LAB #19
Biology 241 – Lab
LAB #19
( 19 th /21 Lab Sessions for Fall Quarter, 2008)
TOPICS TO BE COVERED:
»Discussion of the Anatomy of the Eye (Oculus)
»Demonstration/Dissection of a Cow’s Oculus
»Physiology of the Eye: Visual Tests
DESIRED OUTCOMES:
After completing the activities described for this lab session, students should:
»Be able to identify and describe the accessory structures of the eye
»Be able to identify, explain the actions of, and cite the innervation of each of the six
extrinsic ocular muscles
»Be able to describe and identify the external and internal components of the eye.
»Be able to describe the three tunics of the oculus and their individual subcomponents
»Be able to identify the structures of a dissected cow eye
»Be able to demonstrate the use of a Snellen eye chart, blind spot mapping technique and
accommodation determination.
MATERIALS NEEDED:
» Oversize models of Eye
» Preserved cow eyes
» Gloves
» Safety glasses (or your own glasses)
» Snellen Eye Chart
» Blind Spot Testing Cards
»
Pencils
» Masking Tape
»
»
Wall Posters of The Eye
Rulers
» Small dissection pans (with sides, and black resin bottom)
»
Dissection tools (large forceps, sharp scissors, blunt probes, dissection needles, scalpels)
»Photographic Atlas, Ch. 11
Introduction:
Sensation is broadly defined as awareness of changes in the internal and external environments.
Sensation may be conscious or subconscious, depending on the destination of the sensory information. If the sensory information is ultimately relayed to the cerebral cortex for conscious recognition/interpretation, then it is called perception .
For example: Located in certain blood vessels are special receptors ( called baroreceptors
) whose “job” it is to detect changes in blood pressure. Any change in blood pressure is relayed as important information to the brainstem, which then, initiates changes as necessary to ensure that blood pressure remains relatively constant.
This blood pressure homeostatic information exchange never involves the cerebral cortex, thus you are not consciously aware of it. The sensation has still taken place; but no perception of it has arisen.
However, information that is eventually taken to the cerebral cortex (e.g., the smell of coffee brewing or bacon sizzling, or the taste of either of these) is something of which you become consciously aware. This type of sensation is called perception . It is perception that is the focus of today’s lab activities. You will be examining the anatomy and physiology of the organs of perception, commonly called the Special Senses (“special” because they are all mediated by Cranial Nerves ONLY). The Special Senses include: Vision, Taste, Smell,
Hearing, and Equilibrium. (Remember: Touch is NOT a special sense ….because it is mediated by Cranial and
Spinal Nerves.)
Biology 241 – LAB #18 – continued Page Two
Activity #1: Examination of Oculus Anatomy on Oversize Anatomical Models
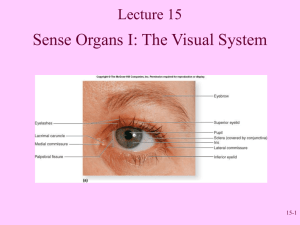
The eye is a complex organ that consists of external structures such as the eyelids and eyelashes , accessory structures such as the lacrimal apparatus , and the oculus itself. Many of the external and accessory structures of the eye serve to protect the delicate oculus.
Anteriorly, the eye is covered by the eyelids, or palpebrae . The eyelids meet medially and laterally at the medial and lateral canthus , respectively. ( A small, red, fleshy structure in the medial canthus of the eye, the lacrimal caruncle , contains modified sebaceous and sweat glands; the secretions from these glands may accumulate in the medial canthus during long periods of sleep and are called “sleepers”.) The interior of the eyelids, as well as most of the anterior oculus, is covered with a thin mucous membrane called the conjunctiva . ( That palpebral conjunctiva lines the underside of the eyelids; while the bulbar conjunctiva covers the cornea.
) Within the eyelids are the
Meibomian glands , whose oily secretions help to keep the eye lubricated.
The eyelashes are short hairs that project from the border of each eyelid. Eyelashes and eyebrows protect the eyeball from foreign objects such as perspiration and dust and also partially shade the eyeball from the sun. Sebaceous ciliary glands , located at the base of the hair follicles, help lubricate the eyeball. An infection of these glands is called a sty .
