VIEKIRA XR
advertisement

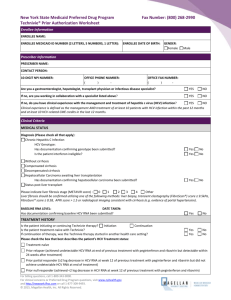
HIGHLIGHTS OF PRESCRIBING INFORMATION
These highlights do not include all the information needed to use
VIEKIRA XR safely and effectively. See full prescribing information for
VIEKIRA XR.
VIEKIRA XR (dasabuvir, ombitasvir, paritaprevir, and ritonavir)
extended-release tablets, for oral use
Initial U.S. Approval: 2014
INDICATIONS AND USAGE
VIEKIRA XR includes dasabuvir, a hepatitis C virus non-nucleoside NS5B
palm polymerase inhibitor, ombitasvir, a hepatitis C virus NS5A inhibitor,
paritaprevir, a hepatitis C virus NS3/4A protease inhibitor, and ritonavir, a
CYP3A inhibitor and is indicated for the treatment of adult patients with
chronic hepatitis C virus (HCV):
• genotype 1b infection without cirrhosis or with compensated cirrhosis
• genotype 1a infection without cirrhosis or with compensated cirrhosis for
use in combination with ribavirin. (1)
DOSAGE AND ADMINISTRATION
Testing Prior to Initiation - Assess for laboratory and clinical evidence of
hepatic decompensation. (2.1)
Recommended dosage: Three tablets taken once daily. VIEKIRA XR must be
taken with a meal because administration under fasting conditions may result
in reduced virologic response and possible development of resistance. (2.2)
Treatment Regimen and Duration by Patient Population
Patient Population
Treatment*
Duration
Genotype 1a,
VIEKIRA XR + ribavirin 12 weeks
without cirrhosis
Genotype 1a,
VIEKIRA XR + ribavirin 24 weeks**
with compensated cirrhosis
Genotype 1b,
VIEKIRA XR
12 weeks
with or without compensated
cirrhosis
*Note: Follow the genotype 1a dosing recommendations in patients with an
unknown genotype 1 subtype or with mixed genotype 1 infection.
**VIEKIRA XR administered with ribavirin for 12 weeks may be considered
for some patients based on prior treatment history [See Clinical Studies
(14.3)].
• HCV/HIV-1 co-infection: For patients with HCV/HIV-1 co-infection,
follow the dosage recommendations in the table above. (2.2)
• Liver Transplant Recipients: In liver transplant recipients with normal
hepatic function and mild fibrosis (Metavir fibrosis score ≤2), the
recommended duration of VIEKIRA XR with ribavirin is 24 weeks. (2.4)
DOSAGE FORMS AND STRENGTHS
Extended-release tablets: 200 mg dasabuvir, 8.33 mg ombitasvir, 50 mg
paritaprevir, and 33.33 mg ritonavir (3)
CONTRAINDICATIONS
• Patients with moderate to severe hepatic impairment. (4, 5.1, 8.6, 12.3)
• If VIEKIRA XR is administered with ribavirin, the contraindications to
ribavirin also apply to this combination regimen. (4)
• Co-administration with drugs that are: highly dependent on CYP3A for
clearance; moderate or strong inducers of CYP3A or strong inducers of
CYP2C8; and strong inhibitors of CYP2C8. (4)
• Known hypersensitivity to ritonavir (e.g. toxic epidermal necrolysis,
Stevens-Johnson syndrome). (4)
WARNINGS AND PRECAUTIONS
• Hepatic Decompensation and Hepatic Failure in Patient with Cirrhosis:
Hepatic decompensation and hepatic failure, including liver transplantation
or fatal outcomes, have been reported mostly in patients with advanced
cirrhosis. Monitor for clinical signs and symptoms of hepatic
decompensation. (5.1)
• ALT Elevations: Discontinue ethinyl estradiol-containing medications prior
to starting VIEKIRA XR (alternative contraceptive methods are
recommended). Perform hepatic laboratory testing on all patients during the
first 4 weeks of treatment. For ALT elevations on VIEKIRA XR, monitor
closely and follow recommendations in full prescribing information. (5.2)
• Risks Associated With Ribavirin Combination Treatment: If VIEKIRA XR
is administered with ribavirin, the warnings and precautions for ribavirin
also apply to this combination regimen. (5.3)
• Drug Interactions: The concomitant use of VIEKIRA XR and certain other
drugs may result in known or potentially significant drug interactions, some
of which may lead to loss of therapeutic effect of VIEKIRA XR. (5.4)
ADVERSE REACTIONS
In subjects receiving the combination of dasabuvir with ombitasvir,
paritaprevir, ritonavir with ribavirin, the most commonly reported adverse
reactions (greater than 10% of subjects) were fatigue, nausea, pruritus, other
skin reactions, insomnia and asthenia. In subjects receiving the combination of
dasabuvir with ombitasvir, paritaprevir, ritonavir without ribavirin, the most
commonly reported adverse reactions (greater than or equal to 5% of subjects)
were nausea, pruritus and insomnia. (6.1)
To report SUSPECTED ADVERSE REACTIONS, contact AbbVie Inc.
at 1-800-633-9110 or FDA at 1-800-FDA-1088 or www.fda.gov/medwatch.
DRUG INTERACTIONS
Co-administration of VIEKIRA XR can alter the plasma concentrations of
some drugs and some drugs may alter the plasma concentrations of VIEKIRA
XR. The potential for drug interactions must be considered before and during
treatment. Consult the full prescribing information prior to and during
treatment for potential drug interactions. (4, 5.4, 7, 12.3)
See 17 for PATIENT COUNSELING INFORMATION and Medication
Guide.
Revised: 7/2016
FULL PRESCRIBING INFORMATION: CONTENTS*
1 INDICATIONS AND USAGE
2 DOSAGE AND ADMINISTRATION
2.1 Testing Prior to Initiation of VIEKIRA XR
2.2 Recommended Dosage in Adults
2.3 Use in Liver Transplant Recipients
2.4 Hepatic Impairment
3 DOSAGE FORMS AND STRENGTHS
4 CONTRAINDICATIONS
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Hepatic Decompensation and Hepatic Failure in Patients with
Cirrhosis
5.2 Increased Risk of ALT Elevations
5.3 Risks Associated With Ribavirin Combination Treatment
5.4 Risk of Adverse Reactions or Reduced Therapeutic Effect Due to Drug
Interactions
5.5 Risk of HIV-1 Protease Inhibitor Drug Resistance in HCV/HIV-1 Coinfected Patients
6 ADVERSE REACTIONS
6.1 Clinical Trials Experience
6.2 Postmarketing Experience
7 DRUG INTERACTIONS
7.1 Potential for VIEKIRA XR to Affect Other Drugs
7.2 Potential for Other Drugs to Affect One or More Components of
VIEKIRA XR
7.3 Established and Other Potential Drug Interactions
7.4 Drugs without Clinically Significant Interactions with VIEKIRA XR
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
8.2 Lactation
8.3 Females and Males of Reproductive Potential
8.4 Pediatric Use
8.5 Geriatric Use
8.6 Hepatic Impairment
8.7 Renal Impairment
10 OVERDOSAGE
11 DESCRIPTION
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
12.2 Pharmacodynamics
12.3 Pharmacokinetics
12.4 Microbiology
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
14 CLINICAL STUDIES
14.1 Description of Clinical Trials
14.2 Clinical Trial Results in Adults with Chronic HCV Genotype 1a and 1b
Infection without Cirrhosis
14.3 Clinical Trial Results in Adults with Chronic HCV Genotype 1a and 1b
Infection and Compensated Cirrhosis
14.4 Effect of Ribavirin Dose Reductions on SVR12
14.5 Clinical Trial of Selected Liver Transplant Recipients (CORAL-I)
14.6 Clinical Trial in Subjects with HCV/HIV-1 Co-infection
(TURQUOISE-I)
14.7 Durability of Response
16 HOW SUPPLIED/STORAGE AND HANDLING
17 PATIENT COUNSELING INFORMATION
*Sections or subsections omitted from the full prescribing information are not
listed.
FULL PRESCRIBING INFORMATION
1 INDICATIONS AND USAGE
VIEKIRA XR is indicated for the treatment of adult patients with chronic hepatitis C virus
(HCV) [see Dosage and Administration (2.2) and Clinical Studies (14)]:
• genotype 1b infection without cirrhosis or with compensated cirrhosis
• genotype 1a infection without cirrhosis or with compensated cirrhosis for use in combination
with ribavirin.
2 DOSAGE AND ADMINISTRATION
2.1 Testing Prior to Initiation of VIEKIRA XR
Prior to initiation of VIEKIRA XR, assess for laboratory and clinical evidence of hepatic
decompensation [see Warnings and Precautions (5.1 and 5.2)].
2.2 Recommended Dosage in Adults
VIEKIRA XR is a 4-drug fixed-dose combination, extended-release tablet containing 200 mg of
dasabuvir, 8.33 mg of ombitasvir, 50 mg of paritaprevir, and 33.33 mg of ritonavir.
The recommended dosage of VIEKIRA XR is three tablets taken orally once daily.
• VIEKIRA XR must be taken with a meal because administration under fasting conditions
may result in reduced virologic response and possible development of resistance [see
Clinical Pharmacology (12.3)].
• Swallow tablets whole. Splitting, crushing, or chewing tablets may compromise the
extended-release performance, efficacy, and/or safety of VIEKIRA XR.
• For optimal release of dasabuvir, alcohol should not be consumed within 4 hours of taking
VIEKIRA XR.
VIEKIRA XR is used in combination with ribavirin (RBV) in certain patient populations (see
Table 1). When administered with VIEKIRA XR, the recommended dosage of RBV is based on
weight: 1000 mg/day for subjects <75 kg and 1200 mg/day for those ≥75 kg, divided and
administered twice-daily with food. The starting dosage and on-treatment dosage of RBV can be
decreased based on changes in hemoglobin levels and/or creatinine clearance. For ribavirin
dosage modifications, refer to the ribavirin prescribing information.
For patients with HCV/HIV-1 co-infection, follow the dosage recommendations in Table 1.
Refer to Drug Interactions (7) for dosage recommendations for concomitant HIV-1 antiviral
drugs.
Table 1 shows the recommended VIEKIRA XR treatment regimen and duration based on patient
population.
Table 1. Treatment Regimen and Duration by Patient Population (Treatment-Naïve or
Interferon-Experienced)
Patient Population
Treatment*
Duration
Genotype 1a,
VIEKIRA XR + ribavirin
12 weeks
without cirrhosis
Genotype 1a,
VIEKIRA XR + ribavirin
24 weeks**
with compensated cirrhosis
(Child-Pugh A)
Genotype 1b,
VIEKIRA XR
12 weeks
with or without compensated
cirrhosis (Child-Pugh A)
*Note: Follow the genotype 1a dosing recommendations in patients with an unknown genotype 1
subtype or with mixed genotype 1 infection.
**VIEKIRA XR administered with ribavirin for 12 weeks may be considered for some patients
based on prior treatment history [see Clinical Studies (14.3)].
2.3 Use in Liver Transplant Recipients
In liver transplant recipients with normal hepatic function and mild fibrosis (Metavir fibrosis
score 2 or lower), the recommended duration of VIEKIRA XR with ribavirin is 24 weeks,
irrespective of HCV genotype 1 subtype [see Clinical Studies (14.6)]. When VIEKIRA XR is
administered with calcineurin inhibitors in liver transplant recipients, dosage adjustment of
calcineurin inhibitors is needed [see Drug Interactions (7)].
2.4 Hepatic Impairment
VIEKIRA XR is contraindicated in patients with moderate to severe hepatic impairment (ChildPugh B and C) [see Contraindications (4), Warnings and Precautions (5.1), Use in Specific
Populations (8.6), and Clinical Pharmacology (12.3)].
3 DOSAGE FORMS AND STRENGTHS
Extended-release tablet: 200 mg of dasabuvir (equivalent to 216.2 mg of dasabuvir sodium
monohydrate), 8.33 mg of ombitasvir, 50 mg of paritaprevir, and 33.33 mg of ritonavir. The
tablets are pale yellow-colored, film-coated, oblong shaped, debossed with “3QD” on one side.
4 CONTRAINDICATIONS
• VIEKIRA XR is contraindicated in patients with moderate to severe hepatic impairment
(Child-Pugh B and C) due to risk of potential toxicity [see Warnings and Precautions (5.1),
Use in Specific Populations (8.6) and Clinical Pharmacology (12.3)].
• If VIEKIRA XR is administered with ribavirin, the contraindications to ribavirin also apply
to this combination regimen. Refer to the ribavirin prescribing information for a list of
contraindications for ribavirin.
• VIEKIRA XR is contraindicated:
◦ With drugs that are highly dependent on CYP3A for clearance and for which elevated
plasma concentrations are associated with serious and/or life-threatening events.
◦ With drugs that are moderate or strong inducers of CYP3A and strong inducers of
CYP2C8 and may lead to reduced efficacy of VIEKIRA XR.
◦ With drugs that are strong inhibitors of CYP2C8 and may increase dasabuvir plasma
concentrations and the risk of QT prolongation.
◦ In patients with known hypersensitivity to ritonavir (e.g. toxic epidermal necrolysis
(TEN) or Stevens-Johnson syndrome).
Table 2 lists drugs that are contraindicated with VIEKIRA XR [see Drug Interactions (7)].
Table 2. Drugs that are Contraindicated with VIEKIRA XR
Drug(s) within Class
Drug Class
that are
Clinical Comments
Contraindicated
Alpha1-adrenoreceptor Alfuzosin HCL
Potential for hypotension.
antagonist
Anti-anginal
Ranolazine
Potential for serious and/or life-threatening
reactions.
Antiarrhythmic
Dronedarone
Potential for serious and/or life-threatening
reactions such as cardiac arrhythmias.
Anticonvulsants
Carbamazepine,
VIEKIRA XR exposures may decrease leading
phenytoin,
to a potential loss of therapeutic activity of
phenobarbital
VIEKIRA XR.
Anti-gout
Colchicine
Potential for serious and/or life-threatening
reactions in patients with renal and/or hepatic
impairment.
Antihyperlipidemic
Gemfibrozil
Increase in dasabuvir exposures by 10-fold
agent
which may increase the risk of QT
prolongation.
Antimycobacterial
Rifampin
VIEKIRA XR exposures may decrease leading
to a potential loss of therapeutic activity of
VIEKIRA XR.
Antipsychotic
Lurasidone
Potential for serious and/or life-threatening
reactions.
Pimozide
Potential for serious and/or life-threatening
reactions such as cardiac arrhythmias.
Ergot derivatives
Ergotamine,
Acute ergot toxicity characterized by vasospasm
dihydroergotamine,
and tissue ischemia has been associated with comethylergonovine
administration of ritonavir and ergonovine,
ergotamine, dihydroergotamine, or
methylergonovine.
Ethinyl estradiolEthinyl estradiolPotential for ALT elevations [see Warnings and
containing products
containing medications Precautions (5.2)].
such as combined oral
contraceptives
GI Motility Agent
Cisapride
Potential for serious and/or life threatening
reactions such as cardiac arrhythmias.
Herbal Product
St. John’s Wort
VIEKIRA XR exposures may decrease leading
(Hypericum
to a potential loss of therapeutic activity of
perforatum)
VIEKIRA XR.
HMG-CoA Reductase Lovastatin,
Potential for myopathy including
Inhibitors
simvastatin
rhabdomyolysis.
Non-nucleoside reverse Efavirenz
Co-administration of efavirenz based regimens
transcriptase inhibitor
with paritaprevir, ritonavir plus dasabuvir was
poorly tolerated and resulted in liver enzyme
elevations.
Phosphodiesterase-5
Sildenafil when dosed There is increased potential for sildenafil(PDE5) inhibitor
as Revatio for the
associated adverse events such as visual
treatment of pulmonary disturbances, hypotension, priapism, and
arterial hypertension
syncope.
(PAH)
Sedatives/hypnotics
Triazolam
Triazolam and orally administered midazolam
Orally administered
are extensively metabolized by CYP3A4.
midazolam
Coadministration of triazolam or orally
administered midazolam with VIEKIRA XR
may cause large increases in the concentration
of these benzodiazepines. The potential exists
for serious and/or life threatening events such as
prolonged or increased sedation or respiratory
depression.
