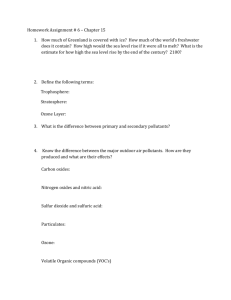
H . A
advertisement

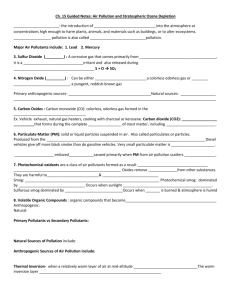
ENVR732-001 1 Fall 2009 HEALTH EFFECTS OF OUTDOOR AND INDOOR AIR POLLUTION. AN INTEGRATED INTERDISCIPLINARY APPROACH. ENVR 732, section 1. Dept. of Environmental Sciences and Engineering, School of Public Health, and Center for Environmental Medicine, Asthma and Lung Biology, School of Medicine 1. Class time: Fall semester, every Tue and Thu 9:30 - 10:45. 2. Classroom: McGavran-Greenberg #2304 3. Description No prerequisites. However, some knowledge of basic human physiology and biochemistry will greatly facilitate comprehension of the presented material. The course is a series of lectures on health effects of ambient criteria air pollutants (ozone, NOx, SOx, CO, particulates, lead) and selected indoor air pollutants with emphasis on the cardiorespiratory system. The students will gain an overall understanding of the health consequences of exposures to typical pollutant atmospheres as assessed by laboratory, field and epidemiological studies. Three credit hours. Fall semester. The course was developed to introduce you to such an important topic and area of public concern as the adverse health effects due to ambient and indoor air pollutants. It will help you to understand the basics of health problems associated with exposures to ambient, particularly "criteria" (regulated by EPA) air pollutants. To comprehend the interaction as well as interdependence of processes involved in identification and assessment of health hazards of environmental pollutants, the course material has integrated contributions of many disciplines, including physiology, cellular and molecular biology, immunology, genetics, dosimetry, etc. This approach should give you a good understanding of the health effects of air pollutants on normal and diseased human populations, including children. Furthermore, it will provide you with a solid framework for detailed studies of more specific areas of interest offered by the existing course program. 4. Instructor M. Hazucha, M.D., Ph.D., Center for Environmental Medicine, Asthma and Lung Biology (CEMALB), and Dept. of Medicine (Pulmonary), UNC 966-0770, mhazucha@med.unc.edu mail: Center for Environmental Medicine, Asthma and Lung Biology, Univ. of North Carolina, CB #7310 Chapel Hill, NC 27599-7310. ENVR732-001 Fall 2009 2 5. Faculty: N. Alexis, Ph.D., CEMALB, and Dept. of Pediatrics, 966-9915, Neil_Alexis@med.unc.edu W. Bennett, Ph.D., CEMALB and Dept. of Medicine (Pulmonary), UNC 966-6229, William_Bennet@med.unc.edu P. Bromberg, M.D.,CEMALB and Dept. of Medicine (Pulmonary), UNC, 966-0774, pwspar@med.unc.edu J. Carson, Ph.D., CEMALB, and Dept. of Pediatrics, UNC, and Dept. of Anatomy and Cell Biology, 966-0763, jcarson@med.unc.edu W. Cascio, M.D., Chief, Division of Cardiology, Brody School of Medicine at ECU, 252-744-0083, casciow@ecu.edu D. Diaz-Sanchez, M.D., Chief, CRB, NHEERL, US EPA, 966-0676, Diaz-Sanchez.David@epamail.epa.gov I. Gilmour, Ph.D., NHEERL, US EPA 966-0663, Gilmour.Ian@epamail.epa.gov I. Jaspers, Ph.D., CEMALB, UNC, 966-8657, ilona_jaspers@med.unc.edu S. Kleeberger, Ph.D., Director, Environmental Genetics Group, NIH, NIEHS, 541-3540, kleeber1@niehs.nih.gov M. Madden, Ph.D., NHEERL, US EPA and Dept. Environ. Sci. Eng., UNC 966-6257, Madden.Michael@epamail.epa.gov L. Neas, Ph.D., NHEERL, US EPA 966-9961, Neas.Lucas@epamail.epa.gov D. Otto, Ph.D., NHEERL, US EPA 966-6226, davidaotto@earthlink.net D. Peden, M.D., Director, CEMALB, Dept. of Pediatrics (Pulmonary/Allergy), UNC, 966-0768, David_Peden@med.unc.edu J. Rogers, Ph.D., Chief, Developmental Biology Branch, NHEERL, US EPA, MD-67 541-5177, Rogers.John@epa.gov J. Rosati, Ph.D., NHSRC, US EPA 541-9429, rosati.jacky@epa.gov G. Shoaf, Ph.D., NCEA, US EPA, B243-01 541-4155, Shoaf.Chon@epa.gov K. Yeatts, CEMALB, UNC, 843-1841, kyeatts@med.unc.edu Should any student wish to discuss the presented and related material of the course, please contact the respective faculty member and make an appointment. 6. Grading: The final grade (average of three exams) for this course follows The Gradual School Handbook grade scale (p. 7). However, each exam question will be graded according to a percentage scale below. The grades will be normalized by the instructor. The following criteria will be used by the faculty as a guideline to grading essay questions. 95-100% (H) Clear mastery of the question; precise and concise organization; depth and scope of discussion ideally suited to the question; if applicable, some evidence of creative insight and an ability to deal with controversies and reservations. ENVR732-001 Fall 2009 3 80-94% (P) Facts are accurate; evidence of reasonable depth of knowledge; evidence that the major issues involved are clearly understood; well-organized; answer contains a judicious selection of available facts. 60-79% (L) A few factual errors; major issues are covered but not in depth; good but not outstanding organization; barely satisfactory. 50-59% (F) Several factual errors; superficial coverage of the area; coherent but weak organization; although the answer is partially correct, it lacks accuracy and completeness. 31-49% (F) Evidence of major gaps in the area; organization so poor that the answer may be difficult to follow; clear evidence of misunderstanding of major issues. 0-30% (F) Either doesn't answer the question, or clearly demonstrates no understanding of the issue. 7. Reference texts and books (at the reserve desk in the Health Sciences Library): There is no required textbook, but if you can afford it get the book by Holgate et al. Air Pollution and Health, 1999. Most of the lectures material comes from this book. The course required reading material consists of selected references and, for some lectures, handouts to be distributed before a lecture. The required references can accessed through HSL Electronic Reserves. The password will be given to you during the first lecture. Additional suggested reading material (reviews, chapters, and articles) has been selected from books and journals available in the HSL. For those who wish to expand their knowledge of a topic selected books listed below are on reserve for this course in the HSL as well. Books/Reports: 1. Holgate,S.T., Koren,H.S., Samet, J.M., and Maynard,R.L., eds., Air Pollution and Health. London, UK: Academic Press, 1999. WA754 A29795 1999 2. W. M. Foster, D. L. Costa, eds. Air pollutants and the respiratory tract. Boca Raton : Taylor & Francis/CRC Press, 2005. WF 140 A2978 2005 3. Jane Q. Koenig. Health effects of ambient air pollution : how safe is the air we breathe? Boston : Kluwer Academic, 2000. WA 754 K78h 2000 4 M. D. Cohen, J. T. Zelikoff, R. B. Schlesinger,eds. Pulmonary immunotoxicology . Boston : Kluwer Academic Publishers, 2000. WF 600 P98349 2000 5. Levitzky, M. G. Pulmonary Physiology. New York: McGraw-Hill, Inc. Health Professionals Division, 1999, p. 1-299. WF600 L666p 1999 6. Amdur, M.O., Doull, J., Klaassen C.D., eds. Casarett and Doull's Toxicology. The Basic Science of Poisons. New York: McGraw-Hill, Inc., 1996, p. 1-1033. QV600 C335 1996 7. Lipfert, F.W. Air Pollution and Community Health. New York: Van Nostrand Reinhold, 1994, p. 1556. WA754 L764a 1994 8. M. Lippmann. Environmental toxicants : human exposures and their health effects / Edition 2nd ed. New York : Wiley-Interscience, 2000. WA 671 E6105 2000 9. D. E.Gardner, J. Crapo, R. O. McClellan , eds.Toxicology of the Lung. New York: Raven Press, 1999, p.1-672. WF600 T755 1999 ENVR732-001 Fall 2009 4 10. Air Quality Criteria for Ozone and Related Photochemical Oxidants. 05/004a-c /, Vol. III, 2006. US EPA, EPA/600/R- 11. EPA document. Air quality criteria for carbon monoxide. EPA 1.23/6:600/P-99/001 F 12. Ayers, J, Maynard R, Richards, R., eds., Air Pollution and Health. London, UK: Imperial College Press, 1999. WA754 A29794 2006 13. P. Brimblecombe, R. L. Maynard, eds. The urban atmosphere and its effects London ; River Edge, NJ : Imperial College Press, 2001. WA 754 U722 2001 14. P. Witorsch, S. V. Spagnolo, eds, Air pollution and lung disease in adults. Boca Raton, Fla. : CRC Press, 1994. WF 600 A2975 1994 15. M. Krzyzanowski, B. Kuna-Dibbert and J.Schneider, eds., Health effects of transport-related air pollution. Copenhagen : World Health Organization Europe, 2005. WA 754 H4343 2005 16. D.L. Dungworth .et al. eds., Relationships between respiratory disease and exposure to air pollution. Washington : ILSI Press, 1998. WA 754 R382 1998 17. D. G. Penney, ed., Carbon monoxide toxicity, Boca Raton ; CRC Press, 2000. QV 662 C2647 2000 ENVR732-001 Fall 2009 5 Class calendar: Aug. 25 ---Introduction: Course objectives, structure, exams, readings; History of air pollution and health. M.J.Hazucha ............................................................................7 Aug. 27 --- Anatomy and physiology of the human respiratory tract: aspects relevant to systemic and respiratory effects of air pollution. P.A.Bromberg ..........................................................................9 Sept. 1 --- Methods in assessment of sensory and organ effects, and pulmonary function changes induced by air pollutants. M. J. Hazucha .......................................................................................................10 Sept. 3 --- Biological markers. Interdisciplinary methodologies for assessment of adverse health effects. M. Madden ..........................................................................................................................................11 Sept. 8 --- Cellular responses and mechanisms of pollutant-induced effects. I. Jaspers ...............................12 Sept. 10 --- Dosimetry of inhaled gases and particulates. W. Bennett ..............................................................13 Sept. 15 --- Health effects of particulate matter: laboratory studies. W. Bennett .............................................14 Sept. 17 --- Epidemiology in assessment of health effects of air pollutants. K. Yeatts ....................................15 Sept. 22 --- Gene-air pollutants-health interaction. S. Kleeberger ....................................................................17 Sept. 24 --- Immuno-toxicological effects of air pollutants. M. I. Gilmour .....................................................18 Sept. 29 --- Animal toxicology. Interspecies comparison and extrapolation of the effects of air pollutants to man. M. I. Gilmour .......................................................................................................................19 TAKE HOME EXAM Oct. 1 ---Controlled human exposure studies in assessment of health effects of ir pollutants. N Alexis ......20 Oct. 6 --- Mucociliary function and mechanisms of cellular damage and repair in the respiratory airways.. J.Carson .........................................................................................................................................22 Oct. 8 --- Diesel exhaust and organic compounds health effects. I. Jaspers .................................................24 Oct. 13 --- Health Effects of Airborne Particulate Matter: Epidemiology Studies. L. Neas ...........................25 Oct. 15 --- Adverse health effects of indoor air (biological aerosols, home environment).J. Rosati ..............26 Oct. 20 --- Acute effects of ozone; laboratory studies. Biochemical and immunotoxic effects. N. Alexis .....27 Oct. 22 Fall recess Oct. 27 --- Acute effects of ozone; laboratory studies. Systemic and lung function effects. M.J.Hazucha ....28 Oct. 29 --- Sulfur dioxide and its products: Effects on sensitive individuals. P.A.Bromberg .......................29 ENVR732-001 Nov. Fall 2009 6 3 --- Health effects of nitrogen oxides. M.J.Hazucha ...........................................................................31 TAKE HOME EXAM Nov. 5 --- Kinetics, mechanisms of action and health effects of exposure to CO. M.J.Hazucha ..................32 Nov. 10 --- Health impacts of secondhand smoke. D. Diaz-Sanchez ...............................................................33 Nov. 12 --- Systemic poisons; Lead and other metals. D. Otto ......................................................................34 Nov. 17 --- Health effects of pollutants mixtures. P.A. Bromberg ...................................................................35 Nov. 19 --- Cardiovascular effects of air pollutants. W. Cascio .......................................................................37 Nov. 24 --- Asthma and allergic disease. D. Peden .........................................................................................38 Nov. 26 Thanksgiving recess Dec. 1 --- Approaches and challenges in health risk assessment. C. Shoaf ..................................................39 Dec. 3 --- Protection of susceptible population. P.A. Bromberg ....................................................................40 Dec. 8 --- Developmental and reproductive