The two most prominent accessory structures of the eye are the (1) lacrimal apparatus , which produces and drains tears, and (2) the extraocular muscles (also called extrinsic ocular muscles) because they do not originate within the eye, but rather on the boney, skeletal components of the orbit and insert into the outer surface of the sclera of each oculus.)
The lacrimal apparatus consists of six structures: the lacrimal glands are located at the superolateral corner of each oculus. Each contains 6 – 12 excretory lacrimal ducts which deliver a slightly alkaline solution, called lacrimal fluid or tears, onto the anterior surface of the eye. ( This fluid contains an antibacterial enzyme called lysozyme which attacks any bacteri that may be on the surface of the eye.) The tears move medially across the surface of the eye and enter two small openings of the medial canthus called the lacrimal puncta and pass into two ducts, the lacrimal canals , which lead to an expanded portion of the nasolacrimal duct called the lacrimal sac . The nasolacrimal duct drains the tears into the nasal cavity ( with openings inferior to the inferior nasal concha) . Tears clean, moisten, and lubricate the surface of the oculus.
The six extrinsic (external) eye muscles control the movements of the oculus. The superior rectus , inferior rectus , medial rectus , and lateral rectus are straight, strap-like muscles that move the eyeball up and down and side to side. The superior and inferior oblique muscles attache diagonally on the oculus. The superior oblique has a tendon passing through a trochlea (“pulley”) located on the superomedial aspect of the orbit.
The superior oblique muscle “rolls the eye down and out” (remember: DARM ( d epression, a bduction, r otation m edially
) and the inferior oblique “rolls it up and out” (remember:
EARL ( e levation, a bduction, r otation l aterally )
(See Handout on Actions of the Six Ocular Muscles )
The oculus itself is a hollow organ with three distinct layers, referred to as tunics:
1.
The outer, fibrous tunic : This outermost layer of the oculus consists mostly of dense regular connective
tissue that has special properties. It is avascular, and consists of two parts:
a. Cornea : Making up the anterior 1/6 of the fibrous tunic, the cornea is crystal-clear and forms a window
that lets light enter the oculus.( The cornea is clear because the collagen of its connective tissue matrix is arranged
in lamellae with the bundles in alternate layers oriented at right angles to those in the intervening layers.
) The cor-
nea functions as one of the refractory media for vision (that is, it bends light coming into the eye.) The
border between the cornea and the sclera is called the limbus ; the scleral venous sinus ( Canal of Schlemm ),
a small passageway that communicates with veins of the eye, is located in this border.
b. Sclera : Making up the posterior 5/6 of the fibrous tunic, the sclera is the white part of the oculus. It is
white because the numerous collagen bundles in its connective tissue matrix are all arranged parallel to
one another forming an opaque and glistening white, tendon-like structure. This structural arrangement
contributes to its thickness and toughness so that it is able to function in shaping and protecting the oculus
Biology 241 – LAB #18 – continued Page Three
and in providing a sturdy anchoring site for the extrinsic eye muscles. It is also continuous posteriorly
with the dura mater that covers the optic nerve.
2. The middle, vascular tunic : Also called the uvea , this tunic carries most of the blood supply to the tissues
of the oculus. It is composed of three main parts:
a. Choroid : The posterior part of the vascular tunic is made of the gighly vascular choroid. The choroid is a very dark-brown pigmented structure whose function is to prevent light scattering within the oculus.
b. Ciliary body : This structure, at the anterior aspect of the oculus, is made chiefly of interlacing smooth
muscle bundles which collectively are called the ciliary muscle . These smooth muscle bundles are impor-
tant in controlling the shape of the lens. Near the lens, the posterior surface of the choroid is thrown into
radiating folds called ciliary processes , which contain the capillaries that secrete aqueous humor ( the fluid
that fills the cavity of the anterior cavity of the oculus ). The suspensory ligament, aka zonular fibers , extends
from the ciliary processes to the lens; this halo of fine fibers encircles and helps hold the lens in its upright
position in the oculus.
c. Iris : The most anterior portion of the uvea , the iris , is the brightly pigmented, most visible part of the eye.