5 WARNINGS AND PRECAUTIONS
5.1 Risk of Hepatic Decompensation and Hepatic Failure in Patients with Cirrhosis
Hepatic decompensation and hepatic failure, including liver transplantation or fatal outcomes,
have been reported postmarketing in patients treated with the components of VIEKIRA XR.
Most patients with these severe outcomes had evidence of advanced cirrhosis prior to initiating
therapy. Reported cases typically occurred within one to four weeks of initiating therapy and
were characterized by the acute onset of rising direct serum bilirubin levels without ALT
elevations in association with clinical signs and symptoms of hepatic decompensation. Because
these events are reported voluntarily from a population of uncertain size, it is not always possible
to reliably estimate their frequency or establish a causal relationship to drug exposure.
VIEKIRA XR is contraindicated in patients with moderate to severe hepatic impairment (ChildPugh B and C) [see Contraindications (4), Adverse Reactions (6.2), Use in Specific Populations
(8.6), and Clinical Pharmacology (12.3)].
For patients with cirrhosis:
• Monitor for clinical signs and symptoms of hepatic decompensation (such as ascites, hepatic
encephalopathy, variceal hemorrhage).
• Hepatic laboratory testing including direct bilirubin levels should be performed at baseline
and during the first 4 weeks of starting treatment and as clinically indicated.
• Discontinue VIEKIRA XR in patients who develop evidence of hepatic decompensation.
5.2 Increased Risk of ALT Elevations
During clinical trials with the combination of dasabuvir tablets and ombitasvir, paritaprevir, and
ritonavir tablets (components of VIEKIRA XR) with or without ribavirin, elevations of ALT to
greater than 5 times the upper limit of normal (ULN) occurred in approximately 1% of all
subjects [see Adverse Reactions (6.1)]. ALT elevations were typically asymptomatic, occurred
during the first 4 weeks of treatment, and declined within two to eight weeks of onset with
continued dosing.
These ALT elevations were significantly more frequent in female subjects who were using
ethinyl estradiol-containing medications such as combined oral contraceptives, contraceptive
patches or contraceptive vaginal rings. Ethinyl estradiol-containing medications must be
discontinued prior to starting therapy with VIEKIRA XR [see Contraindications (4)].
Alternative methods of contraception (e.g., progestin only contraception or non-hormonal
methods) are recommended during VIEKIRA XR therapy. Ethinyl estradiol-containing
medications can be restarted approximately 2 weeks following completion of treatment with
VIEKIRA XR.
Women using estrogens other than ethinyl estradiol, such as estradiol and conjugated estrogens
used in hormone replacement therapy had a rate of ALT elevation similar to those not receiving
any estrogens; however, due to the limited number of subjects taking these other estrogens,
caution is warranted for co-administration with VIEKIRA XR [see Adverse Reactions (6.1)].
Hepatic laboratory testing should be performed during the first 4 weeks of starting treatment and
as clinically indicated thereafter. If ALT is found to be elevated above baseline levels, it should
be repeated and monitored closely:
• Patients should be instructed to consult their health care professional without delay if they
have onset of fatigue, weakness, lack of appetite, nausea and vomiting, jaundice or
discolored feces.
• Consider discontinuing VIEKIRA XR if ALT levels remain persistently greater than 10 times
the ULN.
• Discontinue VIEKIRA XR if ALT elevation is accompanied by signs or symptoms of liver
inflammation or increasing direct bilirubin, alkaline phosphatase, or INR.
5.3 Risks Associated With Ribavirin Combination Treatment
If VIEKIRA XR is administered with ribavirin, the warnings and precautions for ribavirin, in
particular the pregnancy avoidance warning, apply to this combination regimen. Refer to the
ribavirin prescribing information for a full list of the warnings and precautions for ribavirin.
5.4 Risk of Adverse Reactions or Reduced Therapeutic Effect Due to Drug Interactions
The concomitant use of VIEKIRA XR and certain other drugs may result in known or potentially
significant drug interactions, some of which may lead to:
• Loss of therapeutic effect of VIEKIRA XR and possible development of resistance
• Possible clinically significant adverse reactions from greater exposures of concomitant drugs
or components of VIEKIRA XR.
See Table 5 for steps to prevent or manage these possible and known significant drug
interactions, including dosing recommendations [see Drug Interactions (7)]. Consider the
potential for drug interactions prior to and during VIEKIRA XR therapy; review concomitant
medications during VIEKIRA XR therapy; and monitor for the adverse reactions associated with
the concomitant drugs [see Contraindications (4) and Drug Interactions (7)].
5.5 Risk of HIV-1 Protease Inhibitor Drug Resistance in HCV/HIV-1 Co-infected Patients
The ritonavir component of VIEKIRA XR is also an HIV-1 protease inhibitor and can select for
HIV-1 protease inhibitor resistance-associated substitutions. Any HCV/HIV-1 co-infected
patients treated with VIEKIRA XR should also be on a suppressive antiretroviral drug regimen
to reduce the risk of HIV-1 protease inhibitor drug resistance.
6 ADVERSE REACTIONS
The following adverse reaction is described below and elsewhere in the labeling:
• Risk of Hepatic Decompensation and Hepatic Failure in Patients with Cirrhosis [see
Warnings and Precautions (5.1)]
• Increased Risk of ALT Elevations [see Warnings and Precautions (5.2)]
6.1 Clinical Trials Experience
Because clinical trials are conducted under widely varying conditions, adverse reaction rates
observed in clinical trials of VIEKIRA XR cannot be directly compared to rates in the clinical
trials of another drug and may not reflect the rates observed in practice.
If VIEKIRA XR is administered with ribavirin (RBV), refer to the prescribing information for
ribavirin for a list of ribavirin-associated adverse reactions.
The safety assessment was based on data from seven clinical trials in more than 2,000 subjects
who received the components of VIEKIRA XR with or without ribavirin for 12 or 24 weeks.
Components of VIEKIRA XR with Ribavirin in GT 1-Infected Subjects without Cirrhosis
The safety of the components of VIEKIRA XR with ribavirin were assessed in 770 subjects with
chronic HCV genotype 1 (GT1) infection without cirrhosis in two placebo-controlled trials
(SAPPHIRE-I and -II) [see Clinical Studies (14.1, 14.2)]. Adverse reactions that occurred more
often in subjects treated with the components of VIEKIRA XR with ribavirin compared to
placebo were fatigue, nausea, pruritus, other skin reactions, insomnia, and asthenia (see Table 3).
The majority of the adverse reactions were mild in severity. Two percent of subjects experienced
a serious adverse event (SAE). The proportion of subjects who permanently discontinued
treatment due to adverse reactions was less than 1%.
Table 3. Adverse Reactions with ≥5% Greater Frequency Reported in Subjects with
Chronic HCV GT1 Infection without Cirrhosis Treated with the Components of VIEKIRA
XR with Ribavirin Compared to Placebo for 12 Weeks
SAPPHIRE-I and -II
Components of VIEKIRA XR + RBV
Placebo
12 Weeks
12 Weeks
N = 770
N = 255
%
%
Fatigue
34
26
Nausea
22
15
Pruritus*
18
7
$
Skin reactions
16
9
Insomnia
14
8
Asthenia
14
7
*Grouped term ‘pruritus’ included the preferred terms pruritus and pruritus generalized.
$
Grouped terms: rash, erythema, eczema, rash maculo-papular, rash macular, dermatitis, rash
papular, skin exfoliation, rash pruritic, rash erythematous, rash generalized, dermatitis allergic,
dermatitis contact, exfoliative rash, photosensitivity reaction, psoriasis, skin reaction, ulcer,
urticaria.
Components of VIEKIRA XR with and without Ribavirin in GT1-Infected Subjects without
Cirrhosis
The components of VIEKIRA XR with and without ribavirin were assessed in 401 and 509
subjects with chronic HCV infection GT1 infection without cirrhosis, respectively, in three
clinical trials (PEARL-II, PEARL-III and PEARL-IV) [see Clinical Studies (14.1, 14.2)].
Pruritus, nausea, insomnia, and asthenia were identified as adverse events occurring more often
in subjects treated with the components of VIEKIRA XR with ribavirin (see Table 4). The
majority of adverse events were mild to moderate in severity. The proportion of subjects who
permanently discontinued treatment due to adverse events was less than 1% for the components
of VIEKIRA XR with or without ribavirin.
Table 4. Adverse Events with ≥5% Greater Frequency Reported in Subjects with Chronic
HCV GT1 Infection without Cirrhosis Treated with the Components of VIEKIRA XR with
or without Ribavirin for 12 Weeks
PEARL-II, -III and -IV
Components of VIEKIRA XR + RBV Components of VIEKIRA XR without RBV
12 Weeks
12 Weeks
N = 401
N = 509
%
%
Nausea
16
8
Pruritus*
13
7
Insomnia
12
5
Asthenia
9
4
*Grouped term ‘pruritus’ included the preferred terms pruritus and pruritus generalized.
Components of VIEKIRA XR with Ribavirin in GT1-Infected Subjects with Compensated
Cirrhosis
The components of VIEKIRA XR with ribavirin were assessed in 380 subjects with genotype 1
infection and compensated cirrhosis who were treated with the components of VIEKIRA XR
plus ribavirin for 12 (n=208) or 24 (n=172) weeks duration (TURQUOISE-II) [see Clinical
Studies (14.1, 14.3)]. The type and severity of adverse events in subjects with compensated
cirrhosis was comparable to non-cirrhotic subjects in other phase 3 trials. Fatigue, skin reactions
and dyspnea occurred at least 5% more often in subjects treated for 24 weeks. The majority of
adverse events occurred during the first 12 weeks of dosing in both treatment arms. Most of the
adverse events were mild to moderate in severity. The proportion of subjects treated with the
components of VIEKIRA XR for 12 and 24 weeks who experienced SAEs were 6% and 5%,
respectively and 2% of subjects permanently discontinued treatment due to adverse events in
each treatment arm.
Components of VIEKIRA XR without Ribavirin in GT1b-Infected Subjects with Compensated
Cirrhosis
The components of VIEKIRA XR without ribavirin for 12 weeks was assessed in 60 subjects
with genotype 1b infection and compensated cirrhosis (TURQUOISE-III) [see Clinical Studies
(14.1, 14.3)]. The type and severity of adverse events and laboratory abnormalities in genotype
1b-infected subjects with compensated cirrhosis were comparable to subjects in other trials
without ribavirin.
Skin Reactions
In PEARL-II, -III and -IV, 7% of subjects receiving the components of VIEKIRA XR alone and
10% of subjects receiving the components of VIEKIRA XR with ribavirin reported rash-related
events. In SAPPHIRE-I and -II 16% of subjects receiving the components of VIEKIRA XR with
ribavirin and 9% of subjects receiving placebo reported skin reactions. In TURQUOISE-II, 18%
and 24% of subjects receiving the components of VIEKIRA XR with ribavirin for 12 or 24
weeks reported skin reactions. The majority of events were graded as mild in severity. There
were no serious events or severe cutaneous reactions, such as Stevens Johnson Syndrome (SJS),
toxic epidermal necrolysis (TEN), erythema multiforme (EM) or drug rash with eosinophilia and
systemic symptoms (DRESS).
Laboratory Abnormalities
Serum ALT Elevations
Approximately 1% of subjects treated with the components of VIEKIRA XR experienced
post-baseline serum ALT levels greater than 5 times the upper limit of normal (ULN) after
starting treatment. The incidence increased to 25% (4/16) among women taking a
concomitant ethinyl estradiol containing medication [see Contraindications (4) and
Warnings and Precautions (5.2)]. The incidence of clinically relevant ALT elevations among
women using estrogens other than ethinyl estradiol, such as estradiol and conjugated
estrogens used in hormone replacement therapy was 3% (2/59).
ALT elevations were typically asymptomatic, generally occurred during the first 4 weeks of
treatment (mean time 20 days, range 8-57 days) and most resolved with ongoing therapy. The
majority of these ALT elevations were assessed as drug-related liver injury. Elevations in
ALT were generally not associated with bilirubin elevations. Cirrhosis was not a risk factor
for elevated ALT [see Warnings and Precautions (5.2)].
Serum Bilirubin Elevations
Post-baseline elevations in bilirubin at least 2 x ULN were observed in 15% of subjects
receiving the components of VIEKIRA XR with ribavirin compared to 2% in those receiving
the components of VIEKIRA XR without ribavirin. These bilirubin increases were
predominately indirect and related to the inhibition of the bilirubin transporters
OATP1B1/1B3 by paritaprevir and ribavirin-induced hemolysis. Bilirubin elevations
occurred after initiation of treatment, peaked by study Week 1, and generally resolved with
ongoing therapy. Bilirubin elevations were not associated with serum ALT elevations.
Anemia/Decreased Hemoglobin
Across all Phase 3 studies, the mean change from baseline in hemoglobin levels in subjects
treated with the components of VIEKIRA XR with ribavirin was -2.4 g/dL and the mean
change in subjects treated with the components of VIEKIRA XR without ribavirin was -0.5
g/dL. Decreases in hemoglobin levels occurred early in treatment (Week 1-2) with further
reductions through Week 3. Hemoglobin values remained low during the remainder of
treatment and returned towards baseline levels by post-treatment Week 4. Less than 1% of
subjects treated with the components of VIEKIRA XR with ribavirin had hemoglobin levels
decrease to less than 8.0 g/dL during treatment. Seven percent of subjects treated with the
components of VIEKIRA XR with ribavirin underwent a ribavirin dose reduction due to a
decrease in hemoglobin levels; three subjects received a blood transfusion and five required
erythropoietin. One patient discontinued therapy due to anemia. No subjects treated with the
components of VIEKIRA XR without ribavirin had a hemoglobin level less than 10 g/dL.
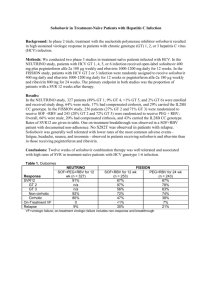
Components of VIEKIRA XR with Ribavirin in HCV/HIV-1 Co-infected Subjects
The components of VIEKIRA XR with ribavirin were assessed in 63 subjects with HCV/HIV-1
co-infection who were on stable antiretroviral therapy. The most common adverse events
occurring in at least 10% of subjects were fatigue (48%), insomnia (19%), nausea (17%),
headache (16%), pruritus (13%), cough (11%), irritability (10%), and ocular icterus (10%).
Elevations in total bilirubin greater than 2 x ULN (mostly indirect) occurred in 34 (54%)
subjects. Fifteen of these subjects were also receiving atazanavir at the time of bilirubin elevation
and nine also had adverse events of ocular icterus, jaundice or hyperbilirubinemia. None of the
subjects with hyperbilirubinemia had concomitant elevations of aminotransferases [see Warnings
and Precautions (5.5), Adverse Reactions (6.1) and Clinical Studies (14.6)]. No subject
experienced a grade 3 ALT elevation.
Seven subjects (11%) had at least one post-baseline hemoglobin value of less than 10 g/dL, and
six of these subjects had a ribavirin dose modification; no subject in this small cohort required a
blood transfusion or erythropoietin.
Median declines in CD4+ T-cell counts of 47 cells/mm3 and 62 cells/mm3 were observed at the
end of 12 and 24 weeks of treatment, respectively, and most returned to baseline levels posttreatment. Two subjects had CD4+ T-cell counts decrease to less than 200 cells/mm3 during
treatment without a decrease in CD4%. No subject experienced an AIDS-related opportunistic
infection.
Components of VIEKIRA XR with Ribavirin in Selected Liver Transplant Recipients
The components of VIEKIRA XR with ribavirin were assessed in 34 post-liver transplant
subjects with recurrent HCV infection. Adverse events occurring in more than 20% of subjects
included fatigue 50%, headache 44%, cough 32%, diarrhea 26%, insomnia 26%, asthenia 24%,
nausea 24%, muscle spasms 21% and rash 21%. Ten subjects (29%) had at least one postbaseline hemoglobin value of less than 10 g/dL. Ten subjects underwent a ribavirin dose
modification due to decrease in hemoglobin and 3% (1/34) had an interruption of ribavirin. Five
subjects received erythropoietin, all of whom initiated ribavirin at the starting dose of 1000 to
1200 mg daily. No subject received a blood transfusion [see Clinical Studies (14.5)].
