UNC Otolaryngology-Head & Neck Surgery Service Medical Student Information Handout
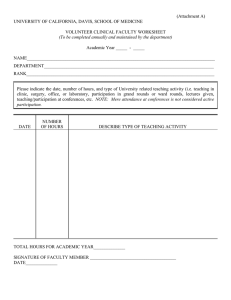
advertisement

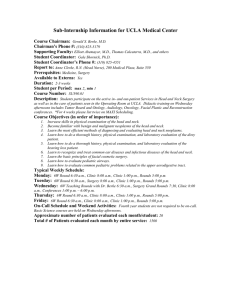
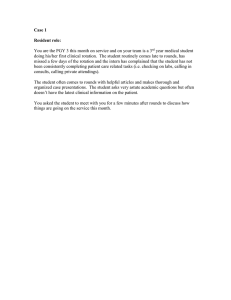
Revised May, 2015 - ASR UNC Otolaryngology-Head & Neck Surgery Service Medical Student Information Handout Welcome to the OTO-HNS service! We look forward to an educational and productive experience for each of you in caring for patients with diseases of the head and neck. While on our service, you will have the opportunity to learn about a wide range of problems while participating as a member of the team in the clinic, on the wards, and in the operating room. The administrative chief resident will be your primary resource person for questions regarding the schedule, end of rotation test, oral presentation expectations, call, and any problems that may occur during the course of the rotation. The overall objective of this rotation is to gain a broad based experience in our specialty. 3rd Year Medical Student Clerkship Director: Dr. Austin Rose Contact: austin_rose@med.unc.edu 4th Year Medical Student Clerkship Director: Dr. Adam Zanation Contact: azanatio@med.unc.edu The Department of Otolaryngology – Head & Neck Surgery and the Department of Surgery in The School of Medicine are both committed to fostering a respectful educational environment. If a student has concerns, the student is encouraged to meet with the Ombudsman for Students. This is a confidential meeting where a student may discuss a concern and learn about resources and procedures available to them. Education: A. The primary goal of your rotation on the OTO-HNS service is for you to learn about the diagnosis and treatment of patients with pathology of the head and neck. The attending and residents physicians have a commitment to excellence in education and consider teaching students a top priority. But, it is YOUR interest that will facilitate worthwhile and effective teaching and learning. B. One of the most effective teaching methods in medicine is asking questions, whether this is on morning rounds, in the operating room, in conference, or in clinic. We use this method liberally, so please read and be prepared. C. Additionally, we may ask students to look up articles or general information from textbooks to present succinctly on morning rounds. D. At the end of the rotation, each student is expected to give a concise 5 min oral presentation with a one-page handout to the team at morning rounds on a topic of their own choosing. Discuss this topic with one of the residents prior to preparation E. Your mandatory conferences take precedence over work on our service. Please excuse yourself to attend these at the appropriate time, however, there may be a rare occasion when you are an essential member of the operating team and are asked to stay for completion of a procedure. F. You are encouraged to seek out information from sources such as the textbooks in our library, and journal articles regarding more in-depth information on patients you Revised June, 2014 - ASR 2 see in the operating room and clinic. Here is a list of some online resources available to you: American Academy of Otolaryngology – Head & Neck Surgery Foundation (AAOHNSF) http://www.entlink.net/ Click on Clinical Otolaryngology OnLine (COOL) to learn about many high-yield areas of interenst to Otolaryngologists in training. Click on Core Education Curriculum as well. This is a curriculum designed especially for medical students. Online Journals: 1. Head & Neck journal http://www.interscience.wiley.com/ 2. Archives of Otolaryngology – Head & Neck Surgery http://archotol.ama-assn.org/ 3. Archives of Facial Plastic Surgery http://archfaci.ama-assn.org/ National Comprehensive Cancer Network http://www.nccn.org Here you will find evidence-based guidelines for the management of cancers in all sites, including head and neck, thyroid. There are also algorithms for management of cancer pain, nausea, and anemia. You can order a free CD-ROM online at this site. A must see site for all oncology-related education. Atlas of Head and Neck Pathology Department of Otolaryngology – Head & Neck Surgery Ohio State University