Shaped like a flattened doughnut, the iris lies between the cornea and the lens and is continuous with the ciliary body of the choroid posteriorly. It consists of two smooth muscle layers with bunches of sticky
elastic fibers that congeal into a random pattern before birth. The bundles of each muscle layer are arrang-
ed around an opening called the pupil, either radially or circularly. As the smooth muscle bundles contract
the pupil changes size: either dilating ( when the radially-arranged muscle bundles contract ) or constricting
( when the circularly-arranged muscle bundles contract). The radially-arranged muscles are innervated by sym-
pathetic fibers, while the radially-arranged muscles are innervated parasympathetic fibers.
3. The inner, nervous tunic : This layer consists of the retina and the optic nerve.
a. The retina is a thin, delicate structure that contains photoreceptors called rods and cones. Rods are scat-
tered throughout the retina and are responsible for vision in dim light and for peripheral vision. Cones are
concentrated at the posterior portion of the retina and are found in highest numbers in an area called the macula lutea *. Cones are responsible for color and high-acuity vision. Specific anatomical landmarks of
the retina are:
1. Ora serrata : This is the anterior-most margin of the retina. It is the structure created by the junction
of the anterior-most margin of the retina and the posterior-most margin of the ciliary body.
2. Macula lutea : Located precisely at the posterior/central pole of the oculus is an oval region called the macula lutea with a minute pit in its center called the fovea centralis . The fovea contains only cones;
the macula contains mostly cones, and from the edge of the macula toward the retina periphery, cone
density declines gradually. The retina’s periphery contains only rods, which continuously decrease in
density from there toward the macula. Only the foveae have a sufficient cone density to provide de-
tailed color vision, so anything we which to view critically is focused on the foveae.
3.
Optic disc : Medial to the macula lutea of each oculus, lies the optic disc where the optic nerve origin-
ates and exits the oculus. Because this structure consists only of axons of all the photoreceptors (and
no rods or cones themselves), this structure is also referred to as “the blind spot” because it lacks
photoreceptors and light focused on it cannot be processed.
b. The Optic Nerve : exits the oculus medially, and passes through the optic foramen of the orbit. At the X-
shaped optic chiasma , fibers from the medial aspect of each eye cross over to the opposite side and then
continue on via the optic tracts, where they enter the thalamus and synapse there. Thalamic fibers project
to the occipital (visual) cortex of the brain where visual interpretation occurs.
A structure that is not considered to be part of any of the three tunics is the lens.
The lens divides the oculus into anterior and posterior cavities . The anterior cavity is further subdivided into an anterior chamber
( between the iris and the cornea ) and a posterior chamber ( between the iris and the lens ). Capillaries of the ciliary processes form a watery fluid called aqueous humor , which is secreted into the posterior chamber . This fluid circulates through the pupil and into the anterior chamber where it is reabsorbed back into the blood via the
Biology 241 – LAB #18 – continued Page Four
Canal of Schlemm ( aka scleral venous sinus ). The aqueous humor helps to maintain the intraocular pressure of the eyeball and supply nutrients to the avascular lens and cornea . The second larger cavity of the oculus is the posterior cavity ( aka vitreous cavity ). This cavity contains the vitreous body, a clear jellylike substance that holds the retina against the choroid layer and prevents the oculus from collapsing.
Using the following Guide , check off each of the structures listed as you identify them while examining the anatomical models in lab. Be sure that you can do so on any diagram of an oculus, as well.
