required Field Attributes 1 Field Numeric Notes Enter the total number of covered accommodation days, ancillary units of service, or visits, where appropriate. Leading zeros should not be reported. If the amount is an integer, no decimal point is reported. The maximum length for this field is 7 digits excluding the decimal. When a decimal is used, the maximum number of digits allowed to the right of the decimal is three. 6 Positions Creation Date: 1 Field 1 Line (23) 6 Positions Numeric Right-justified Form Locator 46 22 Lines Right-justified 7 Positions Decimal The following notes are intended as general guidance. Inpatient Room & board accommodations: Units reflect the total number of days of care provided to the patient. Other revenue codes: Although the inpatient UB-04 is a summary level claim, units can be reported as “1” or more based on the provider’s practice, health plan requirements or regulation. A zero or negative value is not allowed. Outpatient When HPCPS codes are reported, the unit is defined by the HCPCS definition. Where the unit is not defined by the HCPCS code, units can be reported as “1” or more based on the provider’s practice, health plan requirements or regulation. A zero or negative value is not allowed. Form Locator 47 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 70 Data Element Total Charges Definition: Total Charges for the primary payer pertaining to the related revenue code for the current billing period as entered in the statement covers period. Total Charges includes both covered and non-covered charges. Required Yes Reporting Line Item Charges Required: UB-04 (Lines 1-22). 004010/004010A1, 005010 Loop ID 2400 | SV203 Total (Summary) Charges Required: UB-04 Line 23 of the final claim page using Revenue Code 0001. (Revenue 0001 is not used on electronic transactions; report the total claim charge in the appropriate data segment/field as indicated below.) 004010/004010A1, 005010 Loop ID 2300 | CLM02 Field Attributes 1 Field Numeric Notes There are 7 positions for dollars, 2 positions for cents. Amounts greater than or equal to zero are acceptable values for this element. The 23rd line contains an incrementing page count and total number of pages for the claim on each page, creation date of the claim on each page, and a claim total for covered and non-covered charges on the final claim page only indicated using Revenue Code 0001. 23 Lines * Right-justified 9 Positions (see notes) Form Locator 48 Data Element Non-covered Charges Definition: To reflect non-covered charges for the destination payer as it pertains to the related revenue code. Required Not required Reporting Line Item Non-Covered Charges Required: UB-04: Lines 1-22. Required if needed to report line specific non-covered charge amount. 004010/004010A1: Situational 005010: Required if needed to report line specific non-covered charge amount. Total (Summary) Non-Covered Charges Required: UB-04: Required on Line 23 of the final claim page using Revenue code 00001 when there are non-covered charges on the claim. 004010/004010A1, 005010: Not Used Field Attributes 1 Field Right-justified 23 Lines * 9 Positions (see Notes) Numeric Notes There are 7 positions for dollars, 2 positions for cents. * The 23rd line contains an incrementing page count and total number of pages for the claim on each page, creation date of the claim on each page, and a claim total for covered and non-covered charges on the final claim page only indicated using Revenue Code 0001. Form Locator 49 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 71 Data Element Reserved for Assignment by the NUBC Reporting Not used Field Attributes 1 Field 23 Lines 2 Positions Alphanumeric Left-justified Form Locator 50 Data Element Payer Name Definition: Name of health plan that the provider might expect some payment for the bill. Required Yes Reporting UB-04: Line A Required. Lines B and C Situational. Required when other payers are known to potentially be involved in paying this claim. 004010/004010A1, 005010: Required Field Attributes 1 Field Notes A = Primary Payer B = Secondary Payer C = Tertiary Payer 3 Lines 23 Positions Alphanumeric Left-justified Example: If “Medicare” is entered in Form Locator 50A, this indicates that the provider has determined based on the responses form the patient or the patient’s representative or from the insurance enrollment card information that Medicare is the primary payer. Form Locator 51 Data Element Health Plan Identification Number Definition: The number used by the health plan to identify itself. Required No Reporting Report the HIPAA National Plan Identifier when it become mandated; otherwise report the (legacy/proprietary) number (i.e., whatever number used has been defined between trading partners). UB-04: Line A Required. Lines B and C Situational. Required when other health plans are known to potentially be involved in paying this claim. 004010/004010A1, 005010: Required Field Attributes 1 Field 3 Lines 15 Positions Alphanumeric Left-justified Form Locator 52 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 72 Data Element Release of Information Certification Indicator Definition: Code indicating whether the provider has on file a signed statement (from the patient or the patient’s legal representative) permitting the provider to release data to another organization. Required Yes Reporting UB-04 and 005010: Required. See “code structure” noted below. 004010/004010A1: Required. Note: The 004010/004010A1 includes additional codes that are no longer applicable due to the HIPAA medical privacy rule. Field Attributes 1 Field Notes The Release of Information response is limited to the information carried in this claim. 3 Lines 1 Position Alphanumeric Left-justified A = Primary B = Secondary C = Tertiary Code Structure I Informed Consent to Release Medical Information for Conditions or Diagnoses Regulated by Federal Statutes Usage Note: Required when the provider has not collected a signature and state or federal laws do not supersede the HIPAA Privacy Rule by requiring a signature be collected. Y Yes, Provider has a Signed Statement Permitting Release of Medical Billing Data Related to a Claim Usage Note: Required when state or federal laws do not supersede the HIPAA Privacy Rule by requiring a signature be collected. Form Locator 53 Data Element Assignment of Benefits Certification Indicator Definition: Code indicates provider has a signed form authorizing the third party payer to remit payment directly to the provider. Required Yes Reporting UB-04, 004010/004010A1, 005010: Required Field Attributes 1 Field 3 Lines 1 Position Alphanumeric Left-justified Form Locator 53 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 73 Notes Health plans that have arrangements with affiliate health plans in different states may utilize this code to make payments to the provider rather than the insured individual. This element answers the question whether or not the insured has authorized the plan to remit payment directly to the provider. The presence of an assignment does not permit release of medical information about a patient. Code Structure N No W Not Applicable (Use code ‘W’ when the patient refuses to assign benefits.) Y Yes Form Locator 54 Data Element Prior Payments - Payer Definition: The amount the provider has received (to date) by the health plan toward payment of this bill. Required If applicable Reporting UB-04: Required when the indicated payer has paid an amount to the provider towards this bill. Report “0.00” if there is no payment made by the health plan or payment was applied to coinsurance or deductible. 