toxicology. J. Rogers ................................................................41 FINAL TAKE HOME EXAM ENVR732-001 Aug. 25 I. Fall 2009 7 ---Introduction: Course objectives, structure, exams, readings; History of air pollution and health. M.J.Hazucha Introduction: A. Course objective B. Structure of the course C. Exams II. History, standards and trends: A. Definition Air pollution means the presence in the outdoor atmosphere of one or more contaminants, such as dust, fumes, gas, mist, odor, smoke, or vapor in quantities, of characteristics, and duration, such as to be injurious to human, plant, or animal life or to property, or which unreasonably interferes with the comfortable enjoyment of life and property (The Engineer=s Joint Council). B. Significant dates in the history of air pollution 1280 Henry III asks London city official to Ainquire about lime kilns using seacoal@ 20th May 1285 1300 Coal for manufacturing hauled to London from Newcastle (~300 miles, county of Durham). 1306 EDWARD I prohibits use of coal during a session of Parliament (died in 1307). Followed by Edward II, Richard III. 1418 HENRY V establishes Commision of Inquiry to Ainquire of all such who burn coal in the city.....and to punish them with great fines and ransoms, 2nd offence to demolish their furnaces@. 1556 G. AGRICOLA=s 12 volumes ADe Re Metallica@ published. ANew age@ , renaissance of arts and revival of learning (Copernicus, Leonardo da Vinci, Vesalius, Paracelsus). Work translated by Herbert Hoover, the president. 17th century Sweden. Legislation forbidding Aslash and burn land clearing@. Those who broke the law were banished to the New World. 1661 J. EVELYN=s pamphlet AFumifugium@ publ. by royal command of Charles II. J.E. was founder of the Royal Society. 1713 B. RAMAZZINI=s book ADe Morbis Artificum@ (43 chapters) is published 1819 1st English Select Committee of the British Parliament established to study and report upon smoke abatement. 1843 2nd English Select Committee established 1845 Parliament passed the law requiring locomotives to consume their own smoke. 1863 Alkali Act established industrial smoke inspectors in Britain 1866 1st paper on effects on health due to air pollution by W.Farr 1875 Cattle death at London show due to air pollution 1881 (USA) Local smoke ordinances passed in Chicago and Cincinnati declaring the emissions of smoke to be a public nuisance. Required that Afurnaces consume the smoke produced or employ devices that would do so.@ Principal fuel was coal. County-wide legislation to control AP in 1920, state-wide 1960, federal 1963. 1891 (USA) Society for Prevention of Smoke established in Chicago (predecessor of APCA) published model smoke abatement ordinances to help communities in drafting legislation. C. Significant events 1930 MEUSE VALLEY, Belgium (Dec. 1-5). 63 excess death, 6000 ill. Est. 0.1-10 ppm SO2, zinc, PM, but most likely fluorides. 1937 15-month mobile survey of SO2 levels in 5 cities 1943 1st severe smog in LOS ANGELES (July 26) 1947 California establishes first state regulation 1948 DONORA, PA, disaster (Oct.27- Nov. 1) 20 fatalities; 2 days-60 sick, next 2 days-750, last day 1600 (total 5910). 10-week avg. 0.12 ppm SO2, 740 μg/m3 PM, 85 μg/m3 zinc. TSP max was 6000 μg/m3. Strong contribution by fluorides. 1952 LONDON disaster (Dec. 5-10) 4000 excess death; 4000 μg/m3 SO2 and smoke. Mostly older individuals. 1953 NEW YORK episode (Nov. 17-21). First reported in 1962. 200 excess death. ENVR732-001 8 Fall 2009 D. Clean Air Act - Britain (1956) E. Clean Air Act - USA (1963) Purpose to publish and to revise from time to time a list of air pollutants to establish Air Quality Standards (NAAQS) # Primary standards - set at levels which protect not only healthy but sensitive persons as well - to be established using health protection as the sole test # Secondary standards - defines the components of public welfare that must be considered - must protect against any type of adverse effect State Implementation Plan Dispersion Techniques New and Modified Sources Prevention of Deterioration Mobile sources F. US primary standards U.S. NATIONAL PRIMARY AMBIENT AIR QUALITY STANDARDS POLLUTANT ppm Carbon Monoxide (CO) Lead (Pb) Nitrogen Dioxide (NO2) Particulate Matter (PM10) 9 35 0.053 (PM2.5) Ozone (O3) Sulfur Dioxide (SO2) 0.12 0.075 0.03 0.14 μg/m3 10,000 40,000 1.5 100 50 150 15 65 235 157 80 365 AVERAGING TIME STATISTICS 8 hours 1 hour 3 months Annual Annual 24 hours Annual 24 hours 1 hour 8 hours Annual 24 hours Maximum Maximum Quarterly avg. Arithmetic mean Arithmetic mean Maximum, multiple exceed. 99 percentile Maximum Arithmetic mean Maximum G. Classification/categorization of air pollutants 1. For regulatory purposes Criteria pollutants are those substances deemed to present a general risk to public heatlh and for which National Ambient Air Quality Standards (NAAQS) have been issued. Criteria pollutants are ozone, nitrogen dioxide, sulfur dioxide, lead, carbon monoxide, and particulate matter. Hazardous air pollutants or air toxics are those substances identified with cancer, birth defects, neurotoxicity and for which ambient standards are neither appropriate nor practical. (Adapted from Lipfert, 1994). 2. By chemical properties AClassical,@ reducing, London-type - SOx, PM, CO - winter months, early morning - industrial and household fuel combustion APhotochemical,@ oxidizing, Los Angeles-type - ozone, HC, CO, NOx - summer months, early afternoon - motor vehicle fuel combustion H. Trends in ambient air quality Required reading: Ross Anderson, H., Health effects of air pollution episodes, In: Air Pollution and Health, Eds. Holgate,S.T., Koren,H.S., Samet, J.M., and Maynard,R.L., Academic Press, London, UK, 1999, Ch. 21, pp. 461-482. ENVR732-001 Fall 2009 9 Aug. 27--- Anatomy and physiology of the human respiratory tract: aspects relevant to systemic and respiratory effects of air pollution . P.A.Bromberg For detailed description see Bromberg_FunctAnat.pdf at HSL reserves site ENVR732-001 Fall 2009 10 Sept. 1 ---Methods in assessment of sensory and organ effects, and pulmonary function changes induced by air pollutants. M. J. Hazucha I. Subjective Symptoms Methods for obtaining and evaluating symptoms. II. Respiratory System 1. Static lung volumes and capacities (spirometry) 2. Lung dynamic tests (flow-volume) 3. Lung mechanics (plethysmography, airway resistance) 4. Gas exchange (diffusion, blood gases) 5. Control of ventilation (breathing pattern, exercise) 