GUIDE for STRUCTURES of the OCULUS:
1. Outer Fibrous Tunic
a. Cornea
b. Sclera
2. Middle Vascular Tunic (Uvea)
a. Choroid
b. Ciliary Body
3. Inner Nervous Tunic
a. Retina
b. Ora Serrata
c. Optic Disc
d. Macula lutea
1. Fovea Centralis
c. Limbus
( Canal of Schlemm) 2. Ciliary Muscle
4. Lens
a. Zonular fibers ( aka
Suspensory Ligaments
of the Lens)
1. Ciliary Processes
c. Iris
1. Pupil
5. Optic Nerve
2. Circular Muscles
3. Radial Muscles
6. Optic Chiasm
7. Anterior cavity a. Anterior chamber
b. Posterior chamber
c. Aqueous humor
d. Scleral Venous Sinus
8. Posterior Cavity
a. Vitreous humor ( aka Vitreous Body )
9. Extraocular muscles (aka Extrinsic muscles of the oculus)
a. Superior Rectus b. Inferior Rectus
(aka: Canal of Schlemm) c. Medial Rectus d. Lateral Rectus
e. Superior Oblique f. Inferior Oblique
(Give the Cranial Nerve innervations of each of these!)
Activity #2: Demonstration/Dissection of a Cow’s Oculus
The anatomy of the cow eye is similar to the human eye. Of particular note is that the fibrous tunic, the cornea and the sclera , is difficult to cut and care must be used while dissecting.
1.
First, examine the external features of the eyeball. Note the amount of adipose tissue that serves to cushion the oculus in the boney orbit. Identify the(a) Optic Nerve (II) as it leaves the eyeball; (b) remnants of the extrinsic muscles of the eye; (c) any conjunctiva that may be attached; (d) the sclera; and (e) the cornea. (Note: the cornea, which is normally completely transparent, will be opaque due to absorption of the preservative solution.
)
2.
Securely holding the oculus at its anterior and posterior poles, make an incision in the frontal plane about
¼ inch posterior from the cornea. Watch out, as aqueous (and sometimes the vitreous, too) humor is likely to spill out everywhere! Hopefully, the vitreous humor (aka vitreous body ) will remain intact enough not to “spill” out. Rather, most of it should be able to be extracted in toto . Continue the cut around the circumference of the oculus with scissors, being sure to maintain the ¼ inch distance back from the cornea.
Biology 241 – LAB #18 – continued Page Five
3.
Carefully separate the anterior and posterior portions of the oculus. (Again, the vitreous humor, or most of it, should stay with the posterior portion.)
4.
Examine the anterior portion of the oculus. Place a blunt probe between the lens and the ciliary processes and carefully lift the lens up a little. The “halo” of delicate transparent filaments between the lens and the ciliary processes is formed by the zonular fibers (aka suspensory ligaments of the lens ). Notice the ciliary body where the suspensory ligaments originate and the heavily pigmented iris with the pupil in its center.
5.
Remove the vitreous body in the posterior portion of the eyeball. Now, the retina is the tan-colored structure that is easily separated from the heavily pigmented choroid. Examine the optic disk where the retina attaches to the posterior of the oculus. You will notice that the retina does detach very easily (with the vitreous body absent) everywhere EXCEPT at the optic disk. (The choroid has a greenish-blue membrane, the tapetum lucidum , which improves night vision in animals such as sheep and cows; humans do not have this structure.)
Activity #3 : Visual Tests
Visual acuity refers to the sharpness of vision and is tested with a Snellen Eye Chart . This chart contains black letters of various sizes printed on white cardboard. Letters of a certain size are seen clearly by a person with normal vision at a given distance. A person with a visual acuity of 20/20 is considered to have normal ( emmetropic ) vision. The lines of letters are marked with numerical values such as 20/20, 20/30, 20/40 etc. A reading of 20/30, for example, indicates that you can see at 20 feet what an emmetropic eye can see at 30 feet; 20/30 vision is not as sharp as 20/20 vision. An eye that focuses an image in front of the retina is said to be nearsighted ( myopic ) and can see only close objects clearly. If an image is focused behind the retina, the eye is said to be farsighted ( hyperopic ) and can see only distant objects clearly. Corrective lenses are used to adjust for both conditions.
Astigmatism is a reduction in sharpness of vision due to an irregular cornea or lens. These uneven surfaces bend or refract light rays incorrectly, resulting in blurred vision. There is a chart to test for this, called the Astigmatism Chart, that consists of 12 sets of three lines laid out in a circular arrangement resembling a clock. We will NOT be performing the test for astigmatism.