6.2 Postmarketing Experience
The following adverse reactions have been identified during post approval use of the components
of VIEKIRA XR. Because these reactions are reported voluntarily from a population of uncertain
size, it is not always possible to reliably estimate their frequency or establish a causal
relationship to drug exposure.
Immune System Disorders: Hypersensitivity reactions (including angioedema).
Hepatobiliary Disorders: Hepatic decompensation, hepatic failure [see Warnings and
Precautions (5.1)].
7 DRUG INTERACTIONS
7.1 Potential for VIEKIRA XR to Affect Other Drugs
Dasabuvir, ombitasvir, and paritaprevir are inhibitors of UGT1A1, and ritonavir is an inhibitor of
CYP3A4. Paritaprevir is an inhibitor of OATP1B1 and OATP1B3 and dasabuvir, paritaprevir,
and ritonavir are inhibitors of BCRP. Co-administration of VIEKIRA XR with drugs that are
substrates of CYP3A, UGT1A1, BCRP, OATP1B1 or OATP1B3 may result in increased plasma
concentrations of such drugs [see also Contraindications (4), Warnings and Precautions (5.4),
and Clinical Pharmacology (12.3)].
7.2 Potential for Other Drugs to Affect One or More Components of VIEKIRA XR
Paritaprevir and ritonavir are primarily metabolized by CYP3A enzymes. Co-administration of
VIEKIRA XR with strong inhibitors of CYP3A may increase paritaprevir and ritonavir
concentrations. Dasabuvir is primarily metabolized by CYP2C8 enzymes. Co-administration of
VIEKIRA XR with drugs that inhibit CYP2C8 may increase dasabuvir plasma concentrations.
Ombitasvir is primarily metabolized via amide hydrolysis while CYP enzymes play a minor role
in its metabolism. Ombitasvir, paritaprevir, dasabuvir and ritonavir are substrates of P-gp.
Ombitasvir, paritaprevir and dasabuvir are substrates of BCRP. Paritaprevir is a substrate of
OATP1B1 and OATP1B3. Inhibition of P-gp, BCRP, OATP1B1 or OATP1B3 may increase the
plasma concentrations of the various components of VIEKIRA XR.
7.3 Established and Other Potential Drug Interactions
If dose adjustments of concomitant medications are made due to treatment with VIEKIRA XR,
doses should be re-adjusted after administration of VIEKIRA XR is completed. Table 5 provides
the effect of co-administration of VIEKIRA XR on concentrations of concomitant drugs and the
effect of concomitant drugs on the various components of VIEKIRA XR. Refer to
Contraindications for drugs that are contraindicated with VIEKIRA XR [see Contraindications
(4)]. Refer to the ritonavir prescribing information for other potentially significant drug
interactions with ritonavir.
Table 5. Established Drug Interactions Based on Drug Interaction Trials
Concomitant Drug Class:
Effect on
Clinical Comments
Drug Name
Concentration
ANGIOTENSIN RECEPTOR BLOCKERS
valsartan*
↑ angiotensin
Decrease the dose of the angiotensin receptor
losartan*
receptor blockers
blockers and monitor patients for signs and
*
candesartan
symptoms of hypotension and/or worsening
renal function. If such events occur, consider
further dose reduction of the angiotensin
receptor blocker or switching to an
alternative to the angiotensin receptor
blocker.
ANTIARRHYTHMICS
amiodarone*,
↑ antiarrhythmics
Contraindicated antiarrhythmics [see
bepridil*,
Contraindications (4)].
*
disopyramide ,
flecainide*,
Therapeutic concentration monitoring (if
*
lidocaine (systemic) ,
available) is recommended for
mexiletine*,
antiarrhythmics when co-administered with
*
propafenone ,
VIEKIRA XR.
quinidine*
ANTIDIABETIC DRUGS
metformin
↔ metformin
Monitor for signs of onset of lactic acidosis
such as respiratory distress, somnolence, and
non-specific abdominal distress or worsening
renal function. Concomitant metformin use in
patients with renal insufficiency or hepatic
impairment is not recommended. Refer to the
prescribing information of metformin for
further guidance.
ANTIFUNGALS
ketoconazole
↑ ketoconazole
voriconazole*
↓ voriconazole
ANTIPSYCHOTIC
quetiapine*
↑ quetiapine
When VIEKIRA XR is co-administered with
ketoconazole, the maximum daily dose of
ketoconazole should be limited to 200 mg per
day.
Co-administration of VIEKIRA XR with
voriconazole is not recommended unless an
assessment of the benefit-to-risk ratio
justifies the use of voriconazole.
Contraindicated antipsychotics [see
Contraindications (4)].
Quetiapine:
• Initiation of VIEKIRA XR in patients
taking quetiapine: Consider alternative
anti-HCV therapy to avoid increases in
quetiapine exposures. If coadministration
is necessary, reduce the quetiapine dose
to 1/6th of the current dose and monitor
for quetiapine-associated adverse
reactions. Refer to the quetiapine
prescribing information for the
recommendations on adverse reaction
monitoring.
• Initiation of quetiapine in patients taking
VIEKIRA XR: Refer to the quetiapine
prescribing information for initial dosing
and titration of quetiapine.
CALCIUM CHANNEL BLOCKERS
amlodipine
↑ calcium channel
*
nifedipine
blockers
diltiazem*
verapamil*
CORTICOSTEROIDS (INHALED/NASAL)
fluticasone*
↑ fluticasone
Decrease the dose of the calcium channel
blocker. The dose of amlodipine should be
decreased by at least 50%. Clinical
monitoring of patients is recommended for
edema and/or signs and symptoms of
hypotension. If such events occur, consider
further dose reduction of the calcium channel
blocker or switching to an alternative to the
calcium channel blocker.
Concomitant use of VIEKIRA XR with
inhaled or nasal fluticasone may reduce
serum cortisol concentrations. Alternative
corticosteroids should be considered,
particularly for long term use.
DIURETICS
furosemide
↑ furosemide (Cmax) Clinical monitoring of patients is
recommended and therapy should be
individualized based on patient’s response.
ANTIRETROVIRAL AGENTS: PROTEASE INHIBITORS
atazanavir/ritonavir
↑ paritaprevir
When coadministered with VIEKIRA XR,
once daily
atazanavir 300 mg (without ritonavir) should
only be given in the morning.
darunavir/ritonavir
↓ darunavir (Ctrough) Co-administration of VIEKIRA XR with
darunavir/ritonavir is not recommended.
lopinavir/ritonavir
↑ paritaprevir
Co-administration of VIEKIRA XR with
lopinavir/ritonavir is not recommended.
ANTIRETROVIRAL AGENTS: NON-NUCLEOSIDE REVERSE TRANSCRIPTASE
INHIBITORS
rilpivirine
↑ rilpivirine
Contraindicated non-nucleoside reverse
transcriptase inhibitors [see
Contraindications (4)].
Rilpivirine:
Co-administration of VIEKIRA XR with
rilpivirine once daily is not recommended
due to potential for QT interval prolongation
with higher concentrations of rilpivirine.
HMG CoA REDUCTASE INHIBITORS:
pravastatin
↑ pravastatin
rosuvastatin
↑ rosuvastatin
Contraindicated HMG CoA Reductase
Inhibitors [see Contraindications (4)].
Rosuvastatin:
Dose of rosuvastatin should not exceed 10
mg per day.
Pravastatin:
Dose of pravastatin should not exceed 40 mg
per day.
IMMUNOSUPPRESSANTS
cyclosporine
↑ cyclosporine
When initiating therapy with VIEKIRA XR,
reduce cyclosporine dose to 1/5th of the
patient’s current cyclosporine dose. Measure
cyclosporine blood concentrations to
determine subsequent dose modifications.
Upon completion of VIEKIRA XR therapy,
the appropriate time to resume pre-VIEKIRA
XR dose of cyclosporine should be guided by
assessment of cyclosporine blood
concentrations. Frequent assessment of renal
function and cyclosporine-related side effects
is recommended.
tacrolimus
↑ tacrolimus
When initiating therapy with VIEKIRA XR,
the dose of tacrolimus needs to be reduced.
Do not administer tacrolimus on the day
VIEKIRA XR is initiated. Beginning the day
after VIEKIRA XR is initiated; reinitiate
tacrolimus at a reduced dose based on
tacrolimus blood concentrations. Typical
tacrolimus dosing is 0.5 mg every 7 days.
Measure tacrolimus blood concentrations and
adjust dose or dosing frequency to determine
subsequent dose modifications. Upon
completion of VIEKIRA XR therapy, the
appropriate time to resume pre-VIEKIRA XR
dose of tacrolimus should be guided by
assessment of tacrolimus blood
concentrations. Frequent assessment of renal
function and tacrolimus related side effects is
recommended.
LONG ACTING BETA-ADRENOCEPTOR AGONIST
salmeterol*
↑ salmeterol
Concurrent administration of VIEKIRA XR
and salmeterol is not recommended. The
combination may result in increased risk of
cardiovascular adverse events associated with
salmeterol, including QT prolongation,
palpitations and sinus tachycardia.
MUSCLE RELAXANTS
carisoprodol
↓ carisoprodol
Increase dose if clinically indicated.
↔ mepobramate
(metabolite of
carisoprodol)
cyclobenzaprine
↓cyclobenzaprine
Increase dose if clinically indicated.
↓norcyclobenzaprine
(metabolite of
cyclobenzaprine)
NARCOTIC ANALGESICS
acetaminophen/hydrocodone ↑ hydrocodone
Reduce the dose of hydrocodone by 50% and
↔ acetaminophen
monitor patients for respiratory depression
and sedation at frequent intervals. Upon
completion of VIEKIRA XR therapy, adjust
the hydrocodone dose and monitor for signs
↑ buprenorphine
↑ norbuprenorphine
(metabolite of
buprenorphine)
PROTON PUMP INHIBITORS
omeprazole
↓ omeprazole
buprenorphine/naloxone
SEDATIVES/HYPNOTICS
alprazolam
↑ alprazolam
of opioid withdrawal.
Patients should be closely monitored for
sedation and cognitive effects.
Monitor patients for decreased efficacy of
omeprazole. Consider increasing the
omeprazole dose in patients whose symptoms
are not well controlled; avoid use of more
than 40 mg per day of omeprazole.
Contraindicated Sedatives/Hypnotics [see
Contraindications (4)].
Alprazolam:
Clinical monitoring of patients is
recommended. A decrease in alprazolam dose
can be considered based on clinical response.
Increase dose if clinically indicated.
↓ diazepam
↓ nordiazepam
(metabolite of
diazepam)
See Clinical Pharmacology, Tables 7 and 8.
The direction of the arrow indicates the direction of the change in exposures (Cmax and AUC) (↑
= increase of more than 20%, ↓ = decrease of more than 20%, ↔ = no change or change less
than 20%).
*
not studied.
diazepam
7.4 Drugs without Clinically Significant Interactions with VIEKIRA XR
No dosage adjustments are recommended when VIEKIRA XR is co-administered with the
following medications: abacavir, dolutegravir, digoxin, duloxetine, emtricitabine/tenofovir
disoproxil fumarate, escitalopram, lamivudine, methadone, progestin only contraceptives,
raltegravir, sofosbuvir, sulfamethoxazole, trimethoprim, warfarin and zolpidem.
8 USE IN SPECIFIC POPULATIONS
8.1 Pregnancy
Risk Summary
If VIEKIRA XR is administered with ribavirin, the combination regimen is contraindicated in
pregnant women and in men whose female partners are pregnant. Refer to the ribavirin
prescribing information for more information on use in pregnancy.
No adequate human data are available to establish whether or not VIEKIRA XR poses a risk to
pregnancy outcomes. In animal reproduction studies, no adverse developmental effects were
observed when the components of VIEKIRA XR were administered separately during
organogenesis and lactation. During organogenesis, the exposures were up to 28 and 4 times
(mice and rabbits, respectively; ombitasvir), 8 and 98 times (mice and rats, respectively;
paritaprevir, ritonavir), and 24 and 6 times (rats and rabbits, respectively; dasabuvir) exposures at
the recommended clinical dose of VIEKIRA XR. In rodent pre/postnatal developmental studies,
maternal systemic exposures (AUC) to ombitasvir, paritaprevir and dasabuvir were
approximately 25, 17 and 44 times, respectively, the exposure in humans at the recommended
clinical dose [see Data].
The background risk of major birth defects and miscarriage for the indicated population is
unknown. In the U.S. general population, the estimated background risk of major birth defects
and miscarriage in clinically recognized pregnancies is 2% to 4% and 15% to 20%, respectively.
Data
Animal data
Dasabuvir
Dasabuvir was administered orally to pregnant rats (0, 60, 300 and 800 mg/kg/day) and
rabbits (0, 100, 200 or 400 mg/kg/day) during the period of organogenesis (on GD 6 to 17
and GD 7 to 20, respectively). There were no test article-related embryofetal effects
(malformations or fetal toxicity) at any dose level in either species. The highest systemic
exposure of dasabuvir was 24-times higher (rats) and 6-times higher (rabbits) than the
exposures in humans at the recommended clinical dose.
In a pre- and postnatal developmental study in rats, dasabuvir was administered orally at 0,
50, 200, or 800 mg/kg/day from GD 7 to lactation day 21. There were no treatment-related
effects at maternal exposures 44-times higher than exposures in humans at the recommended
clinical dose.
Ombitasvir
Ombitasvir was administered orally to pregnant mice (0, 15, 50, or 150 mg/kg/day) and
rabbits (0, 10 or 60 mg/kg/day) during the period of organogenesis (on gestation days (GD) 6
to 15, and GD 7 to 19, respectively). There were no ombitasvir-related embryofetal effects
(malformations or fetal toxicity) at any dose level in either species. The systemic exposures
at the highest doses were 28-times higher (mice) and 4-times higher (rabbits) than the
exposures in humans at the recommended clinical dose.
In a pre- and postnatal developmental study in mice, ombitasvir was administered orally at 0,
10, 40, or 200 mg/kg/day from GD 6 to lactation day 20. There were no ombitasvir-related
effects at maternal exposures 25-times higher than exposures in humans at the recommended
clinical dose.
The major human metabolites of ombitasvir, M29 and M36, were tested in pregnant mice
during the period of organogenesis from GD 6 to 15. M29 was administered orally at doses
of 0, 1, 2.5 or 4.5 mg/kg/day. M36 was dosed orally at doses 1.5, 3, or 6 mg/kg/day. In both
cases, there were no treatment related embryofetal effects (malformations or fetal toxicity) at
any dose level. The highest doses produced exposures approximately 26-times higher than
the exposures in humans at the recommended clinical dose.
Paritaprevir/ritonavir
Paritaprevir/ritonavir was administered orally to pregnant rats (0/0, 30/15, 100/15, 450/45
mg/kg/day) and mice (0/0, 30/30, 100/30, or 300/30 mg/kg/day) during the period of
organogenesis (on GD 6 to 17, and GD 6 to 15, respectively). There were no test articlerelated embryofetal effects (malformations or fetal toxicity) at any dose level in either
species. The highest systemic exposure of paritaprevir was 8-times higher (rats) and 98-times
higher (mice) than the exposures in humans at the recommended clinical dose.
In a pre- and postnatal developmental study in rats, paritaprevir/ritonavir were administered
orally at 0/0, 6/30, 30/30, or 300/30 mg/kg/day from GD 7 to lactation day 20. There were no
treatment related effects at maternal exposures 17-times higher than exposures in humans at
the recommended clinical dose.
8.2 Lactation
Risk Summary
It is not known whether VIEKIRA XR and its metabolites are present in human breast milk,
affect human milk production or have effects on the breastfed infant. Unchanged ombitasvir,
paritaprevir and its hydrolysis product M13, and dasabuvir were the predominant components
observed in the milk of lactating rats, without effect on nursing pups [see Data].