6. Bronchial Challenge Testing III. Central Nervous System 1. ECG, evoked potentials 2. Olfaction 3. Ocular 4. Acoustic IV. Cardiovascular System 1. Blood Pressure 2. Cardiac Output 3. Electrocardiogram 4. Peripheral Blood Flow V. Other Organs Systems ENVR732-001 Fall 2009 11 Required reading: Handout Materials Optional Reading: 1. Ruppel, G.L. Manual of Pulmonary Function Testing St. Louis: Mosby, 1991 2. Cotes, J.E. Lung Function: Assessment and Application in Medicine. Oxford: Blackwell Scientific, 1993. ENVR732-001 Fall 2009 12 Sept. 3 ---Biological markers; Interdisciplinary methodologies for assessment of adverse health effects. M. Madden I. Definition/Types of “Biomarkers” A. Exposure B. Effect C. Susceptibility II. Rationale for Study of Biomarkers and Utility of Biomarkers III. Time course of biomarker formation IV. Biomarkers of effects: Body Compartments of Interest: A. Whole Lung Physiology B. Breath C. Nasal and Lung Lavage D. Lung Cells & Tissue E. Extrapulmonary Systems (Blood, Urine, Skin) V. Susceptibility Biomarkers Required reading: 1. Madden, M. and Gallagher, J.E. Biomarkers of exposure. In: Air Pollution and Health, Eds. Holgate,S.T., Koren,H.S., Samet, J.M., and Maynard,R.L., Academic Press, London, UK, 1999, Ch. 19, pp. 417-430 2. Henderson, R. and S.A. Belinsky. Biological markers of respiratory tract exposure. In:D.E. Gardner, J.D. Crapo, R.O. McClellan, eds. Toxicology of the Lung, second edition. Raven Press, New York. 1993. pp 253-282. Optional Reading: 1. Papers from a symposium on biomarkers from air toxics exposure. Environ Health Persp 104, Suppl 5: 851932, 1996. 2. La, D.K., and J.A. Swenberg. DNA adducts: biological markers of exposure and potential application to risk assessment. Mutation Res. 365:129-146. 1996. 3. Virchow, J.C. Jr., C. Kroegel, C. Walker, H. Matthys. Cellular and immunological markers of allergic and intrinsic bronchial asthma. Lung. 172:313-334. 1994. 4. Lewtas, J. Human exposure to complex mixtures of air pollutants. Toxicol. Lett. 72:163-169. 1994 5. Gonzalez, F.J., and H.V. Gelboin. Role of human cytochrome P-450s in risk assessment and susceptibility to environmentallt-based disease. J. Toxicol. Environ. Health. 40:289-308. 1993. 6. Vine, M.F. Biological markers of exposure: Current status and future research needs. Toxicol. Ind. Health 12:189-200, 1996. ENVR732-001 Fall 2009 13 Sept. 8--- Cellular responses and mechanisms of pollutant-induced effects. I. Jaspers 1. Pollutant-induced injury i. Inflammation ii. Inflammatory mediator production iii. Comparison of different pollutants 2. General Signal Transduction Concepts 3. Generation of Oxidative Stress i. Increased production of ROI ii. Antioxidant defenses iii. Air pollutant examples 4. Signaling Pathways Activated by Oxidant Pollutants i. Transcription factors 1. General 2. Examples: NF-kB, AP-1, CREB ii. Protein Kinases 1. General Classification 2. PKA 3. MAP kinases 4. Tyrosine kinases a. Receptor Tyrosine Kinases (EGFR) b. Non-receptor Tyrosine Kinases iii. Arachidonic Acid Metabolism Required Reading: 1. B. Baeza-Squiban, V. Bonvallot, S. Boland, F. Marano. Airborne Particles evoke an inflammatory response in human airway epithelium. Activation of transcription factors. Cell Biology and Toxicology 15: 375-380, 1999 2. M.T. Krishna, A.J. Chauhan, A.J. Frew, S.T. Holgate. Toxicological Mechanisms Underlying Oxidant Pollutant-induced Airway Injury. Reviews in Environmental Health. 13: 59-71, 1998 ENVR732-001 Sept. 10 Fall 2009 14 ---Dosimetry of inhaled gases and particulates. W. Bennett Gases I. Characterization of gases solubility (e.g., SO2) and reactivity (e.g., O3) II. Factors affecting distribution of gas uptake in the respiratory tract breathing pattern, oral vs. nasal breathing, adsorption on particles, species differences III. Methods for measuring gas uptake Particulates I. Aerosol characterization size distributions, concentration, hygroscopicity, surface properties II. Mechanisms of particle deposition in the respiratory tract impaction, sedimentation, diffusion, and interception III. Techniques for measuring particle deposition and clearance IV. Factors affecting total and regional pulmonary deposition particle size, breathing pattern, airway morphology, species differences, lung disease V. Particle clearance mechanisms A. Mucociliary and cough clearance B. Alveolar clearance macrophages, dissolution, soluble vs. insoluble particles, ultrafines VI. Factors modifying clearance kinetics age, disease, overload, co-pollutants, Required reading Morgan MS and R Frank. Uptake of pollutant gases by the respiratory system. In: Respiratory Defense Mechanisms, part 1, eds JD Brain, DF Proctor, and LM Reid; New York: Marcel Dekker, 1977, pp. 157189. Bennett WD and JS Brown. Particulate Dosimetry in the Respiratory Tract. In Air Pollutants and the Respiratory Tract, ed Foster and Costa, Marcel Dekker, Inc. NY, NY, 2005. Optional Reading Overton JH and FJ Miller. Absorption of Inhaled Reactive Gases. In: Toxicology of the lung. Eds., Gardner DE, Crapo JD and Massaro EJ; New York: Raven Press, 1988, pp. 477-507. Swift, D.L. Aerosol characterization and generation. In: Aerosols in Medicine. Principles, diagnosis and therapy, eds Moren, F., Newhouse, M.T., and Dolovich, M.B. Amsterdam, Elsevier Science Publishers, 1985, pp. 53-63. ENVR732-001 Sept. 15 Fall 2009 15 --- Health effects of particulate matter: laboratory studies. W. Bennett I. Sources and Limits - Environmental (EPA) and some Occupational (OSHA) A. chemical composition of ambient air B. complex mixture C. size distributions--Coarse vs. Fine vs. Ultrafine Mode II. Factors influencing toxicity A. Particle characteristics - Acidity, surface coatings, size and shape, concentration B. Interactions with other pollutants C. Population characteristics - compromised health, age, dosimetry III. Particle toxicity studies A. Animal vs. Human and Acute vs. Chronic B. Health effects endpoints – cardiopulmonary pathophysiology carcinogenic/genotoxic as applicable to the following particulate matter: 1. PM10 (complex mixture) 2. Acid sulfates 3. Ultrafine particles 4. Metals 5. Diesel Exhaust 6. Silica 7. Asbestos and inflammation,, ENVR732-001 Fall 2009 16 Required reading 1. Pooley, F.D. and M. Mille. Composition of Air Pollution Particles. In: Air Pollution and Health, eds. Holgate, S.T. et al., San Diego, CA: Academic Press, Inc., 1999, pp. 619-634. 