004010/004010A1: Required when the present payer ha paid an amount to the provider towards this bill. 005010: Required when the claim has been adjudicated by the payer identified in Loop ID2330B of this loop. OR Required when Loop ID-2919AC is present. In this case, the claim is a post payment recovery claim submitted by a subrogated Medicaid agency. Field Attributes 1 Field Notes There are 8 positions for dollars, 2 positions for cents. 3 Lines 10 Positions Numeric Right-justified A = Primary B = Secondary C = Tertiary Form Locator 55 Data Element Estimated Amount Due - Payer Definition: The amount estimated by the provider to be due from the indicated payer (estimated responsibility less prior payments). Required If applicable Reporting UB-04: Required when the provider estimates an amount due from the indicated payer. 004010/004010A1: Required when the Payer Estimated Amount Due is applicable to this claim. 005010: Not Used Form Locator 55 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 74 Field Attributes 1 Field 3 Lines 10 Positions Alphanumeric Notes There are 8 positions for dollars, 2 positions for cents. Left-justified A = Primary B = Secondary C = Tertiary Form Locator 56 Data Element National Provider Identifier - Billing Provider Definition: The unique identification number assigned to the provider submitting the bill: NPI is the national provider identifier. Required Yes Reporting The NPI Final Rule was implemented May 23, 2008. UB-04: Required for providers in the United States or its territories on or after the mandated HIPAA National Provider Identifier (NPI) implementation date when the provider is eligible to receive an NPI. OR 005010: Required for providers not in the United States or its territories when the provider has received an NPI. OR Required for providers prior to the mandated NPI implementation date when the provider has received an NPI and the submitter has the capability to send it. Field Attributes 1 Field 3 Lines 15 Positions* Alphanumeric *Note: The NPI is ten characters in length. Left-justified* Notes Proprietary identifiers necessary for the receiver to identify Billing Providers that area not covered entities are to be reported in FL 57 Lines A-C. Form Locator 57 Data Element Other (Billing) Provider Identifier Definition: A unique identification number assigned to the provider submitting the bill by the health plan. Required Yes Form Locator 57 Reporting The NPI Final Rule was implemented May 23, 2008. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 75 004010/004010A1: NPI usage is not applicable due to the implementation of the NPI Final Rule. UB-04: Required when NPI is not used in FL 56 and an identification number other than the NPI is necessary for the receiver to identify the provider. 005010: Required when NM109 in Loop 2010AA is not used and an identification number other than the NPI is necessary for the receiver to identify the provider. Field Attributes 1 Field 3 Lines 15 Positions Alphanumeric Left-justified Notes The UB-04 does not use a qualifier to specify the type of Other (Billing) Provider Identifier. Use this field to report other provider identifiers as assigned by the health plan (as indicated in FL 50 Lines A-C). Form Locator 58 Data Element Insured’s Name Definition: The name of the individual under whose name the insurance benefit is carried. Required Yes Reporting UB-04, 004010/004010A1, 005010: Required Field Attributes 1 Field Notes A = Primary Payer B = Secondary Payer C = Tertiary Payer 3 Lines 25 Positions Alphanumeric Left-justified Use a comma or space to separate land and first names. Enter last name first. No space should be left between a prefix and a name as in MacBeth, and McEnroe. Titles (such as Sir, Msgr, Dr.) should not be recorded in this data element. Record hyphenated names with the hyphen as in Smith-Jones, Rebecca. To record suffix of a name, write the last name, leave a space and write the suffix, then write the first name as in Snyder III, Harold, or Addams JR., Glen Form Locator 59 Data Patient’s Relationship to Insured BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 76 Element Definition: Code indicating the relationship of the patient to the indentified insured. Required Yes Reporting UB-04: Line A required. Lines B and C Situational. Required when other payers are known to potentially be involved in paying on this claim. 004010/004010A1: Required. If the patient is the subscriber, report in Loop ID 2000B. Required if the patient is not the subscriber but has a unique identifier assigned by the destination payer, report in Loop ID 2000C. 005010: Required. If the patient is the subscriber, the name is reported in Loop ID 2000B. If the patient is not the subscriber but has a unique identifier assigned by the destination payer, the name is reported in Loop ID 2000B. If the patient is not the subscriber and cannot be identified by a unique identifier assigned by the destination payer, report in Loop ID 2000C. Field Attributes 1 Field Notes A = Primary Payer B = Secondary Payer C = Tertiary Payer Code 01 18 19 20 21 39 40 53 G8 3 Lines 2 Positions Alphanumeric Left-justified Title Spouse Self Child Employee Unknown Organ Donor Cadaver Donor Life Partner Other Relationship Form Locator 60 Data Element Insured’s Unique Identifier Definition: The unique number assigned by the health plan to the insured. Required Yes Reporting UB-04: Line A Required. Lines B and C Situational. Required when other health plans are known to potentially be involved in paying this claim. 004010/004010A1, 005010: Required Field Attributes 1 Field Notes A = Primary Payer B = Secondary Payer C = Tertiary Payer 3 Lines 20 Positions Alphanumeric Left-justified Form Locator 61 Data Insured’s Group Name BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 77 Element Definition: The group or plan name through which the insurance is provided to the insured. Required Reporting UB-04: Line A Situational. Required if the Group Name is available and FL 62 (Insurance Group Number) is not used. Lines B and C Situational. Required when other insurance/payers/health plans are known to potentially be involved in paying this claim and when FL62 B and C are not used. 004010/004010A1: Situational. Used only when no group number is reported. 