The developmental and health benefits of breastfeeding should be considered along with the
mother’s clinical need for VIEKIRA XR and any potential adverse effects on the breastfed child
from VIEKIRA XR or from the underlying maternal condition.
If VIEKIRA XR is administered with ribavirin, the nursing mother’s information for ribavirin
also applies to this combination regimen. Refer to the ribavirin prescribing information for more
information on use during lactation.
Data
Animal Data
Dasabuvir
No effects of dasabuvir on growth and postnatal development were observed in nursing pups
at the highest dose tested (800 mg/kg/day) in rats. Maternal systemic exposure (AUC) to
dasabuvir was approximately 44 times the exposure in humans at the recommended clinical
dose. Although not measured directly, dasabuvir was likely present in the milk of lactating
rats in this study, since systemic exposure was observed in nursing pups on post-natal day 14
(approximately 14% of maternal exposure).
When dasabuvir was administered to lactating rats (5 mg/kg on post-partum day 10 to 11),
milk exposure (AUC) was 2 times higher than that in plasma, with unchanged parent drug
(78%) accounting for the majority of drug-related material in milk.
Ombitasvir
No effects of ombitasvir on growth and postnatal development were observed in nursing
pups at the highest dose tested (200 mg/kg/day) in mice. Maternal systemic exposure (AUC)
to ombitasvir was approximately 25 times the exposure in humans at the recommended
clinical dose. Although not measured directly, ombitasvir was likely present in the milk of
lactating mice in this study, since systemic exposure was observed in nursing pups on postnatal day 21 (approximately 16% of maternal exposure).
When ombitasvir was administered to lactating rats (5 mg/kg on post-partum day 10 to 11),
milk exposure (AUC) was 4 times higher than that in plasma, with unchanged parent drug
(91%) accounting for the majority of drug-related material in milk.
Paritaprevir/ritonavir
No effects of paritaprevir/ritonavir on growth and postnatal development were observed in
nursing pups at the highest dose tested (300/30 mg/kg/day) in rats. Maternal systemic
exposure (AUC) to paritaprevir was approximately 17 times the exposure in humans at the
recommended clinical dose. Although not measured directly, paritaprevir was likely present
in the milk of lactating rats at the high dose in this study, since systemic exposure was
observed in nursing pups on post-natal day 15 (approximately 0.3 % of maternal exposure).
When paritaprevir/ritonavir was administered to lactating rats (30/15 mg/kg on post-partum
day 10 to 11), milk exposure (AUC) was half that in plasma, with the hydrolysis product
M13 (84%) and unchanged parent drug (16%) accounting for all paritaprevir-related material
in milk.
8.3 Females and Males of Reproductive Potential
If VIEKIRA XR is administered with ribavirin, the information for ribavirin with regard to
pregnancy testing, contraception, and infertility also applies to this combination regimen. Refer
to ribavirin prescribing information for additional information.
8.4 Pediatric Use
Safety and effectiveness of VIEKIRA XR in pediatric patients less than 18 years of age have not
been established.
8.5 Geriatric Use
No dosage adjustment of VIEKIRA XR is warranted in geriatric patients. Of the total number of
subjects in clinical studies of the components of VIEKIRA XR, 8.5% (174/2053) were 65 and
over. No overall differences in safety or effectiveness were observed between these subjects and
younger subjects, and other reported clinical experience has not identified differences in
responses between the elderly and younger subjects, but greater sensitivity of some older
individuals cannot be ruled out.
8.6 Hepatic Impairment
No dosage adjustment of VIEKIRA XR is required in patients with mild hepatic impairment
(Child-Pugh A). VIEKIRA XR is contraindicated in patients with moderate to severe (ChildPugh B and C) hepatic impairment [see Contraindications (4), Warnings and Precautions (5.1)
and Clinical Pharmacology (12.3)].
8.7 Renal Impairment
No dosage adjustment of VIEKIRA XR is required in patients with mild, moderate or severe
renal impairment, including those on dialysis. For patients that require ribavirin, refer to the
ribavirin prescribing information for information regarding use in patients with renal impairment
[see Clinical Pharmacology (12.3)].
10 OVERDOSAGE
In case of overdose, it is recommended that the patient be monitored for any signs or symptoms
of adverse reactions and appropriate symptomatic treatment instituted immediately.
11 DESCRIPTION
VIEKIRA XR fixed dose combination, extended-release tablet includes a hepatitis C virus nonnucleoside NS5B palm polymerase inhibitor (dasabuvir), a hepatitis C virus NS5A inhibitor
(ombitasvir), a hepatitis C virus NS3/4A protease inhibitor (paritaprevir), and a CYP3A inhibitor
(ritonavir) that inhibits CYP3A mediated metabolism of paritaprevir, thereby providing
increased plasma concentration of paritaprevir. The tablets are for oral administration.
Dasabuvir
The chemical name of dasabuvir is Sodium 3-(3-tert-butyl-4-methoxy-5-{6[(methylsulfonyl)amino]naphthalene-2-yl}phenyl)-2,6-dioxo-3,6-dihydro-2H-pyrimidin-1-ide
hydrate (1:1:1). The molecular formula is C26H26N3O5S•Na•H2O (salt, hydrate) and the
molecular weight of the drug substance is 533.57 (salt, hydrate). The drug substance is white to
pale yellow to pink powder, slightly soluble in water and very slightly soluble in methanol and
isopropyl alcohol. Dasabuvir has the following molecular structure:
Ombitasvir
The chemical name of ombitasvir is Dimethyl ([(2S,5S)-1-(4-tert-butylphenyl) pyrrolidine-2,5diyl]bis{benzene-4,1-diylcarbamoyl(2S)pyrrolidine-2,1-diyl[(2S)-3-methyl-1-oxobutane-1,2diyl]})biscarbamate hydrate. The molecular formula is C50H67N7O8•4.5H2O (hydrate) and the
molecular weight for the drug substance is 975.20 (hydrate). The drug substance is white to light
yellow to light pink powder, and is practically insoluble in aqueous buffers but is soluble in
ethanol. Ombitasvir has the following molecular structure:
Paritaprevir
The chemical name of paritaprevir is (2R,6S,12Z,13aS,14aR,16aS)-N-(cyclopropylsulfonyl)-6{[(5-methylpyrazin-2-yl)carbonyl]amino}-5,16-dioxo-2-(phenanthridin-6-yloxy)1,2,3,6,7,8,9,10,11,13a,14,15,16,16a-tetradecahydrocyclopropa[e]pyrrolo[1,2-a][1,4]
diazacyclopentadecine-14a(5H)-carboxamide dihydrate. The molecular formula is
C40H43N7O7S•2H2O (dihydrate) and the molecular weight for the drug substance is 801.91
(dihydrate). The drug substance is white to off-white powder with very low water solubility.
Paritaprevir has the following molecular structure:
Ritonavir
The chemical name of ritonavir is [5S-(5R*,8R*,10R*,11R*)]10-Hydroxy-2-methyl-5-(1methyethyl)-1-[2-(1-methylethyl)-4-thiazolyl]-3,6-dioxo-8,11-bis(phenylmethyl)-2,4,7,12tetraazatridecan-13-oic acid,5-thiazolylmethyl ester. The molecular formula is C37H48N6O5S2 and
the molecular weight for the drug substance is 720.95. The drug substance is white to off white
to light tan powder practically insoluble in water and freely soluble in methanol and ethanol.
Ritonavir has the following molecular structure:
Dasabuvir, Ombitasvir, Paritaprevir, Ritonavir Film-Coated Bilayer Tablets
Dasabuvir, ombitasvir, paritaprevir, and ritonavir film-coated bilayer tablets consist of an
extended release (ER) layer and an immediate release (IR) layer. The ER layer contains 200 mg
dasabuvir (equivalent to 216.2 mg of dasabuvir sodium monohydrate). The ER layer of the tablet
also contains copovidone, K value 28, hypromellose 2208, 17,700 (mPa*s), colloidal silicon
dioxide/colloidal anhydrous silica and magnesium stearate. The IR layer contains 8.33 mg
ombitasvir, 50 mg paritaprevir and 33.33 mg ritonavir. Strength of ombitasvir and paritaprevir in
the drug product are expressed on the anhydrous basis. The IR layer of the tablet also contains
copovidone, K value 28, vitamin E polyethylene glycol succinate, propylene glycol monolaurate,
sorbitan monolaurate, colloidal silicon dioxide/colloidal anhydrous silica. The tablet coating
contains hypromellose (6 mPa*s), hypromellose (15 mPa*s), polyethylene glycol 400,
hydroxypropyl cellulose, polysorbate 80, polyethylene glycol 3350/macrogol 4000, talc, titanium
dioxide, colloidal silicon dioxide/colloidal anhydrous silica and iron oxide yellow.
12 CLINICAL PHARMACOLOGY
12.1 Mechanism of Action
VIEKIRA XR combines three direct-acting hepatitis C virus antiviral agents with distinct
mechanisms of action [see Microbiology (12.4)].
Ritonavir is not active against HCV. Ritonavir is a potent CYP3A inhibitor that increases peak
and trough plasma drug concentrations of paritaprevir and overall drug exposure (i.e., area under
the curve).
12.2 Pharmacodynamics
Cardiac Electrophysiology
The effect of a combination of ombitasvir, paritaprevir, ritonavir, and dasabuvir on QTc interval
was evaluated in a randomized, double blind, placebo and active-controlled (moxifloxacin 400
mg) 4-way crossover thorough QT study in 60 healthy subjects. At concentrations approximately
6, 1.8 and 2 times the therapeutic concentrations of paritaprevir, ombitasvir, and dasabuvir, the
combination did not prolong QTc to any clinically relevant extent.
12.3 Pharmacokinetics
Dasabuvir, ombitasvir, paritaprevir, and ritonavir film-coated bilayer tablets consist of an
extended-release (ER) layer of dasabuvir and an immediate-release (IR) layer of ombitasvir,
paritaprevir and ritonavir.
The pharmacokinetic properties of the components of VIEKIRA XR are provided in Table 6.
Table 6. Pharmacokinetic Properties of the Components of VIEKIRA XR
Ombitasvir
Paritaprevir
Ritonavir
Dasabuvir
Absorption
Tmax (hr) median values
5
5
4
8
Absolute
48
53
NA
70
bioavailability (%)
Effect of high fat meal
1.96
4.60
2.13
5.92
relative to fastinga,b
(1.83-2.15)
(3.8-5.57)
(1.86-2.43)
(5.06-6.92)
0.90- to
Accumulationc
1.5- to 2-fold
0.96-fold
1.03-fold
Distribution
% Bound to human plasma
99.9
97-98.6
>99
>99.5
proteins
Blood-to-plasma ratio
0.49
0.7
0.6
0.7
Volume of distribution
173
103
21.5d
149
at steady state (Vss) (L)
Metabolism
Metabolism
amide hydrolysis
CYP3A4
CYP3A (major),
CYP2C8
followed by
(major),
CYP2D6
(major),
oxidative
CYP3A5
CYP3A
metabolism
Eliminatione
Major route of elimination biliary excretion metabolism
metabolism
metabolism
f
t1/2 (hr)
21-25
5.5
4
5.5-6
% of dose excreted in
90.2
88
86.4
94.4
fecesg
% of dose excreted
87.8
1.1
33.8
26.2
unchanged in fecesg
% of dose excreted in
1.91
8.8
11.3
~2
urineg
% of dose excreted
0.03
0.05
3.5
0.03
unchanged in urineg
NA - data not available
a. High fat meal of 753 Kcal; 55.3% calories from fat, 27.8% calories from carbohydrates, and
16.9% calories from protein.
b. Similar results are expected for ombitasvir, paritaprevir and dasabuvir under moderate fat
meal conditions.
c. Steady state exposures are achieved after approximately 12 days of dosing.
d. It is apparent volume of distribution (V/F) for ritonavir.
e. Ombitasvir, paritaprevir, ritonavir, and dasabuvir do not inhibit organic anion transporter
(OAT1) in vivo and based on in vitro data, are not expected to inhibit organic cation
transporter (OCT2), organic anion transporter (OAT3), or multidrug and toxin extrusion
proteins (MATE1 and MATE2K) at clinically relevant concentrations.
f. t1/2 values refer to the mean elimination half-life.
g. Dosing in mass balance studies: single dose administration of [14C] ombitasvir; single dose
administration of [14C] paritaprevir co-dosed with 100 mg ritonavir; single dose
administration of [14C] dasabuvir.
Specific Populations
There are no clinically relevant changes in the pharmacokinetics of the components of VIEKIRA
XR in relation to sex, race/ethnicity, or geriatric age [see Use in Specific Populations (8.5)]. The
pharmacokinetics of VIEKIRA XR in pediatric patients less than 18 years of age have not been
established [see Use in Specific Populations (8.4)].
Hepatic Impairment
The single dose pharmacokinetics of the combination of dasabuvir, ombitasvir, paritaprevir,
and ritonavir were evaluated in non-HCV infected subjects with mild hepatic impairment
(Child-Pugh Category A; score of 5-6), moderate hepatic impairment (Child-Pugh Category
B, score of 7-9) and severe hepatic impairment (Child-Pugh Category C, score of 10-15).
Relative to subjects with normal hepatic function, dasabuvir AUC values increased by 17%,
and ombitasvir, paritaprevir and ritonavir AUC values decreased by 8%, 29% and 34%,
respectively, in subjects with mild hepatic impairment.
Relative to subjects with normal hepatic function, dasabuvir, ombitasvir, and ritonavir AUC
values decreased by 16%, 30%, and 30% respectively, and paritaprevir AUC values
increased by 62% in subjects with moderate hepatic impairment.
Relative to subjects with normal hepatic function, dasabuvir, paritaprevir, and ritonavir AUC
values increased by 325%, 945%, and 13%, respectively, and ombitasvir AUC values
decreased by 54% in subjects with severe hepatic impairment.
Renal Impairment
The single dose pharmacokinetics of the combination of dasabuvir, ombitasvir, paritaprevir,
and ritonavir were evaluated in non-HCV infected subjects with mild (CLcr: 60 to 89
mL/min), moderate (CLcr: 30 to 59 mL/min), and severe (CLcr: 15 to 29 mL/min) renal
impairment.
Pharmacokinetic data are not available on the use of VIEKIRA XR in non-HCV infected
subjects with End Stage Renal Disease (ESRD).
Relative to subjects with normal renal function, dasabuvir, paritaprevir, and ritonavir AUC
values increased by 21%, 19%, and 42% respectively, while ombitasvir AUC values were
unchanged in subjects with mild renal impairment.
Relative to subjects with normal renal function, dasabuvir, paritaprevir, and ritonavir AUC
values increased by 37%, 33%, and 80% respectively, while ombitasvir AUC values were
unchanged in subjects with moderate renal impairment.
Relative to subjects with normal renal function, dasabuvir, paritaprevir, and ritonavir AUC
values increased by 50%, 45%, and 114% respectively, while ombitasvir AUC values were
unchanged in subjects with severe renal impairment [see Use in Specific Populations (8.7)].
Drug Interaction Studies
See also Contraindications (4), Warnings and Precautions (5.4), Drug Interactions (7)
All drug-drug interaction trials were conducted with VIEKIRA PAK. The effects of some drugs
discussed in Table 5 on the exposures of dasabuvir, ombitasvir, paritaprevir, and ritonavir are
shown in Table 7. For information regarding clinical recommendations, see Drug Interactions
(7).