2. Frampton MW, Utell MJ, and JM Samet. Cardiopulmonary Consequences of particle inhalation. In:Particle-Lung Interactions, eds. Gehr and Heyder. N.Y., N.Y.: Marcel Dekker, Inc. 2000, pp. 653-670. Optional Reading 1. Utell, M.J., and M.W. Frampton. Particles and mortality: a clinical perspective. Inhalation Toxicology 7:645-655, 1995. 2. Ghio, A., and J.M. Samet. Metals and air pollution particles. In: Air Pollution and Health, eds. Holgate, S.T. et al., San Diego, CA: Academic Press, Inc., 1999, pp 635-651. 3. MacNee, W., and K. Donaldson. Particulate Air Pollution:injurious and protective mechanisms in the lungs. In: Air Pollution and Health, eds. Holgate, S.T. et al., San Diego, CA: Academic Press, Inc., 1999, pp 653671. ENVR732-001 Fall 2009 17 Sept. 17---Epidemiologic approaches to assessment of acute and chronic health effects of air pollutants. K. Yeatts I. Introduction A. Examples: London Fog, Atlanta Olympics B. Observational vs experimental studies C. Target populations, sampling, and bias II. Measures of Health Outcomes A. Mortality 1. Overall and cause-specific B. Morbidity 1. Symptoms, lung function, and illness 2. Methods of assessment (e.g. questionnaires, diaries, medical records, Medicaid billing records) III. Measurement of Exposure (Units of exposure, sources/substances) A. Ecologic B. Individual a. Personal monitoring b. Indoor Home monitoring c. Outdoor home monitoring G. Designs/methods for effects from different sources/substances IV. Study Designs A. Ecologic Studies B. “Natural Experiments” C. Cross-sectional (example Stern 1994) D. Time series (examples Pope 1989, Schwartz 1992) E. Cohort (examples Dockery 1993, Pope 1991, Pope 1993) F. Case Cross Over (example Bateson, 2004) G. Panel Studies (example Pope, 2004) H. Advantages and disadvantages V. Relation of Exposures and Health Outcomes A. Measures of association (e.g. relative risk) B. Covariates (confounders and effect modifiers) VI. Difficulties A. Multiple exposures and covariates B. Non-specificity of responses and relatively small effects Required Reading: 1. Dockery D.W. Epidemiologic Study Design for Investigating Respiratory Health Effects of Complex Air Pollution Mixtures. Environ Health Perspect 1993;101 (Suppl 4):187-191. Optional Reading: 1. Samet J.M. and Speizer F.E. Assessment of Health Effects in Epidemiologic Studies of Air Pollution. Environ. Health Perspect. 1993;101 (Suppl 4):149-154. ENVR732-001 Fall 2009 18 2. Pope C.A. Respiratory Disease Associated with Community Air Pollution in a Steel Mill, Utah Valley Am. J. Public Health 1989; 79:623-628. 3. F.W. Lipfert. Air Pollution and Community Health. Van Nostrand Reihold, 1994,New York, ch. 6-10, p.14243. 4. Bateson TF, Schwartz J. Who is sensitive to the effects of particulate air pollution on mortality? A casecrossover analysis of effect modifiers. Epidemiology 2004;15:143-149. 5. Pope CA, Hansen ML et al. Ambient Particulate air pollution, heart rate variability, and blood markers of inflammation in a panel of elderly subject. Environ Health Perspect 2004; 112:339-345 6. Friedman MS et. Impact of Changes in Transportation and Commuting Behaviors During the 1996 Summer Olympic Games in Atlanta on Air Quality and Childhood Asthma. JAMA 2001; 285:897-905. ENVR732-001 Fall 2009 19 Sept. 22 ---Gene-air pollutants–health interaction. S. Kleeberger One of the most challenging problems in modern biomedical research is to gain an understanding of the causes of human diseases. Growing concern has also focused on the role of host factors in the disease process. For example, while it is well established that air pollutants such as ozone may cause inflammation and decrements in pulmonary function, it is also apparent that it is very selective in whom it “chooses” to cause these effects. Why are some people affected while others are seemingly spared, despite apparently similar exposure? In other words, what are the causes of differential susceptibility to diseases and toxic agents in the population? I. Susceptibility factors in disease pathogenesis 1. Cultural and economic milieus 2. Gender and developmental processes (i.e. age and epigenetic processes) 3. Pre-existing Disease 4. Genetic background II. The role of genetic background in human lung disease 1. Inter-individual variation in response to air pollutants 2. Twin studies 3. Familial association III. Animal models of genetic susceptibility to air pollution-induced pulmonary injury 1. Methods and approaches 2. Examples: ozone, particulate matter IV. Translational studies and examples of genetic susceptibility in human populations. 1. Genetic association in clinical studies 2. Genetic epidemiological studies Required reading: 1. Ober C. Perpectives on the past decade of asthma genetics. J Allergy Clin Immunol 116:274-278, 2005. 2. Kleeberger SR, Peden D. Gene-environment interactions in asthma and other respiratory diseases. Ann Rev Med 56:383-400, 2005. Additional/Optional Reading: 1. Kleeberger SR. Genetic aspects of susceptibility to air pollution. Eur Resp J 21 (suppl 40):52s-56s, 2003. 2. Nebert DW. Inter-individual susceptibility to environmental toxicants – A current assessment. Toxicol Appl Pharmacol, in press 2005. ENVR732-001 Fall 2009 20 Sept. 24 --- Immuno-toxicological effects of air pollutants. M. I. Gilmour I. Overview of the immune system A. Nonspecific host defenses B. Specific host defenses II. Protection against disease A. Bacterial infections B. Viral infections III. Hypersensitivity responses A. Hay fever and asthma B. Delayed type hypersensitivity reactions IV. Immunotoxicology testing A. Tier 1 testing B. Tier 2 testing V. Interpretation of immune function data A. Model choice B. Correlation and risk assessment VI. Examples of air pollutant immunotoxicity A. Increase risk of infection B. Increase allergic lung disease C. Systemic effects Required Reading: 1.Burns, L.A.., Meade, B.J., and Munson A.E., Chapter 12: Toxic responses of the immune system. Casarett and Doull’s Toxicology: The Basic Science of Poisons. pp. 355-402, 1996. Optional Reading: 1.Luster et al. Development of a testing battery to assess chemical-induced immunotoxicity. Fund. Appl.Toxicol. 10:2-19, 1988. 2.Luster et al. Risk assessment in immunotoxicity. Fund. Appl. Toxicol. 