Medical Center, William H. Saunders, MD http://medicine.osu.edu/oto/atlas.html Iowa Protocols http://wiki.uiowa.edu/display/protocols/Home Excellent source of information in our field. Otolarynoglogy Pictures http://www.ghorayeb.com/Pictures.html Great site to surf and see some great high-yield pictures. Otolaryngology/ Head & Neck Surgery University of North Carolina http://www.unc-ent.org/ Great links for learning more about the field of OHNS. Schedule: A. Please refer to the ENT master schedule on the resident room board for daily clinic schedules. The OR schedule will be sent via email each weekend and each night before the OR. If you have any questions regarding daily schedule, ask the administrative chief resident what activity would be most educational for that day. B. We offer a very flexible schedule with the goal of a broad based experience in ENT, but it does require the medical students to be proactive! We ask that you attend ORs and clinics in all of the following disciplines: Head and Neck Oncology, otology, 2 Revised June, 2014 - ASR 3 pediatric ENT, laryngology, facial plastic surgery and rhinology, aiming for about 3 OR days and 2 clinic days per week. C. The administrative chief resident may request your presence/help in the operating room or elsewhere if the need or a particularly educational experience arises regardless of the schedule. D. Third-year medical students must attend one half-day clinic with Dr. Rose, the clerkship director, during their rotation – ideally on either Tuesday morning or Thursday afternoon at the Carolina Crossing clinic (919-490-3280). Call Responsibilities: A. Call Requirements: For 3rd year medical students - Take call 1 night/week and 1 day/night combination your first weekend on service (either Saturday or Sunday) For non-AI 4th year medical students - Take call 1 night/week and 1 full weekend per 4-week rotation For AI 4th year medical students – We want you to call at least 1 night/week. We also expect 2 full weekends per 4-week rotation, depending on the number of AI students in a given block. B. When taking call, you will be expected to round with the call team in the evening and then stick around for any active consults, etc. that are occurring at that time. If nothing is in the works, the call team is allowed to leave the hospital. The junior resident on call will contact you for admissions, emergent operations, and ER cases that have educational merit. Call is HOME CALL. C. The student on call should contact the junior resident on call late in the day to find out when afternoon rounds will take place. On the weekends, contact the junior resident the night before to find out the time for morning rounds. Pre-rounding is not expected on the weekends. Rounds: A. Rounds begin promptly at: 6:45 AM * Pre-round on all of your patients and PLEASE BE THERE ON TIME. Head & Neck team rounds are at the discretion of the chief resident on the H&N Service. B. You will present your patients on cue from the administrative chief resident. Presentations will follow the SOAP format and should cover pertinent positives and negatives only. There is no time for superfluous information on morning rounds. Take this opportunity to refine your presentation skills into providing concise story while also providing accurate, yet necessary, information to the team. Sample presentations are provided below. Residents will be happy to assist you in your presentations if you ask for help. C. Ideally, all patients on the service should be covered by the students. We would expect that 3rd year medical students to cover 3-4 patients at a time, while 4th year medical students to cover 4-6 patients at a time. For 4th year medical students on their Critical Care rotation, you are expected to cover ALL ICU patients on our service, regardless of whether you were part of their operation or not. If you are a part of a patient’s operation, you are expected to follow that patient for the entire length of their hospital stay. 3 Revised June, 2014 - ASR 4 o At the end of the operation ask the resident what the pertinent exam findings will be to present on rounds the next morning. o If you are a 3rd year medical student and the patient