Table 7. Drug Interactions: Change in Pharmacokinetic Parameters of Dasabuvir,
Ombitasvir, Paritaprevir, and Ritonavir in the Presence of Co-administered Drug
CoDose of Co- n
DAA
Ratio (with/without co-administered drug)
administered administered
of DAA Pharmacokinetic Parameters
Drug (mg)
Drug
(90% CI);
No Effect = 1.00
Cmax
AUC
Cmin
Alprazolam
0.5 single 12 dasabuvir
0.93
0.98
1.00
dose
(0.83, 1.04)
(0.87, 1.11)
(0.87, 1.15)
ombitasvir
0.98
1.00
0.98
(0.93, 1.04)
(0.96, 1.04)
(0.93, 1.04)
paritaprevir
0.91
0.96
1.12
(0.64, 1.31)
(0.73, 1.27)
(1.02, 1.23)
ritonavir
0.92
0.96
1.01
(0.84, 1.02)
(0.89, 1.03)
(0.94, 1.09)
Amlodipine 5 single dose 14 dasabuvir
1.05
1.01
0.95
(0.97, 1.14)
(0.96, 1.06)
(0.89, 1.01)
ombitasvir
1.00
1.00
1.00
(0.95, 1.06)
(0.97, 1.04)
(0.97, 1.04)
paritaprevir
0.77
0.78
0.88
(0.64, 0.94)
(0.68, 0.88)
(0.80, 0.95)
ritonavir
0.96
0.93
0.95
(0.87, 1.06)
(0.89, 0.98)
(0.89, 1.01)
Atazanavir/
Atazanavir 11 dasabuvir
0.81
0.81
0.80
ritonavira
300
(0.73, 0.91)
(0.71, 0.92)
(0.65, 0.98)
and ritonavir
100
once daily in
the evening
ombitasvir
paritaprevir
ritonavir
Carbamazepine
200 once 12 dasabuvir
daily
followed by
ombitasvir
200 twice
daily
paritaprevir
ritonavir
Carisoprodol
250 single 14
dose
dasabuvir
ombitasvir
paritaprevir
ritonavir
Cyclobenzaprine 5 single dose 14
dasabuvir
ombitasvir
paritaprevir
ritonavir
Cyclosporine
30 single
doseb
10
dasabuvir
ombitasvir
paritaprevir
ritonavir
Darunavirc
800 once
daily
9
dasabuvir
ombitasvir
paritaprevir
0.83
(0.72, 0.96)
2.19
(1.61, 2.98)
1.60
(1.38, 1.86)
0.45
(0.41, 0.50)
0.69
(0.61, 0.78)
0.34
(0.25, 0.48)
0.17
(0.12, 0.24)
0.96
(0.91, 1.01)
0.98
(0.92, 1.04)
0.88
(0.75, 1.03)
0.94
(0.87, 1.02)
0.98
(0.90, 1.07)
0.98
(0.92, 1.04)
1.14
(0.99, 1.32)
0.93
(0.87, 0.99)
0.66
(0.58, 0.75)
0.99
(0.92, 1.07)
1.44
(1.16, 1.78)
0.90
(0.78, 1.04)
1.10
(0.88, 1.37)
0.86
(0.77, 0.95)
1.54
0.90
(0.78, 1.02)
3.16
(2.40, 4.17)
3.18
(2.74, 3.69)
0.30
(0.28, 0.33)
0.69
(0.64, 0.74)
0.30
(0.23, 0.38)
0.13
(0.09, 0.17)
1.02
(0.97, 1.07)
0.95
(0.92, 0.97)
0.96
(0.85, 1.08)
0.94
(0.88, 0.99)
1.01
(0.96, 1.06)
1.00
(0.97, 1.03)
1.13
(1.00, 1.28)
1.00
(0.95, 1.06)
0.70
(0.65, 0.76)
1.08
(1.05, 1.11)
1.72
(1.49, 1.99)
1.11
(1.04, 1.19)
0.94
(0.78, 1.14)
0.86
(0.79, 0.94)
1.29
1.00
(0.89, 1.13)
11.95
(8.94, 15.98)
24.65
(18.64, 32.60)
NA
NA
NA
NA
1.00
(0.92, 1.10)
0.96
(0.92, 0.99)
1.14
(1.02, 1.27)
0.95
(0.89, 1.03)
1.13
(1.07, 1.18)
1.01
(0.98, 1.04)
1.13
(1.01, 1.25)
1.13
(1.05, 1.21)
0.76
(0.71, 0.82)
1.15
(1.08, 1.23)
1.85
(1.58, 2.18)
1.49
(1.28, 1.74)
0.90
(0.76, 1.06)
0.87
(0.82, 0.92)
1.30
ritonavir
Darunavir/
ritonavird
Darunavir 7 dasabuvir
600 twice
daily and
ombitasvir
ritonavir 100
once daily
paritaprevir
in the
evening
ritonavir
Darunavir/
ritonavire
Darunavir 12 dasabuvir
800 and
ritonavir 100
ombitasvir
once daily in
the
paritaprevir
evening
ritonavir
Diazepam
2 single dose 13
dasabuvir
ombitasvir
paritaprevir
ritonavir
Ethinyl
estradiol/
Norgestimate
Ethinyl
7f dasabuvir
estradiol
0.035 and
ombitasvir
Norgestimate
0.25 once
paritaprevir
daily
ritonavir
Furosemide
20 single
dose
12
dasabuvir
ombitasvir
paritaprevir
ritonavir
(1.14, 2.09)
0.84
(0.72, 0.98)
0.84
(0.67, 1.05)
0.76
(0.65, 0.88)
0.70
(0.43, 1.12)
1.61
(1.30, 2.00)
0.75
(0.64, 0.88)
0.87
(0.82, 0.93)
0.70
(0.50, 0.99)
1.19
(1.06, 1.33)
1.05
(0.98, 1.13)
1.00
(0.93, 1.08)
0.95
(0.77, 1.18)
1.10
(1.02, 1.19)
0.51
(0.22, 1.18)
1.05
(0.81, 1.35)
0.70
(0.40, 1.21)
0.80
(0.53, 1.21)
1.12
(0.96, 1.31)
1.14
(1.03, 1.26)
0.93
(0.63, 1.36)
1.10
(0.96, 1.27)
(1.04, 1.61)
0.85
(0.78, 0.93)
0.73
(0.62, 0.86)
0.73
(0.66, 0.80)
0.59
(0.44, 0.79)
1.28
(1.12, 1.45)
0.72
(0.64, 0.82)
0.87
(0.81, 0.93)
0.81
(0.60, 1.09)
1.70
(1.54, 1.88)
1.01
(0.94, 1.08)
0.98
(0.93, 1.03)
0.91
(0.78, 1.07)
1.06
(0.98, 1.14)
0.48
(0.23, 1.02)
0.97
(0.81, 1.15)
0.66
(0.42, 1.04)
0.71
(0.54, 0.94)
1.09
(0.96, 1.23)
1.07
(1.01, 1.12)
0.92
(0.70, 1.21)
1.04
(0.92, 1.18)
(1.09, 1.54)
1.07
(0.93, 1.23)
0.54
(0.49, 0.61)
0.73
(0.64, 0.83)
0.83
(0.69, 1.01)
0.88
(0.79, 0.99)
0.65
(0.58, 0.72)
0.87
(0.80, 0.95)
1.59
(1.23, 2.05)
14.15
(11.66, 17.18)
1.05
(0.98, 1.12)
0.93
(0.88, 0.98)
0.92
(0.82, 1.03)
0.98
(0.92, 1.03)
0.53
(0.30, 0.95)
1.00
(0.88, 1.12)
0.87
(0.67, 1.14)
0.79
(0.68, 0.93)
1.06
(0.98, 1.14)
1.12
(1.08, 1.16)
1.26
(1.16, 1.38)
1.07
(0.99, 1.17)
Gemfibrozilg
600 twice
daily
11
dasabuvir
ombitasvir
paritaprevir
ritonavir
Hydrocodone/ 5/300 single 15
Acetaminophen
dose
dasabuvir
ombitasvir
paritaprevir
ritonavir
Ketoconazole
400 once
daily
12
dasabuvir
ombitasvir
paritaprevir
ritonavir
Lopinavir/
ritonavir
400/100
twice daily
6
dasabuvir
ombitasvir
paritaprevir
ritonavir
Lopinavir/
ritonavirh
800/200 once 12
daily
dasabuvir
ombitasvir
paritaprevir
ritonavir
Omeprazole
40 once daily 11
dasabuvir
ombitasvir
2.01
(1.71, 2.38)
NA
1.21
(0.94, 1.57)
0.84
(0.69, 1.03)
1.13
(1.01, 1.26)
1.01
(0.93, 1.10)
1.01
(0.80, 1.27)
1.01
(0.90, 1.13)
1.16
(1.03, 1.32)
0.98
(0.90, 1.06)
1.37
(1.11, 1.69)
1.27
(1.04, 1.56)
0.99
(0.75, 1.31)
1.14
(1.01, 1.28)
2.04
(1.30, 3.20)
1.55
(1.16, 2.09)
0.56
(0.47, 0.66)
0.87
(0.83, 0.92)
0.99
(0.79, 1.25)
1.57
(1.34, 1.83)
1.13
(1.03, 1.25)
1.02
(0.95, 1.09)
11.25
(9.05, 13.99)
NA
1.38
(1.18, 1.61)
0.90
(0.78, 1.04)
1.12
(1.05, 1.19)
0.97
(0.93, 1.02)
1.03
(0.89, 1.18)
1.03
(0.96, 1.09)
1.42
(1.26, 1.59)
1.17
(1.11, 1.24)
1.98
(1.63, 2.42)
1.57
(1.36, 1.81)
0.93
(0.75, 1.15)
1.17
(1.07, 1.28)
2.17
(1.63, 2.89)
2.05
(1.49, 2.81)
0.54
(0.46, 0.65)
0.97
(0.94, 1.02)
1.87
(1.40, 2.52)
2.62
(2.32, 2.97)
1.08
(0.98, 1.20)
1.05
(0.98, 1.12)
NA
NA
NA
NA
1.16
(1.08, 1.25)
0.93
(0.90, 0.97)
1.10
(0.97, 1.26)
1.01
(0.93, 1.10)
NA
NA
NA
NA
0.68
(0.57, 0.80)
1.24
(1.14, 1.34)
2.36
(1.00, 5.55)
5.25
(3.33, 8.28)
0.47
(0.39, 0.58)
1.11
(1.06, 1.16)
8.23
(5.18, 13.07)
19.46
(15.93, 23.77)
1.05
(0.93, 1.19)
1.04
(0.98, 1.11)
paritaprevir
ritonavir
Pravastatin
10 once daily 12
dasabuvir
ombitasvir
paritaprevir
ritonavir
Rilpivirine
25 once daily 10
(morning)i
dasabuvir
ombitasvir
paritaprevir
ritonavir
Rosuvastatin
5 once daily 11
dasabuvir
ombitasvir
paritaprevir
ritonavir
Tacrolimus
2 single dose 12
dasabuvir
ombitasvir
paritaprevir
ritonavir
1.19
(1.04, 1.36)
1.04
(0.96, 1.12)
1.00
(0.87, 1.14)
0.95
(0.89, 1.02)
0.96
(0.69, 1.32)
0.89
(0.73, 1.09)
1.18
(1.02, 1.37)
1.11
(1.02, 1.20)
1.30
(0.94, 1.81)
1.10
(0.98, 1.24)
1.07
(0.92, 1.24)
0.92
(0.82, 1.04)
1.59
(1.13, 2.23)
0.98
(0.84, 1.15)
0.85
(0.73, 0.98)
0.93
(0.88, 0.99)
0.57
(0.42, 0.78)
0.76
(0.63, 0.91)
1.18
(1.03, 1.37)
1.02
(0.97, 1.08)
0.96
(0.85, 1.09)
0.94
(0.89, 0.99)
1.13
(0.92, 1.38)
0.95
(0.86, 1.05)
1.17
(0.99, 1.38)
1.09
(1.04, 1.14)
1.23
(0.93, 1.64)
1.08
(0.93, 1.27)
1.08
(0.92, 1.26)
0.89
(0.83, 0.95)
1.52
(1.23, 1.90)
1.02
(0.93, 1.12)
0.90
(0.80, 1.02)
0.94
(0.89, 0.98)
0.66
(0.54, 0.81)
0.87
(0.79, 0.97)
0.92
(0.76, 1.12)
0.97
(0.89, 1.05)
1.03
(0.91, 1.15)
0.94
(0.89, 0.99)
1.39
(1.21, 1.59)
1.08
(0.98, 1.19)
1.10
(0.89, 1.37)
1.05
(1.01, 1.08)
0.95
(0.84, 1.07)
0.97
(0.91, 1.04)
1.15
(1.05, 1.25)
0.88
(0.83, 0.94)
1.43
(1.22, 1.68)
1.00
(0.90, 1.12)
1.01
(0.91, 1.11)
0.94
(0.91, 0.96)
0.73
(0.66, 0.80)
1.03
(0.89, 1.19)
a. Atazanavir plus 100 mg ritonavir administered in the evening, 12 hours after morning dose of
the components of VIEKIRA XR.
b. 30 mg cyclosporine was administered with the components of VIEKIRA XR in the test arm
and 100 mg cyclosporine was administered in the reference arm without the components of
VIEKIRA XR.
c. Darunavir administered with the components of VIEKIRA XR in the morning was compared
to darunavir administered with 100 mg ritonavir in the morning.
d. Darunavir administered with the components of VIEKIRA XR in the morning and with 100
mg ritonavir in the evening was compared to darunavir administered with 100 mg ritonavir in
the morning and evening.
e. Darunavir plus 100 mg ritonavir administered in the evening, 12 hours after the morning
dose of the components of VIEKIRA XR compared to darunavir administered with 100 mg
ritonavir in the evening.
f. N=3 for dasabuvir.
g. Study was conducted with paritaprevir, ritonavir and dasabuvir.
h. Lopinavir/ritonavir administered in the evening, 12 hours after morning dose of the
components of VIEKIRA XR.
i. Similar increases were observed when rilpivirine was dosed in the evening with food or 4
hours after food.
NA: not available/not applicable; DAA: Direct-acting antiviral agent; CI: Confidence interval
Doses of dasabuvir were 250 mg or 400 mg (both doses showed similar exposures). Doses of
ombitasvir, paritaprevir, and ritonavir were 25 mg, 150 mg and 100 mg.
Dasabuvir was dosed twice daily and ombitasvir, paritaprevir and ritonavir were dosed once
daily in all the above studies except studies with gemfibrozil, ketoconazole and carbamazepine
that used single doses.
Table 8 summarizes the effects of dasabuvir, ombitasvir, paritaprevir, and ritonavir on the
pharmacokinetics of co-administered drugs which showed clinically relevant changes. For
information regarding clinical recommendations, see Drug Interactions (7).