005010: Required when Group Number (Loop ID 2000B) is not used and the group name is available. Field Attributes 1 Field Notes A = Primary Payer B = Secondary Payer C = Tertiary Payer 3 Lines 14 Positions Alphanumeric Left-justified Form Locator 62 Data Element Insured’s Group Number Definition: The identification number, control number, or code assigned by the carrier or administrator to identify the group under which the individual is covered. Required Yes Reporting UB-04: Line A Situational. Required when the insured’s identification card shows a group number. Lines B and C Situational. Required when other insurance/payers/health plans are known to potentially be involved in paying this claim and when the other insurance’s identification card shows a group number. 004010/004010A1: Situational 005010: Required when the subscriber’s identification card for the destination payer (Loop ID 2010BB) shows a group number. Field Attributes 1 Field Notes A = Primary Payer B = Secondary Payer C = Tertiary Payer 3 Lines 17 Positions Alphanumeric Left-justified Form Locator 63 Data Authorization Code/Referral Number BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 78 Element Definition: An identifier that designates that services on this bill have been authorized by the payer or indicates that a referral is involved. Required No Reporting Authorization UB-04: Situational. Required when an authorization code is assigned by the payer or UMO (Utilization Management Organization) is required to be reported on the claim. 004010/004010A1: Situational. Required where services on this claim were preauthorized or where a referral is involved. 005010: Situational. Required when an authorization code is assigned by the payer or UMO (Utilization Management Organization) AND the services on this claim were preauthorized. Referral Number UB-04: Situational. Required when a referral number is code assigned by the payer or UMO (Utilization Management Organization) AND a referral is involved. 004010/004010A1: Situational. Required where services on this claim were preauthorized or where a referral is involved. 005010: Situational. Required when a referral number is assigned by the payer or UMO (Utilization Management Organization) AND a referral is involved. Field Attributes 1 Field 3 Lines 30 Positions Notes A = Authorization Code B = Referral Number C = Secondary Payer Authorization Code Alphanumeric Left-justified Form Locator 64 Data Element Document Control Number (DCN) Definition: The control number assigned to the original bill by the health plan or the health plan’s fiscal agent as part of their internal control. Required No Reporting UB-04: Situational. Required when Type of Bill Frequency Code (FL 04) indicates this claim is a replacement or void to a previously adjudicated claim. 004010/004010A1: Situational 005010: Situational. (Payer Claim Control Number) required when CLM05-3 (Claim Frequency Code) indicates this claim is a replacement or void to a previously adjudicated claim. Form Locator 64 Field 1 Field BCNEPA/FPH/FPLIC Billing Manual November 2012 3 Lines 26 Positions Alphanumeric Left-justified Page 79 Attributes Notes A = Primary Payer B = Secondary Payer C = Tertiary Payer Payer A’s ICN/DCN should be shown on Line “A” of FL 64. Similarly, the ICN/DCN for Payers B and C should be shown on lines B and C respectively, of FL 64. Form Locator 65 Data Element Employer Name (of the Insured) Definition: The name of the employer that provides health care coverage for the insured individual identifier in FL 58. Required No Reporting UB-04: Situational. Lines A, B, C required when the employer of the insured is known to potentially be involved in paying on this claim. 004010/004010A1 and 005010: Not Used Field Attributes 1 Field Notes A = Primary Payer B = Secondary Payer C = Tertiary Payer 3 Lines 25 Positions Alphanumeric Left-justified Form Locator 66 Data Element Diagnosis and Procedure Code Qualifier (ICD Version Indicator) Definition: The qualifier that denotes the version of International Classification of Diseases (ICD) reported. Required No Reporting UB-04: Qualifier Code “9” Required on claims through September 30, 2014. ICD-9-CM cannot be reported on HIPAA covered entity claims on or after October 1, 2014 (a). The NUBC strongly encourages all entities – covered and non-covered alike – to follow the diagnosis and procedure code rules in effect pre and post October 1, 2014(a). Qualifier Code “0” designating ICD-10-CM and ICD-10-PCS can only be used on or after October 1, 2014(a) based on a final rule naming ICD-10-CM and ICD-10-PCS as allowable code sets under HIPAA, and a proposed rule dated 4/17/12 changing the compliance date from October 1, 2013 to October 1, 2014. OR For claims which are not covered under HIPAA (before October 1, 2014(a)). Form Locator 66 Reporting 004010/004010A1: Not Applicable. Only ICD-9-CM qualifier codes are available in version 4010/4010A1. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 80 005010: Data Element not Applicable. Version 5010 contains distinct qualifier codes for ICD-9-CM (“BF”), ICD-10-CM (“ABF”) and ICD-10-PCS (“BBR”). “ABF” and “BBR” that can only be used on or after October 1, 2014(a) based on a final rule naming the ICD-10CM and ICD-10-PCS as allowable code sets under HIPAA, and a proposed rule dated 4/17/12 changing the compliance date from October 1, 2013 to October 1, 2014. OR For claims which are not covered under HIPAA (before October 1, 2014(a ). Field Attributes 1 Field 1 Lines 1 Positions Alphanumeric Notes Qualifier codes reflects the edition portion of the ICD: 9 - Ninth Revision 0 - Tenth Revision Left-justified (a) In a proposed rule dated 4/17/12, DHHS proposed to change the compliance date for the International Classification of Diseases, 10th Revision, Clinical Modification (ICD-10-CM) for diagnosis coding, including the Official ICD-10-CM Guidelines for Coding and Reporting, and the International Classification of Diseases, 10th Revision, Procedure Coding System (ICD-10-PCS) for inpatient hospital procedure coding, including the Official ICD-10-PCS Guidelines for Coding and Reporting, from October 1, 2013 and October 1, 2014. Form Locator 67 Data Element Principal Diagnosis Code and Present on Admission Indicator Definition: The ICD-9-CM codes describing the principal diagnosis (i.e., the condition established after study to be chiefly responsible for occasioning the admission of the patient for care.) See FL 67 for information on the Present on Admission Indicator noted below. For additional information, refer to the Official ICD-9-CM Guidelines for Coding and Reporting. Required Yes Reporting UB-04, 004010/004010A1, 005010: Principal Diagnosis Code – Required Present on Admission Indicator - See FL 67 for further information on usage. Field Attributes 1 Field 1 Line Alphanumeric Left-justified 8 Positions (1-7: Principal Diagnosis Code; position 8 (shaded area): Present on Admission Indicator) Notes Follow the official coding guidelines for ICD reporting. The reporting of the decimal