will be staying in the ICU for a period of time post-operatively, make sure to ask the resident that you are working with if they would like you to see and follow the patient. o We expect “systems-based” presentations for all of the ICU patients. See example below. D. Pre-round on patients and have your proposed plan outlined in your mind or on paper so that you can provide the group with a streamlined presentation. It is a good idea to touch base with the resident following that patient in the am before rounds to discuss overnight events and the plan of care. E. Be sure to check lab work and LOOK at radiographic studies for your patients. Don’t rely solely on the radiology reports for X-ray interpretation; this is the time to start reading films, not your first night on call as an intern. F. Feel free to ask questions of the residents at anytime. If you have a question chances are your fellow students are wondering as well. Conferences: A. You are expected to attend all mandatory medical student conferences. Attend our conferences when there is not a scheduledconflict. The conference schedule will be on the week ahead email sent from the administrative chief resident. B. Conferences generally will be held in the 2nd floor Starbucks conference room or the ground floor POB conference room. C. 3rd year medical students will give a 5 minute oral presentation in rounds their last week on service. It is recommended that you discuss the topic with a chief resident. D. AI 4th year medical students will be expected to give a 20 minute Grand Rounds presentation at the end of their rotation. This will usually be their final Thursday on service. It is recommended that you discuss the topic with an attending (preferable) or a chief resident. BASIC SCHEDULE for ENT SERVICE Monday 6:45 AM morning rounds 7th floor Neuroscience Conference Room Tuesday 6:45 AM morning rounds 7th floor Neuroscience 5:00 PM Conference, TBD vs. Simulation Lab Wednesday 6:30 AM morning rounds 7th floor Neuroscience 6:45 AM AM Didactics, POB Conference Room 7:30 AM Grand Rounds, POB conference room 5:00 PM Conference, POB Conference Room Thursday 6:45 AM morning rounds 7th floor Neuroscience 4 Revised June, 2014 - ASR 5 Friday 6:45 AM morning rounds, 7th floor Neuroscience 7:00 AM Multidisciplinary Head and Neck Tumor Conference, Cancer Hospital Clinic: A. Ask the attending at the beginning of clinic how they would like you to interact with patients in terms of seeing them together, versus seeing them first and presenting them to the attending. B. Please treat the nurses and ancillary staff with an appropriate degree of respect and courtesy. They will do the same. C. Teaching heads are available for flexible fiberoptic laryngoscopes; ask the attending if you may use them for endoscopies. Several rooms have microscopes, video towers available as well. We also have a video stroboscopy machine that will be utilized. Don’t be afraid to use the otoscopes to look in patients’ ears. Ask one of the residents to show you how to perform an indirect mirror laryngoscopy. D. If you don’t know where something is, ask any of the residents. E. Dr. Rose requests that all third year students spend ½ clinic day with him during the rotation. F. Do not dispose of the green otoscope speculums, these are cleaned and reused. Sample presentations: A. (3yo s/p tonsillectomy and adenoidectomy for obstructive sleep apnea) S: Overnight no desaturations, or bleeding. The child is taking PO liquids well. O: AF,VSS with RR 16 and Sat 98% on room air Bilateral tonsillar fossa have eschar without blood clots, there is no epistaxis. There is no stridor, retractions, or use of accessory muscles of inspiration Lungs are clear to auscultation bilaterally, and the heart has a regular rate and rhythm A: s/p tonsillectomy and adenoidectomy doing well P: D/C home B. (56yo s/p total laryngectomy for larynx cancer) History: Mr. Jones is a 56yo male who presented with a 6 month history of odynophagia, and progressive hoarseness. He underwent a pandendoscopy 2 weeks ago that revealed a T4N1M0 squamous cell carcinoma of the larynx. 