Table 8. Drug Interactions: Change in Pharmacokinetic Parameters for Co-administered
Drug in the Presence of VIEKIRA XR
Co-administered
Dose of Con Ratio (with/without the Components
Drug
administered
of VIEKIRA XR) of Co-administered
Drug (mg)
Drug Pharmacokinetic Parameters
(90% CI); No Effect = 1.00
Cmax
AUC
Cmin
Alprazolam
0.5 single dose
12
1.09
1.34
NA
(1.03, 1.15) (1.15, 1.55)
Amlodipine
5 single dose
14
1.26
2.57
NA
(1.11, 1.44) (2.31, 2.86)
Atazanavir/
Atazanavir 300
12
1.02
1.19
1.68
ritonavira
and ritonavir
(0.92,
(1.11, 1.28)b (1.44, 1.95)b
100 once daily
1.13)b
in the evening
Buprenorphine
Buprenorphine:
10
2.18
2.07
3.12
c
c
4 to 24 once
(1.78, 2.68) (1.78, 2.40) (2.29, 4.27)c
daily and
Norbuprenorphine
2.07
1.84
2.10
Naloxone 1 to
(1.42, 3.01)c (1.30, 2.60)c (1.49, 2.97)c
6 once daily
Naloxone
1.18
1.28
NA
(0.81, 1.73) (0.92, 1.79)c
Carbamazepine
Carbamazepine’s
metabolite,
carbamazepine10,11-epoxide
(CBZE)
Carisoprodol
Carisoprodol's
metabolite,
mepobramate
Cyclobenzaprine
200 once daily
followed by
200 twice daily
12
1.10
1.17
(1.07, 1.14) (1.13, 1.22)
0.84
0.75
(0.82, 0.87) (0.73, 0.77)
1.35
(1.27, 1.45)
0.57
(0.54, 0.61)
250 single dose
14
0.54
0.62
(0.47, 0.63) (0.55, 0.70)
1.17
1.09
(1.10, 1.25) (1.03, 1.16)
NA
0.68
0.60
(0.61, 0.75) (0.53, 0.68)
1.03
0.74
(0.87, 1.23) (0.64, 0.85)
NA
1.01
5.82
(0.85, 1.20)c (4.73, 7.14)c
5 single dose
14
Cyclobenzaprine's
metabolite,
norcyclobenzaprine
Cyclosporine
30 single dosed
10
Darunavire
800 once daily
8
Darunavir/
ritonavirf
Darunavir 600
twice daily and
ritonavir 100
once daily in
the evening
Darunavir 800
and ritonavir
100 once daily
in the evening
2 single dose
7
Darunavir/
ritonavirg
Diazepam
Diazepam's
metabolite,
nordiazepam
Ethinyl Estradiol
Norelgestromin
Ethinyl
estradiol 0.035
and Norgestimate
0.25 once daily
Norgestrel
Furosemide
20 single dose
10
13
8
NA
NA
0.92
(0.87,
0.98)b
0.87
(0.79,
0.96)b
0.76
(0.71, 0.82)b
15.80
(13.81,
18.09)c
0.52
(0.47, 0.58)b
0.80
(0.74, 0.86)b
0.57
(0.48, 0.67)b
0.79
(0.70,
0.90)b
1.34
(1.25, 1.43)b
0.54
(0.48, 0.62)b
1.18
0.78
(1.07, 1.30) (0.73, 0.82)
1.10
0.56
(1.03, 1.19) (0.45, 0.70)
1.16
1.06
(0.90, 1.50) (0.96, 1.17)
9
2.01
2.60
(1.77, 2.29) (2.30, 2.95)
9
2.26
2.54
(1.91, 2.67) (2.09, 3.09)
12
1.42
1.08
NA
NA
1.12
(0.94, 1.33)
3.11
(2.51, 3.85)
2.93
(2.39, 3.57)
NA
Hydrocodone
5 single dose
15
Ketoconazole
400 once daily
12
Lopinavir/
ritonavir
400/100
twice daily
6
Lopinavir/
ritonavirh
800/200
once daily
12
Omeprazole
40 once daily
11
Pravastatin
10 once daily
12
Rilpivirine
8
Rosuvastatin
25 once daily
(morning)i
5 once daily
11
Tacrolimus
2 single dose
12
(1.17, 1.72)
1.27
(1.14, 1.40)
1.15
(1.09, 1.21)
0.87
(0.76,
0.99)b
0.86
(0.80,
0.93)b
0.62
(0.48, 0.80)
1.37
(1.11, 1.69)
2.55
(2.08, 3.12)
7.13
(5.11, 9.96)
3.99
(3.21, 4.97)c
(1.00, 1.17)
1.90
(1.72, 2.10)
2.17
(2.05, 2.29)
0.94
(0.81, 1.10)b
0.94
(0.87, 1.01)b
0.62
(0.51, 0.75)
1.82
(1.60, 2.08)
3.25
(2.80, 3.77)
2.59
(2.09, 3.21)
57.13
(45.53,
71.69)c
NA
NA
1.15
(0.93, 1.42)b
3.18
(2.49, 4.06)b
NA
NA
3.62
(3.12, 4.21)
0.59
(0.51, 0.69)
16.56
(12.97,
21.16)c
a. Atazanavir plus 100 mg ritonavir administered in the evening, 12 hours after morning dose of
the components of VIEKIRA XR.
b. Atazanavir or darunavir or lopinavir parameters are reported.
c. Dose normalized parameters reported.
d. 30 mg cyclosporine was administered with the components of VIEKIRA XR in the test arm
and 100 mg cyclosporine was administered in the reference arm without the components of
VIEKIRA XR.
e. Darunavir administered with the components of VIEKIRA XR in the morning was compared
to darunavir administered with 100 mg ritonavir in the morning.
f. Darunavir administered with the components of VIEKIRA XR in the morning and with 100
mg ritonavir in the evening was compared to darunavir administered with 100 mg ritonavir in
the morning and evening.
g. Darunavir plus 100 mg ritonavir administered in the evening, 12 hours after morning dose of
the components of VIEKIRA XR compared to darunavir administered with 100 mg ritonavir
in the evening.
h. Lopinavir/ritonavir administered in the evening, 12 hours after morning dose of the
components of VIEKIRA XR.
i. Similar increases were observed when rilpivirine was dosed in the evening with food or 4
hours after food.
NA: not available/not applicable; CI: Confidence interval
Doses of dasabuvir were 250 mg or 400 mg (both doses showed similar exposures). Doses of
ombitasvir, paritaprevir, and ritonavir were 25 mg, 150 mg and 100 mg.
Dasabuvir was dosed twice daily and ombitasvir, paritaprevir and ritonavir were dosed once
daily in all the above studies except studies with ketoconazole and carbamazepine that used
single doses.
12.4 Microbiology
Mechanism of Action
VIEKIRA XR combines three direct-acting antiviral agents with distinct mechanisms of action
and non-overlapping resistance profiles to target HCV at multiple steps in the viral lifecycle.
Dasabuvir
Dasabuvir is a non-nucleoside inhibitor of the HCV RNA-dependent RNA polymerase
encoded by the NS5B gene, which is essential for replication of the viral genome. In a
biochemical assay, dasabuvir inhibited a panel of genotype 1a and 1b NS5B polymerases
with median IC50 values of 2.8 nM (range 2.4 nM to 4.2 nM; n = 3) and 3.7 nM (range 2.2
nM to 10.7 nM; n = 4), respectively. Based on drug resistance mapping studies of HCV
genotypes 1a and 1b, dasabuvir targets the palm domain of the NS5B polymerase, and is
therefore referred to as a non-nucleoside NS5B-palm polymerase inhibitor.
Ombitasvir
Ombitasvir is an inhibitor of HCV NS5A, which is essential for viral RNA replication and
virion assembly. The mechanism of action of ombitasvir has been characterized based on cell
culture antiviral activity and drug resistance mapping studies.
Paritaprevir
Paritaprevir is an inhibitor of the HCV NS3/4A protease which is necessary for the
proteolytic cleavage of the HCV encoded polyprotein (into mature forms of the NS3, NS4A,
NS4B, NS5A, and NS5B proteins) and is essential for viral replication. In a biochemical
assay, paritaprevir inhibited the proteolytic activity of recombinant HCV genotype 1a and 1b
NS3/4A protease enzymes with IC50 values of 0.18 nM and 0.43 nM, respectively.
Antiviral Activity
Dasabuvir
The EC50 values of dasabuvir against genotype 1a-H77 and 1b-Con1 strains in HCV replicon
cell culture assays were 7.7 nM and 1.8 nM, respectively. The median EC50 values of
dasabuvir against HCV replicons containing NS5B genes from a panel of genotype 1a and 1b
isolates from treatment-naïve subjects were 0.6 nM (range 0.4 nM to 2.1 nM; n = 11) and 0.3
nM (range 0.2 nM to 2 nM; n = 10), respectively.
Ombitasvir
The EC50 values of ombitasvir against genotype 1a-H77 and 1b-Con1 strains in HCV
replicon cell culture assays were 14.1 pM and 5 pM, respectively. The median EC50 values of
ombitasvir against HCV replicons containing NS5A genes from a panel of genotype 1a and
1b isolates from treatment-naïve subjects were 0.68 pM (range 0.35 to 0.88 pM; n = 11) and
0.94 pM (range 0.74 to 1.5 pM; n = 11), respectively.
Paritaprevir
The EC50 values of paritaprevir against genotype 1a-H77 and 1b-Con1 strains in the HCV
replicon cell culture assay were 1.0 nM and 0.21 nM, respectively. The median EC50 values
of paritaprevir against HCV replicons containing NS3 genes from a panel of genotype 1a and
1b isolates from treatment-naïve subjects were 0.68 nM (range 0.43 nM to 1.87 nM; n = 11)
and 0.06 nM (range 0.03 nM to 0.09 nM; n = 9), respectively.
Ritonavir
In HCV replicon cell culture assays, ritonavir did not exhibit a direct antiviral effect and the
presence of ritonavir did not affect the antiviral activity of paritaprevir.
Combination Antiviral Activity
Evaluation of pairwise combinations of ombitasvir, paritaprevir, dasabuvir and ribavirin in HCV
genotype 1 replicon cell culture assays showed no evidence of antagonism in antiviral activity.
Resistance
In Cell Culture
Exposure of HCV genotype 1a and 1b replicons to ombitasvir, paritaprevir or dasabuvir
resulted in the emergence of drug resistant replicons carrying amino acid substitutions in
NS5A, NS3, or NS5B, respectively. Amino acid substitutions in NS5A, NS3, or NS5B
selected in cell culture or identified in Phase 2b and 3 clinical trials were phenotypically
characterized in genotype 1a or 1b replicons.
For dasabuvir, in HCV genotype 1a replicons single NS5B substitutions C316Y, M414I/T,
E446K/Q, Y448C/H, A553T, G554S, S556G/R, and Y561H reduced dasabuvir antiviral
activity by 8- to 1,472-fold. In genotype 1b replicons, single NS5B substitutions C316H/N/Y,
S368T, N411S, M414I/T, Y448C/H, A553V, S556G and D559G reduced dasabuvir antiviral
activity by 5- to 1,569-fold.
For ombitasvir, in HCV genotype 1a replicons single NS5A substitutions M28T/V, Q30E/R,
L31V, H58D, and Y93C/H/L/N reduced ombitasvir antiviral activity by 58- to 67,000-fold.
In genotype 1b replicons, single NS5A substitutions L28T, L31F/V, and Y93H reduced
ombitasvir antiviral activity by 8- to 661-fold. In general, combinations of ombitasvir
resistance-associated substitutions in HCV genotype 1a or 1b replicons further reduced
ombitasvir antiviral activity.
For paritaprevir, in HCV genotype 1a replicons single NS3 substitutions F43L, R155G/K/S,
A156T, and D168A/E/F/H/N/V/Y reduced paritaprevir antiviral activity by 7- to 219-fold.
An NS3 Q80K substitution in a genotype 1a replicon reduced paritaprevir antiviral activity
by 3-fold. Combinations of V36M, Y56H, or E357K with R155K or D168 substitutions
reduced the activity of paritaprevir by an additional 2- to 7-fold relative to the single R155K
or D168 substitutions in genotype 1a replicons. In genotype 1b replicons single NS3
substitutions A156T and D168A/H/V reduced paritaprevir antiviral activity by 7- to 159-fold.
The combination of Y56H with D168 substitutions reduced the activity of paritaprevir by an
additional 16- to 26-fold relative to the single D168 substitutions in genotype 1b replicons.
In Clinical Studies
In a pooled analysis of subjects treated with regimens containing dasabuvir, ombitasvir,
paritaprevir, and ritonavir with or without ribavirin (for 12 or 24 weeks) in Phase 2b and
Phase 3 clinical trials, resistance analyses were conducted for 64 subjects who experienced
virologic failure (20 with on-treatment virologic failure, 44 with post-treatment relapse).
Treatment-emergent substitutions observed in the viral populations of these subjects are
shown in Table 9. Treatment-emergent substitutions were detected in all 3 HCV drug targets
in 30/57 (53%) HCV genotype 1a infected subjects, and 1/6 (17%) HCV genotype 1b
infected subjects.
Table 9. Treatment-Emergent Amino Acid Substitutions in the Pooled Analysis of the
Components of VIEKIRA XR with and without Ribavirin Regimens (12- or 24-week
durations) in Phase 2b and Phase 3 Clinical Trials
Genotype 1a Genotype 1b
N = 58a
N=6
Target
Emergent Amino Acid Substitutions
% (n)
% (n)
NS3
Any of the following NS3 substitutions: V36A/M/T,
F43L, V55I, Y56H, Q80L, I132V, R155K, A156G,
88 (51)
67 (4)
D168(any), P334S, S342P, E357K, V406A/I, T449I,
P470S, V23A (NS4A)
V36A/M/Tb
7 (4)
-b
V55I
7 (4)
-b
Y56H
10 (6)
50 (3)
b
I132V
7 (4)
-R155K
16 (9)
-d
D168 (any)
72 (42)
67 (4)
D168V
59 (34)
50 (3)
b,c
P334S
7 (4)
-b,c
E357K
5 (3)
17 (1)
b,c
V406A/I
5 (3)
-b,c
T449I
5 (3)
-b,c
P470S
5 (3)
-b
NS4A V23A
-17 (1)
b
b
b,c
F43L , Q80L , A156G, S342P
<5%
-NS5A
Any of the following NS5A substitutions: K24R,
M28A/T/V, Q30E/K/R, H/Q54Y, H58D/P/R,
78 (45)
33 (2)
Y93C/H/N
K24R
5 (3)
-M28A/T/V
33 (19)
-Q30E/K/R
47 (27)
-H/Q54Y
-17 (1)
H58D/P/R
7 (4)
-Y93C/N
5 (3)
--
NS5B
Y93H
Any of the following NS5B substitutions: G307R,
C316Y, M414I/T, E446K/Q, A450V, A553I/T/V,
G554S, S556G/R, G558R, D559G/I/N/V, Y561H
C316Y
M414I
M414T
A553I/T/V
S556G/R
D559G/I/N/V
Y561H
G307R, E446K/Q, A450V, G554S, G558R
--
33 (2)
67 (38)
33 (2)
4 (2)
-5 (3)
7 (4)
39 (22)
7 (4)
5 (3)
<5%
17 (1)
17 (1)
17 (1)
-17 (1)
----
a. N = 57 for the NS5B target.
b. Substitutions were observed in combination with other emergent substitutions at NS3
position R155 or D168.
c. Position located in NS3 helicase domain.
d. D168A/F/H/I/L/N/T/V/Y.
Persistence of Resistance-Associated Substitutions
The persistence of dasabuvir, ombitasvir, and paritaprevir treatment-emergent amino acid
substitutions in NS5B, NS5A, and NS3, respectively, was assessed in HCV genotype 1a-infected
subjects in Phase 2 trials whose virus had at least 1 treatment-emergent resistance-associated
substitution in the drug target, and with available data through at least 24 weeks post-treatment.
Population and clonal nucleotide sequence analyses (assay sensitivity approximately 5-10%)
were conducted to detect the persistence of viral populations with treatment-emergent
substitutions.
For dasabuvir, viral populations with 1 or more treatment-emergent substitutions in NS5B
persisted at detectable levels through at least Post-Treatment Week 24 in 11/16 (69%) subjects,
and through Post-Treatment Week 48 in 8/15 (53%) subjects with available data. Treatmentemergent S556G persisted through Post-Treatment Week 48 in 6/9 (67%) subjects.
For ombitasvir, viral populations with 1 or more resistance-associated treatment-emergent
substitutions in NS5A persisted at detectable levels through at least Post-Treatment Week 24 in
24/24 (100%) subjects, and through Post-Treatment Week 48 in 18/18 (100%) subjects with
available data.
For paritaprevir, viral populations with 1 or more treatment-emergent substitutions in NS3
persisted at detectable levels through at least Post-Treatment Week 24 in 17/29 (59%) subjects,
and through Post-Treatment Week 48 in 5/22 (23%) subjects with available data. Resistanceassociated variant R155K remained detectable in 5/8 (63%) subjects through Post-Treatment
Week 24, and in 1/5 (20%) subjects through Post-Treatment Week 48. Resistance-associated
D168 substitutions remained detectable in 6/22 (27%) subjects through Post-Treatment Week 24,
and were no longer detectable through Post-Treatment Week 48.
Among HCV genotype 1b infected subjects who experienced virologic failure with a regimen
including ombitasvir and paritaprevir, a treatment-emergent NS5A Y93H substitution persisted
through at least Post-Treatment Week 48 in 2/2 subjects, and a NS3 D168V treatment-emergent
substitution persisted through Post-Treatment Week 24 in 2/4 subjects, but was no longer
detectable through Post-Treatment Week 48 (0/4 subjects).
The lack of detection of virus containing a resistance-associated substitution does not indicate
that the resistant virus is no longer present at clinically significant levels. The long-term clinical
impact of the emergence or persistence of virus containing VIEKIRA XR-resistance-associated
substitutions is unknown.
Effect of Baseline HCV Polymorphisms on Treatment Response
A pooled analysis of subjects in the Phase 3 clinical trials of dasabuvir, ombitasvir, and
paritaprevir with or without ribavirin was conducted to explore the association between baseline
HCV NS5B, NS5A, or NS3 resistance-associated polymorphisms and treatment outcome.