18:200-210, 1992. ENVR732-001 Fall 2009 21 Sept. 29--- Animal toxicology. Interspecies comparison and extrapolation of the effects of air pollutants to man. M. I. Gilmour I. Purpose of extrapolation modelling A. Animal study limitations and uncertainty factors B. Toxicology requirements C. Calculating risk II. Advantages of animal studies A. Methodology (control of exposure C & T variables; availability of strain and genetically engineered animals; access to tissues and choise of biologic endpoints; mechanism) B. Acute studies (concentration / dose -response; interactions) C. Chronic studies (scenarios and duration) III. Dosimetry IV. Interspecies comparisons of normal lung structure and function A. Basic architecture: morphology vs. morphometry B. Physiologic scaling (growth, aging) C. Clearance mechanisms D. Biochemistry V. Interspecies comparisons of health effects of air pollutants A. Biomarkers in humans and animals after ozone exposure B. Effects of ozone on host defenses in mice and men VI. Extrapolation modelling from in vitro data to in vivo situations A. Parallelogram design B. Ozone and alveolar macrophage function C. Extrapolation to phosgene VII. Risk assessment paradigm Required Reading: 1. Selgrade, M.K., et al. Immunotoxicity: Bridging the gap between animal research and human health effects. Fund. Appl. Toxicol. 24:13-21, 1995. 2. Warheit, D.B. Interspecies comparisons of lung responses to inhaled particles and gases. Toxicology. 20(1):1-29, 1989. Criteria reviews in Optional Reading: 1. Comparative Biology of the Normal Lung. Ed: R.A. Parent. CRC Press, Boca Raton, FL. 1991. (Good reference for comparative evaluations of structure, function, biochemistry of the lung. 2. Extrapolation of Dosimetric Relationships for Inhaled Gases and Particles. J Toxicol and Environ Health 13: Symposium Proceedings (1984). 3. Tepper, J.S., Costa, D.L., and Lehmann JR. Extrapolation of Animal Data to Humans: Homology of Pulmonary Physiological Responses with Ozone Exposure. Toxicology of the Lung. Ed. D.E. Gardner et al., Raven Press Ltd. NY, 1993. 4. Schlesinger, R.B. The interaction of inhaled toxicants with respiratory tract clearance mechanisms. Critical reviews in Toxicology. 20(4):258-285, 1990. TAKE HOME EXAM ENVR732-001 Fall 2009 22 Oct. 1 ---Controlled human exposure studies in assessment of health effects of air pollutants. N. Alexis I.Introduction/Background Put into perspective what has been covered to date (i.e. Historical perspective of air pollution; Anatomy and physiology of respiratory system; Methods to assess outcomes) Introduce today’s topic as a transition from previous topics II.Purpose of Today’s Lecture Introduction to controlled human exposure experiments III.Research Approaches Controlled human exposure studies Translational research approaches IV.Strengths and Limitations Strength: Has the ability to hold all things constant except for the exposure of interest – can isolate on exposure Limitation: Can only study “reversible” effects V.Ethical Considerations Risk vs. Benefit Analysis Informed Consent Right to Withdraw VI.Utility of Controlled Human Exposure Studies To determine if a pollutant causes a particular health effect vs. exacerbates an existing effect To figure out the mechanism underlying the response VII.Exposure Facility Requirements Generate the pollutant, monitor it, and control its concentration Maintain your target concentration with acceptable variation I.Control the environmental variables II.Regulate the temperature, relative humidity, air exchanges – concerned with subject comfort VIII.Study Designs Clear statement of question Clearly formed and testable hypothesis IX.Subject Phenotype Do you study healthy or diseased X.Exposure Protocol Are you trying to establish a realistic exposure pattern – is it required ? XI.Outcome Measurements Anthropogenic data / Clinical parameters Inflammation XII.Data Collection and Management Need a centralized protected system Open and responsive to validation and quality assurance scrutiny ENVR732-001 Fall 2009 23 Required reading: Holz O, Jorres RA, Timm P, Mucke M, Richter K, Koschyk S, Magnussen H. Ozone-induced airway inflammatory changes differ between individuals and are reproducible. Am J Respir Crit Care Med. 1999 Mar;159(3):776-84. Folinsbee, L.J. Human clinical inhalation exposures: experimental design, methodology, and physiological responses. In: Toxicology of the Lung. D.E. Gardner, J.D. Crapo, E.J. Massaro, eds. Raven Press, NY, pp. 175198, 1988. Optional reading Alexis NE, Becker S, Bromberg PA, Devlin R, Peden DB. Circulating CD11b expression correlates with the neutrophil response and airway mCD14 expression is enhanced following ozone exposure in humans. Clin Immunol. 2004 Apr;111(1):126-31 Lay JC, Alexis NE, Kleeberger SR, Roubey RA, Harris BD, Bromberg PA, Hazucha MJ, Devlin RB, Peden DB. Ozone enhances markers of innate immunity and antigen presentation on airway monocytes in healthy individuals. J Allergy Clin Immunol. 2007 Jun 20 ENVR732-001 Oct. 6 Fall 2009 24 ---Mucociliary function and mechanisms of cellular damage and repair in the respiratory airways. J.Carson I. Airway epithelium A. Cell populations and structure (nose, large and small airways, centriacinar region, alveoli) 1. Cell types 2. Histologic organization B. 1. 2. 3. Structure-function relationships Ciliated cell structure/function Mucus cell structure/function Phenotypic transitions C. Imaging techniques 1. Applications of microscopy to investigating structure and function 2. Light microscopy a. Advantages of different optical configurations b. Documentation (microphotography and video microscopy) 3. Transmission electron microscopy a. Ultrathin sections b. Freeze-fracture 4. Scanning electron microscopy 5. Special techniques a. Immunocytochemistry b. In situ hybridization c. Elemental microprobe analysis II. Acute airway injury Sites of primary damage and repair A. Nasal mucosa - ozone, sulfur dioxide, nitrogen dioxide, viral infection B. Lower airway III. Chronic exposures A. Histologic changes Mucus cell hyperplasia Squamous metaplasia Neoplasia B. Ultrastructural changes IV. In vitro cell and organ culture models A. Epithelial cell culture B. Tissue and organ culture V. Lung mucociliary system A. Mucus secretion revisited B. Ciliary structure and activity revisited C. The complex interplay of secretory and ciliated components D. Pathologic consequences of dysfunction of components ENVR732-001 Fall 2009 25 Required reading: 1. Carson, J. L. 1993. Ozone Exposure, Respiratory Health Effects. In: Handbook of Hazardous Materials. Academic Press, Inc., pp. 527-538. 2. Carson, J. L., A. M. Collier, S. C. S. Hu, and R. B. Devlin. 