between the third and fourth digit is unnecessary because it is implied. The principal diagnosis code will include the use of “V” codes. Present on Admission (POA) Indicator The eighth digit of FL 67 - Principal Diagnosis and each of the secondary diagnosis fields FL A-Q. The eighth digit of FL 72 – External Cause of Injury (ECI) (3 fields on the form). Form Locator 67 Notes Present on Admission (POA) Indicator BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 81 General Reporting Requirements All claims involving inpatient admissions to general acute care hospitals or other facilities that are subject to a law or regulation (e.g., Deficit Reduction Act of 2005) mandating collection of present on admission information. Effective 1/1/2011: All claims involving inpatient admissions to general acute care hospitals or other facilities that are subject to a law or regulation (e.g. Deficit Reduction Act of 2005) mandating collection of present on admission information, or as mutually agreed to under contract with an insurance program. Present on admission is defined as present at the time the order for inpat4ient admission occurs – conditions that develop during an outpatient encounter, including emergency department, observation, or outpatient surgery, are considered as present on admission. POA indicator is assigned to principal and secondary diagnoses ( as defined in Section II of the Official Guidelines for Coding and Reporting) and the external cause of injury codes. Issues related to inconsistent, missing, conflicting or unclear documentation must still be resolved by the provider. If a condition would not be coded and reported based on UHDDS definitions and current official coding guidelines, then the POA indicator would not be reported. Reporting Options The five reporting options for all diagnosis reporting are as follows: Code Y Yes N No U No Information in the Record W Clinically Undetermined Blank Field on UB-04/ Exempt from POA Reporting Not Populated in 005010 837 Effective July 1, 2011 1 on UB-04 Only/Not Exempt from POA Reporting Populated in 005010 837 Reporting Definitions: Code Y N U Definition Present at the time of inpatient admission Not present at the time of inpatient admission Documentation is insufficient to determine if condition is present on admission W = Provider is unable to clinically determine whether condition was present on admission or not Effective July 1, 2011 1* = Exempt from POA Reporting = = = * UB-04 only; not for use on 837 Form Locator 67 Notes Present on Admission (POA) Indicator (continued) BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 82 Health plans that receive POA information on the claim should not reject the claim if their claims processing systems have no use for any of the POA information. The American Health Information Management Association, American hospital Association, CMS and the National Center for Health Statistics (known as the “Cooperating Parties”) has published a list of ICD-9-CM codes that are exempt from POA reporting. The indicator can be left unreported only for the codes on this list, that is, the filed is left blank on the paper form and “Not Used” on the 00510 837 electronic claim. The list of exempt diagnosis codes will be included in the POA guideline published in the ICD-9-CM Official Guidelines for Coding and Reporting (Appendix I - Present on Admission Reporting Guidelines). These guidelines will be updated as needed to address identified coding errors or areas of confusion. POA for 00410/00410A1 837 Medicare Claims Section 5001© of the Deficit Reduction Act of 2005 requires hospitals to begin reporting the secondary diagnoses that are present on the admission (POA) of patients effective for discharges on or after October 1, 2007. Effective October 1, 2007, Medicare will begin to accept a POA indicator for every diagnosis on your inpatient acute care hospital claims. However, providers must submit the POA on hospital claims beginning with discharges on or after January 1, 2008. Critical access hospitals, Maryland waiver hospitals, long term care hospitals, cancer hospitals, and children’s inpatient facilities are exempt from this requirement. CMS does not require a POA indicator for the external cause of injury code unless it is being reported as an “other diagnosis.” CMS Reporting Options and Definitions Y = Yes = present at the time of inpatient admission N = No = not present at the time of inpatient admission U = Unknown = the documentation is insufficient to determine if the condition was present at the time of inpatient admission. W = Clinically Undetermined = the provider is unable to clinically determine whether the condition was present at the time of inpatient admission or not 1 = Unreported/Not used - Exempt from POA reporting. This code is the equivalent code of a blank on the UB-04, however, it was determined that blanks were undesirable when submitting this data via the 0410/00410A1 The POA element on your electronic claims must contain the letters “POA” followed by a single POA indicator for every diagnosis that your report. The POA indicator for the principal diagnosis should be the first indicator after “POA,” and (when applicable) the POA indicators for secondary diagnoses would follow. The last POA indicator must be followed by the letter “Z” to indicate the end of the data element (or FIs and A/B MACs will allow the letter “X” which CMS may use to identify special data processing situations in the future). Form Locator 67 Notes Present on Admission (POA) Indicator (continued) BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 83 POA for 00410/00410A1 837 Medicare Claims Note that on paper claims the POA is the eighth digit of the Principal Diagnosis field (FL 67), and the eighth digit of each of the secondary diagnosis fields (FL 67 A-Q); and on claims submitted electronically via 00410/00410A1 837 format, you must use segment K3 in the 2300 loop, data element K301. Below is an example of what this coding should look like on an electronic claim: If segment K3 read as follows: “POAYNUWIYZ,” it would represent the POA indictors for a claim with 1 principal and 5 secondary diagnoses. The principal diagnosis was POA (Y), the first secondary diagnosis was not POA (N), it was unknown if the second secondary diagnosis was POA (U), it is clinically undetermined if the third secondary diagnosis was POA (W), the fourth secondary diagnosis was exempt from reporting for POA (1), and the fifth secondary diagnosis was POA (Y). As of January 1, 2008, all direct data entry (DDE) screens will allow for the entry of POA data and POA data will also be included with any secondary claims sent by Medicare for coordination of benefits purposes. The official instruction, CR5679, issued to FIs or A/B MACs can be found at http://www.cms.hhs.gov/Transmittals/downloads/R289OTN.pdf. Hospitals Exempt from Present on Admission (POA) Reporting (i.e. non-Inpatient Prospective Payment System (IPPS) Hospitals) and