Baseline samples from HCV genotype 1a infected subjects who experienced virologic failure
(n=47), as well as samples from a subset of demographically matched subjects who achieved
SVR (n=94), were analyzed to compare the frequencies of resistance-associated polymorphisms
in these two populations. The NS3 Q80K polymorphism was detected in approximately 38% of
subjects in this analysis and was enriched approximately 2-fold in virologic failure subjects
compared to SVR-achieving subjects. Ombitasvir resistance-associated polymorphisms in NS5A
(pooling data from all resistance-associated amino acid positions) were detected in
approximately 22% of subjects in this analysis and similarly were enriched approximately 2-fold
in virologic failure subjects. Dasabuvir resistance-associated polymorphisms in NS5B were
detected in approximately 5% of subjects in this analysis and were not enriched in virologic
failure subjects.
In contrast to the Phase 3 subset analysis, no association of NS3 or NS5A polymorphisms and
treatment outcome was seen in an analysis of noncirrhotic HCV genotype 1a-infected subjects
(n=174 for NS3 and n=183 for NS5A) who received dasabuvir, ombitasvir, and paritaprevir with
or without ribavirin (for 12 or 24 weeks) in a Phase 2b trial.
Baseline HCV polymorphisms are not expected to have a substantial impact on the likelihood of
achieving SVR when VIEKIRA XR is used as recommended for HCV genotype 1a and 1b
infected patients, based on the low virologic failure rates observed in clinical trials.
Cross-resistance
Cross-resistance is expected among NS5A inhibitors, NS3/4A protease inhibitors, and nonnucleoside NS5B-palm inhibitors by class. Dasabuvir retained full activity against HCV
replicons containing a single NS5B L159F, S282T, or V321A substitution, which are associated
with resistance or prior exposure to nucleot(s)ide analogue NS5B polymerase inhibitors. In
clinical trials of the components of VIEKIRA XR, no subjects who experienced virologic failure
had treatment-emergent substitutions potentially associated with resistance to nucleot(s)ide
analogue NS5B polymerase inhibitors.
The impact of prior dasabuvir, ombitasvir, or paritaprevir treatment experience on the efficacy of
other NS5B inhibitors, NS5A inhibitors, or NS3/4A protease inhibitors has not been studied.
Similarly, the efficacy of VIEKIRA XR has not been studied in subjects who have failed prior
treatment with another NS5B inhibitor, NS5A inhibitor, or NS3/4A protease inhibitor.
13 NONCLINICAL TOXICOLOGY
13.1 Carcinogenesis, Mutagenesis, Impairment of Fertility
Carcinogenesis and Mutagenesis
Dasabuvir
Dasabuvir was not carcinogenic in a 6-month transgenic mouse study up to the highest dose
tested (2000 mg per kg per day). Similarly, dasabuvir was not carcinogenic in a 2-year rat
study up to the highest dose tested (800 mg per kg per day), resulting in dasabuvir exposures
approximately 19-fold higher than those in humans at 500 mg.
Dasabuvir was not genotoxic in a battery of in vitro or in vivo assays, including bacterial
mutagenicity, chromosome aberration using human peripheral blood lymphocytes and in vivo
rat micronucleus assays.
Ombitasvir
Ombitasvir was not carcinogenic in a 6-month transgenic mouse study up to the highest dose
tested (150 mg per kg per day). Similarly, ombitasvir was not carcinogenic in a 2-year rat
study up to the highest dose tested (30 mg per kg per day), resulting in ombitasvir exposures
approximately 16-fold higher than those in humans at 25 mg.
Ombitasvir and its major inactive human metabolites (M29, M36) were not genotoxic in a
battery of in vitro or in vivo assays, including bacterial mutagenicity, chromosome aberration
using human peripheral blood lymphocytes and in vivo mouse micronucleus assays.
Paritaprevir, ritonavir
Paritaprevir, ritonavir was not carcinogenic in a 6-month transgenic mouse study up to the
highest dose tested (300/30 mg per kg per day). Similarly, paritaprevir, ritonavir was not
carcinogenic in a 2-year rat study up to the highest dose tested (300/30 mg per kg per day),
resulting in paritaprevir exposures approximately 9-fold higher than those in humans at 150
mg.
Paritaprevir was positive in an in vitro chromosome aberration test using human
lymphocytes. Paritaprevir was negative in a bacterial mutation assay, and in two in vivo
genetic toxicology assays (rat bone marrow micronucleus and rat liver Comet tests).
If VIEKIRA XR is administered with ribavirin, refer to the prescribing information for ribavirin
for information on carcinogenesis, and mutagenesis.
Impairment of Fertility
Dasabuvir
Dasabuvir had no effects on embryo-fetal viability or on fertility when evaluated in rats up to
the highest dose of 800 mg per kg per day. Dasabuvir exposures at this dose were
approximately 16-fold the exposure in humans at the recommended clinical dose.
Ombitasvir
Ombitasvir had no effects on embryo-fetal viability or on fertility when evaluated in mice up
to the highest dose of 200 mg per kg per day. Ombitasvir exposures at this dose were
approximately 25-fold the exposure in humans at the recommended clinical dose.
Paritaprevir, ritonavir
Paritaprevir, ritonavir had no effects on embryo-fetal viability or on fertility when evaluated
in rats up to the highest dose of 300/30 mg per kg per day. Paritaprevir exposures at this dose
were approximately 2- to 5-fold the exposure in humans at the recommended clinical dose.
If VIEKIRA XR is administered with ribavirin, refer to the prescribing information for ribavirin
for information on Impairment of Fertility.
14 CLINICAL STUDIES
14.1 Description of Clinical Trials
Table 10 presents the clinical trial design including different treatment arms that were conducted
with the components of VIEKIRA XR with or without ribavirin in subjects with chronic hepatitis
C (HCV) genotype 1 (GT1) infection. For detailed description of trial design and recommended
regimen and duration [see Dosage and Administration (2) and Clinical Studies (14)].
Table 10. Clinical Trials Conducted with the Components of VIEKIRA XR With or
Without Ribavirin (RBV) in Subjects with Chronic HCV GT1 Infection
Trial
Population
Study Arms and Duration
(Number of Subjects Treated)
SAPPHIRE-I
GT1 (a and b)
• Components of VIEKIRA XR + RBV for 12 weeks
(double-blind)
TNa without cirrhosis
(473)
• Placebo for 12 weeks (158)
SAPPHIRE-II
(double-blind)
GT1 (a and b)
• Components of VIEKIRA XR + RBV for 12 weeks
TEb without cirrhosis
(297)
• Placebo for 12 weeks (97)
PEARL-II
(open-label)
GT1b
TE without cirrhosis
PEARL-III
(double-blind)
GT1b
• Components of VIEKIRA XR + RBV for 12 weeks
TN without cirrhosis
(210)
• Components of VIEKIRA XR for 12 weeks (209)
PEARL-IV
(double-blind)
GT1a
• Components of VIEKIRA XR + RBV for 12 weeks
TN without cirrhosis
(100)
• Components of VIEKIRA XR for 12 weeks (205)
TURQUOISE-II
(open-label)
GT1 (a and b)
TN & TE with
• Components of VIEKIRA XR + RBV for 12 weeks
(88)
• Components of VIEKIRA XR for 12 weeks (91)
• Components of VIEKIRA XR + RBV for 12 weeks
(208)
compensated
cirrhosis
TURQUOISE-III
(open-label)
GT1b
TN & TE with
compensated
cirrhosis
• Components of VIEKIRA XR + RBV for 24 weeks
(172)
• Components of VIEKIRA XR for 12 weeks (60)
a. TN, treatment-naïve was defined as not having received any prior therapy for HCV infection.
b. TE, treatment-experienced subjects were defined as having failed to respond to prior
treatment with pegIFN/RBV.
The components of VIEKIRA XR with RBV were also evaluated in the following two studies:
• HCV GT1-infected liver transplant recipients (CORAL-I) [see Clinical Studies (14.5)].
• Subjects with HCV GT1 co-infected with HIV-1 (TURQUOISE-I) [see Clinical Studies
(14.6)].
In all clinical trials, the ombitasvir, paritaprevir, ritonavir dose was 25/150/100 mg once daily
and the dasabuvir dose was 250 mg twice daily and doses were not adjusted. For subjects who
received RBV, the RBV dose was 1000 mg per day for subjects weighing less than 75 kg or
1200 mg per day for subjects weighing greater than or equal to 75 kg. RBV dose adjustments
were performed according to the RBV labeling.
In all clinical trials, sustained virologic response was defined as HCV RNA below the lower
limit of quantification (<LLOQ) 12 weeks after the end of treatment (SVR12). Plasma HCV
RNA levels were measured using the COBAS TaqMan HCV test (version 2.0), for use with the
High Pure System, which has an LLOQ of 25 IU per mL. Outcomes for subjects not achieving
an SVR12 were recorded as on-treatment virologic failure (VF), post-treatment virologic relapse
through post-treatment Week 12 or failure due to other non-virologic reasons (e.g., premature
discontinuation, adverse event, lost to follow-up, consent withdrawn).
14.2 Clinical Trial Results in Adults with Chronic HCV Genotype 1a and 1b Infection
without Cirrhosis
Subjects with Chronic HCV GT1a Infection without Cirrhosis
Subjects with HCV GT1a infection without cirrhosis treated with the components of VIEKIRA
XR with RBV for 12 weeks in SAPPHIRE-I and -II and in PEARL-IV [see Clinical Studies
(14.1)] had a median age of 53 years (range: 18 to 70); 63% of the subjects were male; 90% were
White; 7% were Black/African American; 8% were Hispanic or Latino; 19% had a body mass
index of at least 30 kg per m2; 55% of patients were enrolled in US sites; 72% had IL28B
(rs12979860) non-CC genotype; 85% had baseline HCV RNA levels of at least 800,000 IU per
mL.
Table 11 presents treatment outcomes for HCV GT1a treatment-naïve and treatment-experienced
subjects treated with the components of VIEKIRA XR with RBV for 12 weeks in SAPPHIRE-I,
PEARL-IV and SAPPHIRE-II.
Treatment-naïve, HCV GT1a-infected subjects without cirrhosis treated with the components of
VIEKIRA XR with RBV for 12 weeks in PEARL-IV had a significantly higher SVR12 rate than
subjects treated with the components of VIEKIRA XR without RBV (97% and 90%
respectively; difference +7% with 95% confidence interval, +1% to +12%). The components of
VIEKIRA XR without RBV were not studied in treatment-experienced subjects with GT1a
infection.
In SAPPHIRE-I and SAPPHIRE-II, no placebo subject achieved a HCV RNA <25 IU/mL during
treatment.
Table 11. SVR12 for HCV Genotype 1a-Infected Subjects without Cirrhosis Who Were
Treatment-Naïve or Previously Treated with PegIFN/RBV
Components of
VIEKIRA XR + RBV
for 12 Weeks
% (n/N)
GT1a treatment-naïve
96% (308/322)
SAPPHIRE-I SVR12
Outcome for subjects without SVR12
On-treatment VF
<1% (1/322)
Relapse
2% (6/314)
Other
2% (7/322)
97% (97/100)
PEARL-IV SVR12
Outcome for subjects without SVR12
On-treatment VF
1% (1/100)
Relapse
1% (1/98)
Other
1% (1/100)
GT1a treatment-experienced
96% (166/173)
SAPPHIRE-II SVR12
Outcome for subjects without SVR12
On-treatment VF
0% (0/173)
Relapse
3% (5/172)
Other
1% (2/173)
SVR12 by Prior pegIFN Experience
Null Responder
95% (83/87)
Partial Responder
100% (36/36)
Relapser
94% (47/50)
Subjects with Chronic HCV GT1b Infection without Cirrhosis
Subjects with HCV GT1b infection without cirrhosis were treated with the components of
VIEKIRA XR with or without RBV for 12 weeks in PEARL-II and -III [see Clinical Studies
(14.1)]. Subjects had a median age of 52 years (range: 22 to 70); 47% of the subjects were male;
93% were White; 5% were Black/African American; 2% were Hispanic or Latino; 21% had a
body mass index of at least 30 kg per m2; 21% of patients were enrolled in US sites; 83% had
IL28B (rs12979860) non-CC genotype; 77% had baseline HCV RNA levels of at least 800,000
IU per mL.
The SVR rate for HCV GT1b-infected subjects without cirrhosis treated with the components of
VIEKIRA XR without RBV for 12 weeks in PEARL-II (treatment-experienced: null responder,
n=32; partial responder, n=26; relapser, n=33) and PEARL-III (treatment-naïve, n=209) was
100%.
14.3 Clinical Trial Results in Adults with Chronic HCV Genotype 1a and 1b Infection and
Compensated Cirrhosis
The components of VIEKIRA XR with and without ribavirin were evaluated in two clinical trials
in patients with compensated cirrhosis.
TURQUOISE-II was an open-label trial that enrolled 380 HCV GT1 subjects with cirrhosis and
mild hepatic impairment (Child-Pugh A) who were either treatment-naïve or did not achieve
SVR with prior treatment with pegIFN/RBV. Subjects were randomized to receive the
components of VIEKIRA XR with RBV for either 12 or 24 weeks of treatment.
Treated subjects had a median age of 58 years (range: 21 to 71); 70% of the subjects were male;
95% were White; 3% were Black/African American; 12% were Hispanic or Latino; 28% had a
body mass index of at least 30 kg per m2; 43% of patients were enrolled in US sites; 82% had
IL28B (rs12979860) non-CC genotype; 86% had baseline HCV RNA levels of at least 800,000
IU per mL; 69% had HCV GT1a infection, 31% had HCV GT1b infection; 42% were treatmentnaïve, 36% were prior pegIFN/RBV null responders; 8% were prior pegIFN/RBV partial
responders, 14% were prior pegIFN/RBV relapsers; 15% had platelet counts of less than 90 x 109
per L; 50% had albumin less than 4.0 mg per dL.
TURQUOISE-III was an open-label trial that enrolled 60 HCV GT1b-infected subjects with
cirrhosis and mild hepatic impairment (Child-Pugh A) who were either treatment-naïve or did
not achieve SVR with prior treatment with pegIFN/RBV. Subjects received the components of
VIEKIRA XR without RBV for 12 weeks. Treated subjects had a median age of 61 years (range:
26 to 78); including 45% treatment-naïve and 55% pegIFN/RBV treatment-experienced; 25%
were ≥65 years; 62% were male; 12% were Black; 5% were Hispanic or Latino; 28% had a body
mass index of at least 30 kg per m2; 40% of patients were enrolled in US sites; 22% had platelet
counts of less than 90 x 109 per L; 17% had albumin less than 35 g/L; 92% had baseline HCV
RNA levels of at least 800,000 IU per mL; 83% had IL28B (rs12979860) non-CC genotype.
Table 12 presents treatment outcomes for GT1a- and GT1b-infected treatment-naïve and
treatment-experienced subjects.
In GT1a infected subjects, the overall SVR12 rate difference between 24 and 12 weeks of
treatment with the components of VIEKIRA XR with RBV was +6% with 95% confidence
interval (-0.1% to +13% with differences varying by pretreatment history).
Table 12. TURQUOISE-II: SVR12 for Chronic HCV Genotype 1-Infected Subjects with
Cirrhosis Who Were Treatment-Naïve or Previously Treated with pegIFN/RBV
GT1a
GT1b
(TURQUOISE-II)
(TURQUOISE-III)
SVR12
Outcome for subjects
without SVR12
On-treatment VF
Relapse
Other
SVR12 for Naïve
SVR12 by Prior pegIFN
Experience
Null Responder
Partial Responder
Relapser
Components of
VIEKIRA XR
+ RBV for
24 Weeks
% (n/N)
95% (115/121)
Components of
VIEKIRA XR
+ RBV for
12 Weeks
% (n/N)
89% (124/140)
Components of
VIEKIRA XR
without RBV for
12 Weeks
% (n/N)
100% (60/60)
2% (3/121)
1% (1/116)
2% (2/121)
95% (53/56)
<1% (1/140)
8% (11/135)
3% (4/140)
92% (59/64)
0
0
0
100% (27/27)
100% (33/33)
93% (39/42)
100% (10/10)
100% (13/13)
80% (40/50)
100% (11/11)
93% (14/15)
100% (7/7)
100% (5/5)
100% (3/3)
14.4 Effect of Ribavirin Dose Reductions on SVR12
Seven percent of subjects (101/1551) treated with the components of VIEKIRA XR with RBV
had a RBV dose adjustment due to a decrease in hemoglobin level; of these, 98% (98/100)
achieved an SVR12.