1993. Effect of Nitrogen Dioxide on Human Nasal Epithelium. Am J Respir Cell Mol Biol. 9:264-270. Supplemental Reading: 1. Carson, J. L., A. M. Collier, and Clyde, Jr. 1979. Ciliary membrane alterations occurring in experimental Mycoplasma pneumoniae infection. Science 206: 349-351. 2. Carson, J. L., A. M. Collier, and S. S. Hu. 1985. Acquired ciliary defects in nasal epithelium of children with acute viral upper respiratory infections. N Engl J Med. 312:463-468. 3. Carson, J. L., A. M. Collier, S. Hu, C. A. Smith, and P. Stewart. 1987. The appearance of compound cilia in the nasal mucosa of normal human subjects following acute, in vivo exposure to sulfur dioxide. Environ Res. 42: 155-165. 4. Carson, J. L., Collier, A. M., Gambling, T. M., Hu, S. S. 1998. An autoradiographic assessment of epithelial cell proliferation and post-natal maturation of the tracheal epithelium in infant ferrets. Anat. Rec. 256:242-251. 5. Carson, J. L., A. M. Collier, G. W. Fernald, and S. C. Hu. 1994. Microtubular discontinuities as acquired ciliary defects in airway epithelium of patients with chronic respiratory diseases. Ultrastruct Pathol. 18: 327-332. 6. Becker, S., Soukup, J. M., Reed, W., Carson, J., Devlin, R. B., Noah, T. L. 1998. Effect of ozone on susceptibility to respiratory viral infection and virus-induced cytokine secretion. Environ. Toxicol. Pharmacol. 6:257-265. 7. Frampton, M. W., Ghio, A. J., Samet, J. M., Carson, J. L., Carter, J. D., Devlin, R. B. 1999. Effects of aqueous extracts of PM(10) filters from the Utah Valley on human airway epithelial cells. Am. J. Physiol. 277(5 Pt 1):L960-967. 8. Reed, W., Carson, J. L., Moats-Staats, B. M., Lucier, T., Hu, P.-C., Brighton, L., Gambling, T. M., Huang, C.-H., Leigh, M. W., Collier, A. M. 2000. Identification of an axonemal dynein heavy chain expressed early in airway epithelial ciliogenesis. Am. J. Resp. Cell. Molec. Biol. 23:734-741. 9. Calderon-Garciduenas, L., Valencia-Salazar, G., Rodriguez-Alcaraz, A., Gambling, T. M., Garcia, R., Osnaya, N., Villarreal-Calderon, A., Devlin, R. B., Carson, J. L. 2001. Ultrastructural nasal pathology in children chronically and sequentially exposed to air pollutants. Am. J. Respir. Cell & Molec. Biol. 24:132-138. 10. Calderon-Garciduenas L., Mora-Tiscareno A., Fordham L. A. Q. , Chung C. J., Carson, J. L., Koren H., Devlin, R. B. 2001. Canines as sentinel species for assessing chronic exposures to air pollutants. Part I. Respiratory Pathology. Toxicol. Sci. 61:342-355. 11. Ghio AJ, Silbajoris R, Carson JL, Samet JM. 2001. Biological effects of oil fly ash. Environ. Health Perspect. 110 Suppl 1:89-94. (Review). 12. Ghio, A. J., Gilbey, J. G., Roggli, V. L., Richards, J. H., McGee, J. K., Carson, J. L., Devlin, R. B., Cascio, W. E. 2001. Diffuse alveolar damage after exposure to an oil fly ash. Am. J. Respir. Crit. Care Med. 164:1514-1518. ENVR732-001 Fall 2009 26 Oct. 8 ---Diesel exhaust and organic compounds health effects. I. Jaspers Sources On road vs. off road Old engines vs. new engines Composition Particle phase Gas phase Health Effects Epidemiology Clinical Studies o o o o Inflammation Immunology and Allergy Cancer Cardiovascular Effects Animal Studies o Acute vs. Chronic o Immunology and Allergy o Cancer In vitro Studies o Epithelial Cells o Monocytes/Macrophages Considerations Diesel Sample o Fresh vs. aged o Particle vs. organic extract vs. complex mixture o High load vs. idle Required reading: 1) Sydbom A, Blomberg A, Parnia S, Stenfors N, Sandstrom T, Dahlen SE (2001) Health effects of diesel exhaust emissions. Eur Respir J 17: 733-746. 2) Riedl M, Diaz-Sanchez D (2005) Biology of diesel exhaust effects on respiratory function. J Allergy Clin Immunol 115: 221-228 Optional reading: 1) Sydbom A, Dahlen SE (2000) Experimental studies on the effects of diesel exhaust emissions. Scand J Work Environ Health 26 Suppl 1: 28-38 2) Pandya RJ, Solomon G, Kinner A, Balmes JR (2002) Diesel exhaust and asthma: hypotheses and molecular mechanisms of action. Environ Health Perspect 110 Suppl 1: 103-112 3) Mauderly JL (2001) Diesel emissions: is more health research still needed? Toxicol Sci 62: 6-9 4) Mauderly JL (2000) Animal models for the effect of age on susceptibility to inhaled particulate matter. Inhal Toxicol 12: 863-900 ENVR732-001 Oct. 13 Fall 2009 27 ---Health Effects of Airborne Particulate Matter: Epidemiology Studies. L. Neas 28 I. Mortality and Hospitalization at Typical Particle Levels 29 ENVR732-001 Fall 2009 $ Poisson regression and daily health event time series Philadelphia, Pennsylvania 100 U.S. Cities II. Effects of Long-term Particle Exposures Cox proportional hazard models and cumulative mortality in a closed cohort Harvard Six-Cities Adult Longitudinal Cohort $ American Cancer Society Cohort III. Physiological Mechanisms ENVR732-001 $ $ Fall 2009 30 Mixed effect models and daily variation in physiological measurements Autonomic control of the heart and heart rate variability IV. Particle Sources $ Source apportionment models and daily mortality $ Fine versus coarse particles $ Fine particles from different sources V. Uncertainities Composition, size of particles, species Dosimetry Site of action Cause and effect relationship Pathophysiology and mechanisms Required Reading: 1. Association of fine particulate matter from different sources with daily mortality in six U.S. cities. Laden F, Neas LM, Dockery DW, Schwartz J. Environ Health Perspect 2000 Oct;108(10) Optional Reading: 1. The National Morbidity, Mortality, and Air Pollution Study. Part II: Morbidity and Mortality from Air Pollution in the United States. Samet JM, Zeger SL, Dominici F, Curriero F, Coursac I, Dockery DW, Schwartz J, Zanobetti A. http://www.healtheffects.org/Pubs/Samet2.pdf 1. An association between air pollution and mortality in six U.S. cities. Dockery DW, Pope CA 3d, Xu X, Spengler JD, Ware JH, Fay ME, Ferris BG Jr, Speizer FE. N Engl J Med 1993 Dec 9;329(24):1753-9 2. Daily variation of particulate air pollution and poor cardiac autonomic control in the elderly. Liao D, Creason J, Shy C, Williams R, Watts R, Zweidinger. Environ Health Perspect 1999 Jul;107(7):521-5 3. Is daily mortality associated specifically with fine particles? Schwartz J, Dockery DW, Neas LM J Air Waste Manag Assoc 1996 Oct;46(10):927-39 4.