the Grouper Although POA reporting is not required for IPPS exempt hospitals, their claims still process through Grouper. Some exempt hospitals report the POA, however, due to other payer requirements or business needs. When exempt hospitals report the POA, they must include an “X” to indicate the end of POA reporting in the K3 segment of the claim. The “X” indicator will prevent Grouper from Applying Hospital-Acquired Condition (HAC) Diagnosis Related Group (DRG) logic to the claim. Effective October 1, 2008, FISS will automatically replace any reported ‘Z’ indicator with an ‘X’ for providers exempt from reporting POA. However, exempt providers should begin to report an ‘X’ to indicate the end of POA reporting as soon as possible. The official instruction, CR6086, can be found at http://www.cms.hhs.gov/Transmittals/downloads/R354OTN.pdf. Form Locator 67A-Q Data Other Diagnosis Code and Present on Admission Indicator BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 84 Element Definition: The ICD-9-CM codes corresponding to all conditions that coexist at the time of admission, that develop subsequently, or that affect the treatment received and/or length of stay. Exclude diagnoses that relate to an earlier episode which have no bearing on the current hospital stay. For additional information, refer to the Official ICD-9-CM Guidelines for Coding and Reporting. Required Reporting Other Diagnosis Codes UB-04: Situational. Required when other condition(s) coexist or develop(s) subsequently during the patient’s treatment. 004010/004010A1: Situational. Required when other condition(s) coexists with the Principal Diagnosis, coexists at the time of admission or develops subsequently during the patient’s treatment. 005010: Situational. Required when other condition(s) coexist or develop(s) subsequently during the patient’s treatment. Present on Admission Indicator For use on the UB-04 and 00510 only; not for use in any manner on 004010/004010A1 Field Attributes 17 Fields 2 Lines Alphanumeric Left-justified 8 Positions (1-7: Principal Diagnosis Code; position 8 (shaded area): Present on Admission Indicator) Notes The reporting of the decimal between the third and fourth digits is unnecessary because it is implied. Other diagnoses codes will permit the use of ICD-9-CM “V” and “E” codes where appropriate. Other diagnosis is interpreted as additional conditions that affect patient care in terms of requiring: Clinical Evaluation, or Therapeutic Treatment, or Diagnostic Procedures, or Extended Length of Hospital Stay, or Increased Nursing Care and/or Monitoring. Form Locator 68 Data Element Reserved for Assignment by the NUBC Definition: Reporting Not Used Field Attributes 1 Field 2 Lines 8 Positions (Line 1) Alphanumeric 9 Positions (Line 2) Left-justified Form Locator 69 Data Admitting Diagnosis Code BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 85 Element Definition: The ICD diagnosis code describing the patient’s diagnosis at the time of admission. Required Yes - Inpatient only Reporting UB-04: Situational. Required when claim involves an inpatient admission. Required on 012x, 022x and inpatient claims (“IP”) except 028x, 065x, 066x, 084x, 086x. 004010/004010A1: Situational. The Admitting Diagnosis is required on all inpatient admission claims and encounters. 005010: Situational. Required when claim involves an inpatient admission. Field Attributes 1 Field Notes The ICD-9-CM diagnosis code describing the admitting diagnosis as a significant finding representing patient distress, an abnormal finding on examination, a possible diagnosis based on significant findings, a diagnosis established from a previous encounter or admission, an inquiry, a poisoning, or a reason or condition (not an illness or injury) such as follow-up or pregnancy in labor. Report only one admitting diagnosis. This condition shall be determined based on the ICD-9-CM coding directives in Volumes I and II of the ICD-9-CM coding manuals (ICD-9-CM codes 001 – V82.9). The reporting of the decimal between the third and fourth digits is unnecessary because it is implied. 1 Line 7 Positions Alphanumeric Left-justified Form Locator 70a-c Data Element Patient’s Reason for Visit BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 86 Definition: The ICD-CM diagnosis codes describing the patient’s reason for visit at the time of outpatient registration. Required Reporting UB-04: Situational. 1. Required for all unscheduled outpatient visits. An “unscheduled” outpatient visit is defined as an outpatient Type of Bill 013x, 085x, or 078x together with FL 14 (Priority of Visit/Type of Admission) codes 1,2 or 5 and Revenue Codes 045x, 0516, 0526, or 0762 (Observation Hours). 2. May be reported at submitter’s discretion for scheduled outpatient visits (such as encounters for ancillary tests) when this information provides additional information to support medical necessity. This information may be any documented reason for the service provided, including patient’s stated reason for seeking care or the reason provided by the physician as part of the order for the service. This information is not required for all scheduled outpatient encounters. 3. Payers should not reject outpatient claims that contain patient’s reason for visit information in FL 70 if this information is not needed for their adjudication of the claim. 004010/004010A1: Situational. Required for all unscheduled outpatient visits or upon the patient’s admission to the hospital. 005010: Situational. Required when claim involves outpatient visits. See ASC X12N/TG2 interpretation (RFI #1256) on Reporting Patient’s Reason for Visit (005010X223A2) http://www.x12.org/x12org/subcommittees/x12rfi.cfm (See specific UB-04 requirements above and FL 04.) Field Attributes 1 Field, 3 Subfields (a,b,c) 7 Positions 1 Line Alphanumeric Left-justified Notes The ICD-9-CM diagnosis code describing the patient’s stated reason for seeking care (or as stated by the patient’s representative). This may be a condition representing patient distress, an injury, a poisoning, or a reason or condition (not an illness or injury) such as follow-up or pregnancy in labor. Report the first diagnosis code describing the patient’s primary reason for seeking care in subfield a. This condition shall be determined based on the ICD-9-CM coding directives in Volumes I and II of the ICD-9-CM coding manuals (ICD9-CM codes 001 - V82.9). There are two other diagnosis code subfields to report additional reasons for the patient’s visit for care. Reporting the decimal between the third and fourth digits is unnecessary because it is implied. Form Locator 71 Data Element Prospective Payment System (PPS) Code BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 87 Definition: The PPS code assigned to the claim to identify the DRG based on the grouper software called for under contract with the primary payer. Required Reporting UB-04: Situational. Required for inpatient claims when the hospital is under contract with the health plan to provide this information. 