I. Visual Acuity Test:
The Snellen Eye Chart , must be mounted on a wall at eye level, and a strip of masking tape will be placed on the floor to mark the distance of 20 feet from the chart. Perform this test in groups of two: one person stands next to the eye chart and indicates which line is to be read; the other is the “subject” and stands at the 20 foot mark to test his or her vision. Here is the procedure:
1.
The subject will stand at the 20-ft mark and cover one eye with the cupped eye-piece. Read a line where you can easily focus on all the letters. Continue to view lines of progressively smaller letters until you cannot accurately read them. Use the format suggested on the next page to record the value of the smallest line that can be read without errors. This line is your visual acuity for that eye.
2.
Repeat this process with your other eye. Again, record your data.
3.
Now, using both eyes, read the lowest line that you can see clearly. Record your data.
4.
If you wear glasses or contact lenses, repeat the test while wearing the corrective lenses. Again, record data.
Biology 241 – LAB #18 – continued
Recording format for Visual Acuity Test :
Acuity (without glasses) Acuity
Page Six
(with glasses)
Left eye:_____________________________ ___________________________________
Right eye:____________________________ ___________________________________
Both eyes:____________________________ ___________________________________
II. Blind Spot Mapping:
The optic disc , or blind spot, is an area of the retina lacking photoreceptors. Normally, one is not aware of these gaps in our vision because the visual fields of the eyes overlap and the brain uses a sophisticated process called filling in to deal with the absence of input from the blind spot. Here is the procedure:
1.
Hold the card (with the figures of a black cross and a black dot) provided at your Lab Table approximately 2
inches from your face.
2.
Close your left eye and stare at the cross with your right eye , keeping the cross in the center of your field of
vision.
3.
Slowly begin moving the card away from your face, increasing the distance. The dot will disappear when its
image falls on the blind spot of your right eye.
4.
Now, to check the blind spot in the left eye, close your right eye and stare at the dot with your left eye .
Repeat steps 1 – 3 with the card until the cross disappears due to its image falling on the blind spot of your
left eye.
III. Test for Accommodation
For objects closer than 20 feet from the eye, the lens must bend light rays together ( converge them ) so that they focus a sharp image on the retina. This process is called accommodation .
Objects 20 feet or further from the eye have parallel light rays that enter the eye. The ciliary muscle is relaxed, and the ciliary body is behind the lens. This causes the supensory ligaments to pull the lens flat for proper refraction of the parallel light rays. Objects closer than 20 feet to the eye have divergent or spreading light rays that require more refraction to focus them on the retina. Thus, the ciliary muscle contracts, and the ciliary body shifts forward, releasing the tension on the suspensory ligaments which causes the lens to bulge and beome rounded. The more spherical lens increases refraction, and the divergent rays are bent into focus on the retina. Reading and other activities requiring near vision cause eyestrain and fatigue because of the contraction of the ciliary muscle for accommodation. The lens gradually loses its elasticity as we age and causes a form of far-sightedness called presbyopia. Many individual have difficulty reading small type by the age of 40 andmay require reading glasses to correct for the reduction in accommodation.
Accommodation is determined by measuring the closest distance from which one can see an object in sharp focus; called the near point of vision. A simple test for near-point vision involves moving an object toward the eye until it becomes blurred. Here is the procedure:
1.
Hold a pencil, eraser-end up, approximately 2 ft from your eyes. Look at the ribs on the metal eraser casing.
2.
Close one eye and slowly bring the pencil toward your open eye.
Biology 241 – LAB #18 – continued Page Seven
3.
Measure the distance from the eye just before the metal casing blurs. Record your measurements in a format
as demonstrated below.
4.
Repeat the procedure with the other eye.
5.
To focus on near objects, the eyes must rotate medially, a process called convergence. To observe conver-
gence, stare at the pencil from arm’s length and slowly move it closer to your eyes. Which way do your eyes
move?
6.
Compare near-point distances with classmates of various ages. Record this comparative data.
7.
Why does accommodation change as we age?
Recording format for Near-Point Determination:
Right Eye Initials of Subject / Age
_________/_______________
_________/_______________
_________/_______________
_______________
_______________
_______________
Left Eye
_______________
_______________
_______________
Both Eyes
__________________
__________________
__________________