14.5 Clinical Trial of Selected Liver Transplant Recipients (CORAL-I)
The components of VIEKIRA XR with RBV were administered for 24 weeks to 34 HCV GT1infected liver transplant recipients who were at least 12 months post transplantation at enrollment
with normal hepatic function and mild fibrosis (Metavir fibrosis score F2 or lower). The initial
dose of RBV was left to the discretion of the investigator with 600 to 800 mg per day being the
most frequently selected dose range at initiation of the components of VIEKIRA XR and at the
end of treatment.
Of the 34 subjects (29 with HCV GT1a infection and 5 with HCV GT1b infection) enrolled,
(97%) achieved SVR12 (97% in subjects with GT1a infection and 100% of subjects with GT1b
infection). One subject with HCV GT1a infection relapsed post-treatment.
14.6 Clinical Trial in Subjects with HCV/HIV-1 Co-infection (TURQUOISE-I)
In an open-label clinical trial 63 subjects with HCV GT1 infection co-infected with HIV-1 were
treated for 12 or 24 weeks with the components of VIEKIRA XR with RBV. Subjects were on a
stable HIV-1 antiretroviral therapy (ART) regimen that included tenofovir disoproxil fumarate
plus emtricitabine or lamivudine, administered with ritonavir boosted atazanavir or raltegravir.
Subjects on atazanavir stopped the ritonavir component of their HIV-1 ART regimen upon
initiating treatment with the components of VIEKIRA XR with RBV. Atazanavir was taken with
the morning dose. The ritonavir component of the HIV-1 ART regimen was restarted after
completion of treatment.
Treated subjects had a median age of 51 years (range: 31 to 69); 24% of subjects were black;
81% of subjects had IL28B (rs12979860) non-CC genotype; 19% of subjects had compensated
cirrhosis; 67% of subjects were HCV treatment-naïve; 33% of subjects had failed prior treatment
with pegIFN/RBV; 89% of subjects had HCV genotype 1a infection.
The SVR12 rates were 91% (51/56) for subjects with HCV GT1a infection and 100% (7/7) for
those with HCV GT1b infection. Of the 5 subjects who were non-responders, 1 experienced
virologic breakthrough, 1 discontinued treatment, 1 experienced relapse and 2 subjects had
evidence of HCV re-infection post-treatment.
One subject had confirmed HIV-1 RNA >400 copies/mL during the post-treatment period. This
subject had no evidence of resistance to the ART regimen. No subjects switched their ART
regimen due to loss of plasma HIV-1 RNA suppression.
14.7 Durability of Response
In an open-label clinical trial, 92% of subjects (526/571) who received various combinations of
the direct acting antivirals included in VIEKIRA XR with or without RBV achieved SVR12, and
99% of those who achieved SVR12 maintained their response through 48 weeks post-treatment
(SVR48).
16 HOW SUPPLIED/STORAGE AND HANDLING
VIEKIRA XR is dispensed in a monthly carton for a total of 28 days of therapy. Each monthly
carton contains four weekly cartons. Each weekly carton contains seven daily dose packs.
Each child-resistant daily dose pack contains three tablets. The NDC number is 0074-0063-28.
Dasabuvir, ombitasvir, paritaprevir, and ritonavir 200 mg/8.33 mg/50 mg/33.33 mg tablets are
pale yellow-colored, film-coated, oblong shaped, debossed with “3QD” on one side.
Store at or below 30°C (86°F).
17 PATIENT COUNSELING INFORMATION
Advise the patient to read the FDA-approved patient labeling (Medication Guide).
Inform patients to review the Medication Guide for ribavirin [see Warnings and Precautions
(5.3)].
Risk of ALT Elevations or Hepatic Decompensation and Failure
Inform patients to watch for early warning signs of liver inflammation or failure, such as fatigue,
weakness, lack of appetite, nausea and vomiting, as well as later signs such as jaundice, onset of
confusion, abdominal swelling, and discolored feces, and to consult their health care professional
without delay if such symptoms occur [see Warnings and Precautions (5.1 and 5.2) and Adverse
Reactions (6)].
Pregnancy
Advise patients taking VIEKIRA XR with ribavirin to avoid pregnancy during treatment and
within 6 months of stopping ribavirin. Inform patients to notify their health care provider
immediately in the event of a pregnancy [see Use in Specific Populations (8.1)].
Drug Interactions
Inform patients that VIEKIRA XR may interact with some drugs; therefore, patients should be
advised to report to their healthcare provider the use of any prescription, non-prescription
medication or herbal products [see Contraindications (4), Warnings and Precautions (5.4) and
Drug Interactions (7)].
Inform patients that contraceptives containing ethinyl estradiol are contraindicated with
VIEKIRA XR [see Contraindications (4) and Warnings and Precautions (5.2)].
Administration
Advise patients to take VIEKIRA XR every day at the regularly scheduled time and that
VIEKIRA XR must be taken with a meal because taking it under fasting conditions may result in
reduced virologic response and possible development of resistance. Inform patients to swallow
tablets whole and not to consume alcohol within 4 hours of taking VIEKIRA XR [see Dosage
and Administration (2.2)].
Inform patients that it is important not to miss or skip doses and to take VIEKIRA XR for the
duration that is recommended by the healthcare provider.
Manufactured by AbbVie Inc., North Chicago, IL 60064.
VIEKIRA XR and NORVIR are trademarks of AbbVie Inc. All other brands listed are
trademarks of their respective owners and are not trademarks of AbbVie Inc. The makers of
these brands are not affiliated with and do not endorse AbbVie Inc. or its products.
© 2016 AbbVie Inc. All rights reserved.
03-B193
MEDICATION GUIDE
VIEKIRA XR (vee-KEE-rah-XR)
(dasabuvir, ombitasvir, paritaprevir, and ritonavir) extended-release tablets
for oral use
Important: When taking VIEKIRA XR in combination with ribavirin, you should also read the
Medication Guide that comes with ribavirin.
What is the most important information I should know about VIEKIRA XR?
VIEKIRA XR may cause severe liver problems, especially in people with certain types of cirrhosis. These
severe liver problems can lead to the need for a liver transplant, or can lead to death.
VIEKIRA XR can cause increases in your liver function blood test results, especially if you use ethinyl
estradiol-containing medicines (such as some birth control products).
• You must stop using ethinyl estradiol-containing medicines before you start treatment with VIEKIRA
XR. See the section “Who should not take VIEKIRA XR?” for a list of these medicines.
• If you use these medicines as a method of birth control, you must use another method of birth control
during treatment with VIEKIRA XR, and for about 2 weeks after you finish treatment with VIEKIRA
XR. Your healthcare provider will tell you when you may begin taking ethinyl estradiol-containing
medicines.
• Your healthcare provider should do blood tests to check your liver function during the first 4 weeks
and then as needed, during treatment with VIEKIRA XR.
• Your healthcare provider may tell you to stop taking VIEKIRA XR if you develop signs or symptoms of
liver problems.
• Tell your healthcare provider right away if you develop any of the following symptoms, or if they
worsen during treatment with VIEKIRA XR:
◦
◦
◦
◦
tiredness
weakness
loss of appetite
nausea and vomiting
◦
◦
◦
◦
yellowing of your skin or eyes
color changes in your stools
confusion
swelling of the stomach area
What is VIEKIRA XR?
• VIEKIRA XR is a prescription medicine used with or without ribavirin to treat people with genotype 1
chronic (lasting a long time) hepatitis C virus (HCV) infection.
• VIEKIRA XR can be used in people who have compensated cirrhosis.
• VIEKIRA XR is not for people with advanced cirrhosis (decompensated). If you have cirrhosis, talk to
your healthcare provider before taking VIEKIRA XR. VIEKIRA XR is not for people with certain types
of liver problems.
It is not known if VIEKIRA XR is safe and effective in children under 18 years of age.
Who should not take VIEKIRA XR?
Do not take VIEKIRA XR if you:
• have certain liver problems
• take any of the following medicines:
®
◦ alfuzosin hydrochloride (Uroxatral )
®
®
®
®
®
®
◦ carbamazepine (Carbatrol , Epitol , Equetro , Tegretol , TEGRETOL-XR , TERIL )
®
◦ cisapride (Propulsid )
®
◦ colchicine (Colcrys ) in patients who have certain kidney or liver problems
®
◦ dronedarone (Multaq )
®
®
◦ efavirenz (Atripla , Sustiva )
◦ ergot containing medicines including:
®
®
®
®
®
®
■ ergotamine tartrate (Cafergot , Ergomar , Ergostat , Medihaler , Migergot , Wigraine ,
®
Wigrettes )
®
®
■ dihydroergotamine mesylate (D.H.E. 45 , Migranal )
®
®
■ methylergonovine (Ergotrate , Methergine )
◦ ethinyl estradiol-containing medicines:
■ combination birth control pills or patches, such as Lo Loestrin FE, Norinyl , Ortho Tri-Cyclen
®
®
Lo , Ortho Evra
®
■ hormonal vaginal rings such as NuvaRing
®
■ the hormone replacement therapy medicine, Fem HRT
®
◦ gemfibrozil (Lopid )
®
®
®
◦ lovastatin (Advicor , Altoprev , Mevacor )
®
◦ lurasidone (Latuda )
◦ midazolam, when taken by mouth
®
®
◦ phenytoin (Dilantin , Phenytek )
®
◦ phenobarbital (Luminal )
®
◦ pimozide (Orap )
®
◦ ranolazine (Ranexa )
®
®
®
◦ rifampin (Rifadin , Rifamate , Rifater , Rimactane)
®
◦ sildenafil citrate (Revatio ), when taking for pulmonary artery hypertension (PAH)
®
®
®
◦ simvastatin (Simcor , Vytorin , Zocor )
◦ St. John’s wort (Hypericum perforatum) or a product that contains St. John’s wort
®
◦ Triazolam (Halcion )
®
• have had a severe skin rash after taking ritonavir (Norvir )
®
®
What should I tell my healthcare provider before taking VIEKIRA XR?
Before taking VIEKIRA XR tell your healthcare provider about all your medical conditions,
including if you:
• have liver problems other than hepatitis C infection. See “Who should not take VIEKIRA XR?”
• have HIV infection
®
®
• have had a liver transplant. If you take the medicines tacrolimus (Prograf ) or cyclosporine (Gengraf ,
®
®
Neoral , Sandimmune ) to help prevent rejection of your transplanted liver, the amount of these
medicines in your blood may increase during treatment with VIEKIRA XR.
◦ Your healthcare provider should check the level of tacrolimus or cyclosporine in your blood, and if
needed may change your dose of these medicines or how often you take them.
◦ When you finish taking VIEKIRA XR or if you have to stop VIEKIRA XR for any reason, your
healthcare provider should tell you what dose of tacrolimus or cyclosporine to take and how often
you should take it.
• are pregnant or plan to become pregnant. It is not known if VIEKIRA XR will harm your unborn baby.
When taking VIEKIRA XR in combination with ribavirin you should also read the ribavirin
Medication Guide for important pregnancy information.
• are breastfeeding or plan to breastfeed. It is not known if VIEKIRA XR passes into your breast milk.
Talk to your healthcare provider about the best way to feed your baby if you take VIEKIRA XR.
Tell your healthcare provider about all the medicines you take, including prescription and over-thecounter medicines, vitamins, and herbal supplements. Some medicines interact with VIEKIRA XR. Keep
a list of your medicines to show your healthcare provider and pharmacist.
• You can ask your healthcare provider or pharmacist for a list of medicines that interact with VIEKIRA
XR.
• Do not start taking a new medicine without telling your healthcare provider. Your healthcare
provider can tell you if it is safe to take VIEKIRA XR with other medicines.
• When you finish treatment with VIEKIRA XR:
◦ If your healthcare provider changed the dose of one of your usual medicines during treatment
with VIEKIRA XR: Ask your healthcare provider about when you should change back to your
original dose after you finish treatment with VIEKIRA XR.
◦ If your healthcare provider told you to stop taking one of your usual medicines during treatment
with VIEKIRA XR: Ask your healthcare provider if you should start taking these medicines again
after you finished treatment with VIEKIRA XR.
How should I take VIEKIRA XR?
• Take VIEKIRA XR exactly as your healthcare provider tells you to take it. Do not change your dose.
• Do not stop taking VIEKIRA XR without first talking with your healthcare provider.
Take VIEKIRA XR tablets one time each day.
VIEKIRA XR tablets must be taken with a meal.
Swallow VIEKIRA XR tablets whole. Do not split, crush, or chew the tablets.
Do not drink alcohol within 4 hours of taking VIEKIRA XR.
VIEKIRA XR comes in monthly cartons that contain enough medicine for 28 days.
◦ Each monthly carton of VIEKIRA XR contains 4 smaller cartons.
◦ Each of the 4 smaller cartons contains enough child resistant daily dose packs of medicine to
last for 7 days (1 week).
◦ Each daily dose pack contains all of your VIEKIRA XR medicine for 1 day (3 tablets). Follow the
instructions on each daily dose pack about how to remove the tablets.
• It is important that you do not miss or skip doses of VIEKIRA XR during treatment.
• If you take too much VIEKIRA XR, call your healthcare provider or go to the nearest hospital
emergency room right away.
•
•
•
•
•
What are the possible side effects of VIEKIRA XR?
VIEKIRA XR can cause serious side effects. See “What is the most important information I should
know about VIEKIRA XR?”
Common side effects of VIEKIRA XR when used with ribavirin include:
• tiredness
• nausea
• itching
• skin reactions such as redness or rash
• sleep problems
• feeling weak
Common side effects of VIEKIRA XR when used without ribavirin include:
• nausea
• itching
• sleep problems
These are not all the possible side effects of VIEKIRA XR. Call your doctor for medical advice about side
effects. You may report side effects to FDA at 1-800-FDA-1088.
How should I store VIEKIRA XR?
• Store VIEKIRA XR at or below 86°F (30°C).
Keep VIEKIRA XR and all medicines out of the reach of children.
General information about the safe and effective use of VIEKIRA XR
Medicines are sometimes prescribed for purposes other than those listed in a Medication Guide. Do not
use VIEKIRA XR for a condition for which it was not prescribed. Do not give VIEKIRA XR to other people,
even if they have the same symptoms that you have. It may harm them. You can ask your pharmacist or
healthcare provider for information about VIEKIRA XR that is written for health professionals.
What are the ingredients in VIEKIRA XR?
Active ingredients: dasabuvir, ombitasvir, paritaprevir, and ritonavir
Inactive ingredients:
• The extended release layer contains: copovidone, K value 28, hypromellose 2208, 17,700 (mPa*s),
colloidal silicon dioxide/colloidal anhydrous silica, and magnesium stearate.
• The immediate release layer contains: copovidone, K value 28, vitamin E polyethylene glycol
succinate, propylene glycol monolaurate, sorbitan monolaurate, colloidal silicon dioxide/colloidal
anhydrous silica.
• The tablet coating contains: hypromellose (6 mPa*s), hypromellose (15 mPa*s), polyethylene glycol
400, hydroxypropyl cellulose, polysorbate 80, polyethylene glycol 3350/macrogol 4000, talc, titanium
dioxide, colloidal silicon dioxide/colloidal anhydrous silica and iron oxide yellow.
Manufactured by AbbVie Inc., North Chicago, IL 60064.
VIEKIRA XR and NORVIR are trademarks of AbbVie Inc. All other brands listed are trademarks of their respective owners and are not trademarks of
AbbVie Inc. The makers of these brands are not affiliated with and do not endorse AbbVie Inc. or its products.
For more information go to www.viekira.com or call 1-844-843-5472.
This Medication Guide has been approved by the U.S. Food and Drug Administration.
Issued: July 2016
03-B193