004010/004010A1: Situational. Required when an inpatient hospital is under DRG contract with a payer and the contract requires the provider to identify the DRG to the payer. 005010: Situational. Required when an inpatient hospital is under DRG contract with a payer and the contract requires the provider to identify the DRG to the payer. Field Attributes 1 Field 1 Line 4 Positions Right-justified (all positions fully coded) Note Many workers’ compensation programs require this information. Numeric Form Locator 72a-c Data External Cause of Injury (ECI) Code and Present on Admission Indicator BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 88 Element Definition: The ICD diagnosis codes pertaining to external cause of injuries, poisoning, or adverse effect. For additional information, refer to the Official ICD-9-CM Guidelines for Coding and Reporting. Required Reporting External Cause of Injury (ECI) Code UB-04: Situational. Required when an injury, poisoning, or adverse effect is the cause for seeking medical treatment or occurs during the medical treatment. 004010/004010A1: Situational. Required whenever a diagnosis is needed to describe an injury, poisoning or adverse effect. 005010: Situational. Required when an external Cause of Injury is needed to describe an injury, poisoning, or adverse effect. Present on Admission Indicator: For use on the UB-04 and 005010 only; not for use in any manner on 004010/004010A1. See FL 67 for further information on usage. Field Attributes 3 Fields 1 Line Left-justified 8 Positions (1-7: Principal Diagnosis Code; position 8 (shaded area): Present on Admission Indicator) Note The priorities for recording an ECI code in Form Locator 72a-c are: 1. Principal diagnosis of an injury or poisoning. 2. Other diagnosis of an injury, poisoning, or adverse effect directly related to the principal diagnosis. 3. Other diagnosis with an external cause. Form Locator 73 Data Element Reserved for Assignment by the NUBC Definition: Reporting Not Used Field Attributes 1 Field 1 Line Alphanumeric BCNEPA/FPH/FPLIC Billing Manual November 2012 9 Positions Left-justified Page 89 Form Locator 74 Data Element Principal Procedure Code and Date Definition: The ICD code that identifies the inpatient principal procedure performed at the claim level during the period covered by this bill and the corresponding date. Required Reporting UB-04: Situational. Required on inpatient claims when a procedure was performed. If not required (i.e., on outpatient claims) do not send. 004010/004010A1: Situational. Required on Home IV therapy claims or encounters when surgery was performed during the inpatient stay from which the course of therapy was initiated. Required on inpatient claims or encounters when a procedure was performed. 005010: Situational. Required on inpatient claims when a procedure was performed. If not required by the 005010 implementation guide, do not send. Field Attributes 1 Field (code) 1 Line 7 Positions Alphanumeric Left-justified Notes Reporting the decimal between the second and third digits of the ICD is unnecessary because it is implied. Enter date as MMDDYY 1 Field (date) 1 Line 6 Positions Numeric Right-justified Form Locator 74a-c Data Element Other Procedure Codes and Dates Definition: The ICD codes identifying all significant procedures other than the principal procedure and the dates (identified by code) on which the procedures were performed. Report those that are most important for the episode of care and specifically any therapeutic procedures closely related to the principal diagnosis. Required Reporting UB-04: Situational. Required on inpatient claims when additional procedures must be reported. If not required (i.e., on outpatient claims) do not send. 004010/004010A1: Situational. Required on Home IV therapy claims or encounters when surgery was performed during the inpatient stay from which the course of therapy was initiated. Required on inpatient claims or encounters when additional procedures must be reported. 005010: Situational. Required on inpatient claims when additional procedures must be reported. If not required by the 005010 implementation guide (TR3), do no send. Field Attributes 5 Fields (code) 1 Line 7 Positions Alphanumeric Left-justified Notes Reporting the decimal between the second and third digits of the ICD is unnecessary because it is implied. Enter date as MMDDYY BCNEPA/FPH/FPLIC Billing Manual November 2012 5 Fields (date) 1 Line 6 Positions Numeric Right-justified Page 90 Form Locator 75 Data Element Reserved for Assignment by the NUBC Definition: Required Reporting Not Used Field Attributes 1 Field Alphanumeric 4 Lines Left-justified 4 Positions Form Locator 76 Data Element Attending Provider Name and Identifiers Definition: The Attending Provider is the individual who has overall responsibility for the patient’s medical care and treatment reported in this claim. Required Yes Reporting Name UB-04 and 005010: Situational. Required when the claim contains any services other than non-scheduled transportation claims. 004010/004010A1: Situational. Required on all inpatient claims or encounters. Required to indicate the Primary Physician responsible on a Home Health Agency Plan of Treatment. Identifiers - National Provider Identifier The NPI Final Rule was implemented on May 23, 2008. For purposes of this manual, the 004010/004010A1 National Provider Identifier and Secondary Identifier situational usage is not applicable due to the implementation of the NPI Final Rule. UB-04: Situational. Required for providers in the United States or its territories when the provider is eligible to receive an NPI. OR Required for providers not in the United States or its territories when the provider has received an NPI. 005010: Situational. Required for providers in the United States or its territories on or after the mandated HIPAA NPI implementation date when the provider is eligible to receive an NPI. OR Required for providers not in the United States or its territories on or after the mandated HIPAA National Provider Identifier (NPI) implementation date when the provider has received an NPI. OR Required for providers prior to the mandated NPI implementation date when the provider has received an NPI and the submitter has the capability to send it. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 91 Form Locator 76 Reporting Identifiers - Secondary UB-04: Situational. Required when the NPI in this field is not used and an identification number other than the NPI is necessary for the receiver to identify the provider. 