4 days ago he underwent a total laryngectomy with a right selective neck dissection levels 2, 3, and 4, and a left modified radical neck dissection sparing the spinal accessory nerve. His postoperative course has been complicated by ETOH withdrawal for which he is being treated with benzodiazepines. He is scheduled to have a gastrograffin swallow study on postoperative day 5. E. ICU Patient This is a 55yo male with a h/o a T3N2bM0 SCC of the oropharynx who is s/p failed chemoradiation therapy, now with persistent dz in the mouth and neck who is POD #2 s/p near total glossectomy and bilateral MRNDs as well as reconstruction with a radial forearm free flap. 5 Revised June, 2014 - ASR 6 Overnight, pt. had no issues. Nursing states that he rested well. He does seem to wake up at times and is appropriate. He remains on the ventilator. Flap checks were excellent through the night per the call team. VITALS: Give ranges over the course of the last day, not just numbers. Make sure to include I/Os. STUDIES: KUB last night confirmed NGT in good position after pt. pulled it partially out. CXR this AM with mild volume loss bilaterally at bases. Report on daily labs. NEURO: Awake, minimally sedated. Pain well-controlled per his reports. Follows commands appropriately Plan: wean off sedation fully to extubate, transition to PCA once more awake ENT: Intraoral skin paddle pink and warm with good cap refill, suture line intact with no dehiscence, external Doppler signals with good triphasic arterial signal with good venous hum and augmentation. Neck inicision c/d/I, no fluctuance or overlying skin changes. #8 cuffed tracheostomy tube in place, patent and secure x 4 sutures. JP drains in place in neck x 2 and holding suction, serosanguinous output. NGT suture secured to columella. Plan: Once off ventilator, take trach cuff down. Decrease Doppler checks to q 4 hours. Cont. wound cares with Vaseline and H2O2. Cont. absolute NPO, cont. NGT feeds. Consider removing JP drain #2 if output remains low throughout the day today. CV: RESP: Reg rhythm, mildly tachycardic, remains in NSR Plan: consider increasing his preoperative B-blockade dose, as BP and HR remain slightly elevated above normal. Consider better pain control first however to see if this is related to pain. Lungs CTA-B. CXR with some volume loss – likely atelectasis. No signs of any PNA however. Secretions from trach minimal. Wean from vent today. Recheck CXR in AM. Consider trach aspirate if spikes fever. Cont. routine trach cares by nursing – plan trach change on POD#5. FEN/GI: NGT in good position, suture-secured to columella. Bowel sounds positive, no abd distension. Cont. to increase TFs slowly to goal of 60ml/hr per nutrition recommendations. GU: Foley in place D/C foley once pt. more awake and able to use bedpan HEME/ID: Pt. with stable H+H since being transfused on POD#1. Slightly elevated WBC likely related to perioperative steroid use – trending down. No evidence of any soft tissue infection. Cont. Unasyn for clean-contaminated case for 7 day course. 6 Revised June, 2014 - ASR 7 ACTIVITY: Bedrest with HOB to 45 degrees Once off ventilator today, will get OOB to chair. PROPH: Cont. SQ heparin, TEDs and SCDs. Cont. Famotidine. DISPO: Likely transfer out of unit tomorrow. 7 Revised June, 2014 - ASR 8 2013/14 Medical Student Question Sheet (please make sure to hand this in to the Administrative Chief Resident at the end of the rotation) 1. What are the definitions of: a. Acute Otitis Media: b. Recurrent Otitis Media: c. Chronic Suppurative Otitis Media: 2. How do we stage cervical lymph nodes in carcinoma (“N” staging)? 3. What anatomical structures have to be traversed/dissected through when performing a tracheostomy? 4. What is a Sistrunk procedure and what are its indications? 5. Who is a candidate for a cochlear implant? 6. What are the three most common benign lesions of the glottis/true vocal cords? 7. What is the drainage pathway in the nose of the posterior ethmoid sinuses? Where is the distal opening within the nose of the lacrimal duct? 8. What are the different types of Basal Cell Carcinoma of the skin? 9. What are the different categories, based on AHI severity, of Obstructive Sleep Apnea (OSA)? 10. Describe the three main surgical approaches for resection of Vestibular Schwannomas? 8