005010: Situational. Required prior to the mandated HIPAA National Provider Identifier (NPI) implementation date when an identification number other than the NPI is necessary for the receiver to identify the provider. OR Required on or after the mandated NPI Implementation Date when the NPI in this field is not used and an identification number other than the NPI is necessary for the receiver to identify the provider. Field Attributes 5 Fields 2 Lines Alphanumeric Left-justified Line 1: 11 Positions* - National Provider Identifier 2 Positions - Secondary Identifier Qualifier (see below) 9 Positions - Secondary Identifier Line 2: 16 Positions - Last Name 12 Positions - First Name *Note: The NPI is ten characters in length. Secondary Identifier Qualifiers: 0B - State License Number 1G - Provider UPIN Number G2 - Provider Commercial Number BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 92 Form Locator 77 Data Element Operating Physician Name and Identifiers Definition: The name and identification number of the individual with the primary responsibility for performing the surgical procedure(s). Required Reporting Name UB-04 and 005010: Situational. Required when a surgical procedure code is listed on this claim. 004010/004010A1: Situational. Required when any surgical procedure code is listed on this claim. Identifiers - National Provider Identifier The NPI Final Rule was implemented on May 23, 2008. For purposes of this manual, the 004010/004010A1 National Provider Identifier and Secondary Identifier situational usage is not applicable due to the implementation of the NPI Final Rule. UB-04: Situational. Required for providers in the United States or its territories when the provider is eligible to receive an NPI. OR Required for providers not in the United States or its territories when the provider has received an NPI. 005010: Situational. Required for providers in the United States or its territories on or after the mandated HIPAA NPI implementation date when the provider is eligible to receive an NPI. OR Required for providers not in the United States or its territories on or after the mandated HIPAA National Provider Identifier (NPI) implementation date when the provider has received an NPI. OR Required for providers prior to the mandated NPI implementation date when the provider has received an NPI and the submitter has the capability to send it. Identifiers - Secondary UB-04: Situational. Required when the NPI in this field is not used and an identification number other than the NPI is necessary for the receiver to identify the provider. 005010: Situational. Required prior to the mandated HIPAA National Provider Identifier (NPI) implementation date when an identification number other than the NPI is necessary for the receiver to identify the provider. OR Required on or after the mandated NPI Implementation Date when the NPI in this field is not used and an identification number other than the NPI is necessary for the receiver to identify the provider. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 93 Form Locator 77 Field Attributes 5 Fields 2 Lines Alphanumeric Left-justified Line 1: 11 Positions* - National Provider Identifier 2 Positions - Secondary Identifier Qualifier (see below) 9 Positions - Secondary Identifier Line 2: 16 Positions - Last Name 12 Positions - First Name *Note: The NPI is ten characters in length. Secondary Identifier Qualifiers: 0B - State License Number 1G - Provider UPIN Number G2 - Provider Commercial Number Form Locator 78-79 Data Element Other Provider (Individual) Names and Identifiers Definition: The name and ID number of the individual corresponding to the Provider Type category indicated in this section of the claim. See notes below. Required Reporting Name UB-04 and 005010: Situational. See allowable provider type qualifier codes and usage notes. 004010/004010A1: Situational. Required when the claim/encounter involves another provider such as, but not limited to: Referring Provider, Ordering Provider, Assisting Provider, etc. Identifiers - National Provider Identifier The NPI Final Rule was implemented May 23, 2008. For purposes of this manual, the 004010/004010A1 National Provider Identifier and Secondary Identifier situational usage is not applicable due to the implementation of the NPI Final Rule. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 94 Form Locator 78-79 Reporting Other Operating Physician and Rendering Provider: UB-04: Situational. Required for providers in the United States or its territories when the provider is eligible to receive an NPI. OR Required for providers not in the United States or its territories when the provider has received an NPI. 005010: Situational. Required for providers in the United States or its territories on or after the mandated HIPAA NPI implementation date when the provider is eligible to receive an NPI. OR Required for providers not in the United States or its territories on or after the mandated HIPAA National Provider Identifier (NPI) implementation date when the provider has received an NPI. OR Required for providers prior to the mandated NPI implementation date when the provider has received an NPI and the submitter has the capability to send it. Referring Provider: UB-04: Required for providers when the provider has received an NPI and the NPI is available to the submitter. 005010: Required for providers on or after the mandated HIPAA National Provider Identifier (NPI) implementation date when the provider has received an NPI and the NPI is available to the submitter. OR Required for providers prior to the mandated NPI Implementation date when the provider has received an NPI and the submitter has the capability to send it. Identifiers - Secondary UB-04: Situational. Required when the NPI in this field is not used and an identification number other than the NPI is necessary for the receiver to identify the provider. 005010: Situational. Required prior to the mandated HIPAA National Provider Identifier (NPI) implementation date when an identification number other than the NPI is necessary for the receiver to identify the provider. OR Required on or after the mandated NPI Implementation Date when the NPI in this field is not used and an identification number other than the NPI is necessary for the receiver to identify the provider. Field Attributes 6 Fields 2 Lines Alphanumeric Left-justified Line 1: 2 Positions - Provider Type Qualifier (see below) 11 Positions* - National Provider Identifier 2 Positions - Secondary Identifier Qualifier (see below) 9 Positions - Secondary Identifier Line 2: 16 Positions - Last Name 12 Positions - First Name *Note: The NPI is ten characters in length. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 95 Form Locator 78-79 Notes Provider Type Qualifier Codes/Definition/Situational Usage Notes for UB-04 and 005010: DN - Referring Provider. The provider who sends the patient to another provider for services. Required on an outpatient claim when the Referring Provider is different than the Attending Physician. If not required, do not send. ZZ - Other Operating Physician. An individual performing a secondary surgical procedure or assisting the Operating Physician. Required when another Operating Physician is involved. If not required, do not send. 82 - Rendering Provider. The health care professional who delivers or completes a particular medical service or non-surgical procedure. Report when state or federal regulatory requirements call for a combined claim, i.e., a claim that includes both facility and professional fee components (e.g., a Medicaid clinic bill or Critical Access Hospital claim). If not required, do not send. Secondary Identifier Qualifiers: 0B - State License Number 1G - Provider UPIN Number G2 - Provider Commercial Number Form Locator 80 Data Element Remarks Field Definition: Area to capture additional information necessary to adjudicate the claim. Required Reporting UB-04: Situational. Required when in the judgment of the provider, the information is needed to substantiate the medical treatment and is not supported elsewhere within the claim data set. 004010/004010A1: Situational. The Billing Note segment (Loop ID 2300 | NTE) is used to convey additional information necessary to adjudicate the claim. Required when: (1) State regulations mandate information not identified elsewhere within the claim set; or (2) in the opinion of the provider, the information is needed to substantiate the medical treatment and is not supported elsewhere within the claim data set. 005010: Situational (Loop ID 2300 | NTE). Required when in the judgment of the provider, the information is needed to substantiate the medical treatment and is not supported elsewhere within the claim data set. OR Required when in the judgment of the provider, narrative information from the forms “Home Health Certification and Plan of Treatment” or “Medical Update and Patient Information” is needed to substantiate home health services. Field Attributes 1 Field 4 Lines Line 1: 19 Positions Notes The UB-04 Remarks Field is too small to accommodate addresses. Therefore, do not use this field for the patient or health plan address; FL 38 is designed for window envelopes and should be used for this purpose. BCNEPA/FPH/FPLIC Billing Manual November 2012 Alphanumeric Line 2-4: 24 Positions Left-justified Page 96 Form Locator 81 Data Element Code-Code Field Definition: To report additional codes related to a Form Locator (overflow) or to report externally maintained codes approved by the NUBC for inclusion in the institutional data set. Required Reporting Situational. See specifics below. For overflow NUBC codes (A1-A4), see applicable Form Locator. Field Attributes Middle Column Right Column Left Column 1 Field (Code Qualifier) 1 Field (Code) 1 Field (Number or Value) 4 Lines 4 Lines 4 Lines 2 Positions 10 Positions 12 Positions Alphanumeric Alphanumeric Alphanumeric Left-justified Left-justified Right-justified (fully coded) Notes Code List Qualifiers: 01-A0 Reserved for National Assignment A1 National Uniform Billing Committee Condition Codes (FL 18-28) Right Example: A 1 4 A2 National Uniform Billing Committee Occurrence Codes (FL 31-34) Example: A 2 0 A3 4 1 0 2 2 8 0 6 National Uniform Billing Committee Occurrence Span Codes (FL 35-36) All positions fully coded in the right column. Example: A A4 3 M 4 0 3 0 1 0 6 0 3 0 9 0 6 National Uniform Billing Committee Value Codes (FL 39-41) For Value Codes, there is an implied dollar/cents delimiter in the right column of FL 81 separating the last two positions as illustrated below. $ $ $ $ $ $ $ $ $ $ c c See FL 39-41 for special rules for reporting values. Whole numbers or nondollar amounts are right justified to the left of the implied dollars/cents delimiter. Do not zero fill the positions to the left of the implied delimiter. However, values are reported as cents, thus reference to the instructions for specific does is necessary. A BCNEPA/FPH/FPLIC Billing Manual November 2012 4 5 4 3 3 3 3 Page 97 Form Locator 81 Notes A5-AB Reserved for Assignment by the NUBC. AC Attachment Control Number (Effective 1/1/09) Code Source: ASC X12 Data Element 755 - Report Type Code Codes valid for use on UB-04: 04 Drugs Administered (medications) AM Ambulance Certification DS Discharge Summary LA Laboratory Results M1 Medical Record Attachment NN Nursing Notes OB Operative Notes OZ Support Data for Claim (e.g., itemized bill) PN Physical Therapy Notes RR Radiology Reports UL Other Type of Report Example: A C R R E L A C 1 2 3 4 5 6 AD-B0 Reserved for Assignment by the NUBC. B1 Standards for the Classification of Federal Data on Race and Ethnicity Code Source: ASC X12 External Code Source 859 (Centers for Disease Control and Prevention (CDC)) Reporting* FOR PUBLIC HEALTH DATA REPORTING ONLY when required by state or federal law or regulations. Example: B 1 R B2 5 E 2 Reserved for Martial Status Code Source: ASC X12 Data Element 1067 Reporting* (Effective Date to be Determined) FOR PUBLIC HEALTH DATA REPORTING ONLY when required by state or federal law or regulations. Example: B 2 M * Use of Code List Qualifiers B1 and B2 is intended to promote standardized public health reporting of these data elements. BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 98 Form Locator 81 Notes B3 Health Care Provider Taxonomy Code Code Source: ASC X12 External Code Source 682 (National Uniform Claim Committee) Reporting UB-04: Situational. Used for Billing Provider Only (FL01). Required when the payer’s adjudication is known to be impacted by the provider taxonomy code. 004010/004010A1 (Loop ID 2000A | PRV03): Situational. Required when adjudication is known to be impacted by the provider taxonomy code, and the Service Facility Provider is the same entity as the Billing and/or Pay-to Provider. 005010 (Loop ID 2000A | PRV03): Situational. Required when the payer’s adjudication is known to be impacted by the provider taxonomy code. All positions fully coded in the middle column; the right-hand column is left blank. Example: B 3 2 8 2 N 0 0 0 0 0 X B4-B6 Source of Payment Typology Code Source: Public Health Data Standards Consortium (http://www.phdsc.org/) (ASC X12 External Code Source 944) B4 = Payer A (Primary) B5 = Payer B (Secondary) B6 = Payer C (Tertiary) Reporting* (Effective Date July 1, 2009) FOR PUBLIC HEALTH DATA REPORTING ONLY when required by state or federal law or regulations. Example: B 4 1 2 1 B 5 2 *Use of Code List Qualifiers B4-B6 is intended to promote standardized Public Health Reporting of these data elements. B7 Preferred Language Spoken Code Source: ISO 639-2 Language Codes Definition: The language the patient prefers for discussing health care information with those in the health care community. Reporting (Effective Date January 1, 2011) FOR PUBLIC HEALTH DATA REPORTING ONLY when required by state or federal law or regulations. Example*: B 7 SPA *ISO 639-2 recommends use of the language codes in lower case, but they should be considered case-insensitive and are unique codes regardless of case. This examples uses upper case letters which coincides with the basic character set used in the X12 standard (Appendix B.1.1.2.2 of the implementation guides). B8-ZZ BCNEPA/FPH/FPLIC Billing Manual November 2012 Reserved for Assignment by the NUBC. Page 99 BCNEPA/FPH/FPLIC Billing Manual November 2012 Page 100