“The Fog” in Eleven Blue Men by Berton Roueche. ENVR732-001 Oct. 15 Fall 2009 31 ---Adverse health effects of indoor air (biological aerosols, home environment). J.Rosati Outdoor Sources of Indoor Air Pollution How indoor contamination by outdoor sources occurs Types of outdoor sources and contaminants o Vehicles o Industry o Photochemical oxidants (Ozone) o Bioaerosols o Pesticides o Radiologics Health effects Mitigation Indoor Sources of Indoor Air Pollution Types of indoor sources and contaminants o Human Activities Human movement Cooking Combustion Showering/washing o Building Related Contamination Asbestos Lead VOCs o Appliances o Animals o Cockroaches o Dust mites o Biologics Mold, fungi, bacteria, viruses o Endotoxin Health Effects Mitigation Required reading: Wallace, L. Indoor particles: a review. J. Air & Waste Manage. Assoc., 46, 98-126. Mendell, M. Indoor residential chemical emissions as risk factors for respiratory and allergic effects in children: a review. Indoor Air, 17, 259-277. Optional reading: Ferro et al. Source strengths for indoor human activities that resuspend particulate matter. Environ. Sci. Tech., 38, 1759-1764. Jacob, B. Indoor exposure to molds and allergic sensitization. Environ. Health Persp., 110, 647-653. ENVR732-001 Oct. 20 Fall 2009 32 ---Acute effects of ozone; laboratory studies. Biochemical and immunotoxic effects. N. Alexis ENVR732-001 Fall 2009 33 I. In vivo/in vitro Exposure Systems A. Types (typical protocols with human volunteers) B. Advantages and disadvantages II. Deposition and Absorption in the Lung III. Ozone Reaction with Lung Constituents Lipids, proteins, antioxidants (vit C, E, glutathione, Uric acid) IV. Morphological Effecs A. Phagocyte changes B. Epithelial cell changes V. Cellular and Biochemical Effects A. Cellular Neutrophilic inflammation Macrophage activation B. Biochemical Lipid metabolism (AA formation) Cytokine and protein production Neuropeptide generation (Sub P) ROS generation Signal transduction events (NF-Kappa B) VI. Immunologic Effects A. Lung clearance B. Macrophage phagocytosis, oxidative burst, bacterial response to LPS C. Surface marker responses VII. Interesting Similarities to LPS A. Changes in lung function B. Neutrophilic inflammation C. Biochemical response IL-8, IL-6, protein D. Role of mCD14 and CD11b Required Reading: 1. Koren, H.S., R.B. Devlin, S. Becker. Ozone-induced inflammatory response in pulmonary cells. In: Xenobiotics and Inflammation. Eds. L.B. Schook and D.L. Laskin. Academic Press, NY, pp. 249-281. 1994. 2. Krishna, M.T. et al. Effects of ozone on epithelium and sensory nerves in the bronchial mucosa of healthy humans. Am. J. Respir. Crit. Care Med. 156:943-950, 1997. Optional Reading: 1. Pryor, W.A. Mechanisms of radical formation from reactions of ozone with target molecules in the lung. Free Radical Biology & Medicine 17:451-465. 1994. 2. Victorin, K. Review of the genotoxicity of ozone. Mutat. Res. 277:221-38. 1992. 3. United States Environmental Protection Agency. Air Quality Criteria for ozone and related photochemical oxidants. EPA/600/AP-93/004c. 1993. 4. Lippman, M. Health effects of tropospheric ozone: review of recent research findings and their implications to ambient air quality standards. J. Expo. Anal. Environ. Epidem. 3:103-129. 1993. Oct. 16 FALL RECESS ENVR732-001 Oct. 27 Fall 2009 34 ---Acute effects of ozone; laboratory studies. Systemic and lung function effects. M.J.Hazucha I. Sources, emissions, measurements, NAAQS (briefly) II. Single exposure to ozone (short and prolonged) A. Systemic effects (CNS, olfactory, behavioral, cardiovascular) B. Pulmonary symptoms and function effects 1. Healthy subjects (age, race, gender) a. Dosimetry (threshold, C x T x VE) b. Symptomatic response c. Lung function changes d. Variability of response (responders, nonresponders) e. Mechanisms of response 2. Populations at-risk (children, asthma, allergies, COPD) 3. Concentration-response relationship III. Repeated exposures A. Consecutive daily (adaptation) B. Repeated periodically (consistency of response) Required reading: 1. Lippmann, M. Health effects of ozone. A critical review. JAPCA. 39: 672-695, 1989. Optional reading: 1. Air Quality Criteria for Ozone and Related Photochemical Oxidants. US EPA, EPA/600/AP-93/004c, Review draft Vol.III, Sec. 7-2, p. 7-1 to 7-118. 2. Hazucha, M. J., D. V. Bates, and P. A. Bromberg. Mechanism of action of ozone on the human lung. J Appl Physiol. :Respirat Environ Exercise Physiol. 67: 1535-1541, 1989. 3. Mehlman, M. A. and C. Borek. Toxicity and Biochemical Mechanisms of Ozone. Environ Res. 42: 36-53, 1987. 4. Lippmann, M. Effects of ozone on respiratory function and structure. Annu Rev Public Health. 10: 49-67, 1989. ENVR732-001 Fall 2009 35 Oct. 29 --- Sulfur dioxide and its products: Effects on sensitive individuals P.A.Bromberg SO2 is a “Criteria” air pollutant gas. There are two primary NAAQS; 0.14 ppm averaged over 24 hrs. 0.03 ppm averaged over one year I. Sources: SO2 is directly emitted into the air by the combustion of sulfur-containing fuels, notably in electric power plants. It is also an important chemical in operations of the chemical, paper and cement manufacturing and smelting industries, in fumigation, in preservation of perishables (it is a reducing agent and anti-oxidant), in refrigeration, etc. It is therefore an important chemical for occupational health. The American Council of Governmental Industrial Hygienists (ACGME) has established a Threshold Limit Value (TLV) for exposure of 2 ppm weighted over an 8-hr work day with a 15 min ceiling of 5 ppm. The Occupational Safety and Health Administration (OSHA) also established an eight hour weighted average exposure limit of 2ppm although the NIOSH recommendation is for a level of 0.5ppm. According to NIOSH exposure to more than 100ppm for more than 30 min is “immediately dangerous to life or health”. II. Chemistry: SO2 is a moderately water-soluble gas. It rapidly reacts with water to form sulfurous acid (H2SO3) which immediately dissociates to H+ and HSO3- (pKa = 1.9). The pKa of the further dissociation of the HSO3- ion is 7.2. Thus, most of the SO2 absorbed on respiratory surfaces following its inhalation will be in the HSO3- form. This is a reactive nucleophile which can be oxidized to sulfate (SO4--) to be ultimately excreted in the urine or incorporated into glycoproteins like mucins, or can attack RS-SR’ residues in proteins to form RS-SO3- and R’SH. The bisulfite ion is also absorbed into the blood stream and is widely distributed. The amount of H+ generated rapidly in a localized region (airways mucosa) during intense SO2 exposures may also play a role in its toxicity. III. Physiology and toxicity of inhaled SO2: As a water-soluble gas, SO2 is rapidly absorbed by mucosal surfaces. The small initial tissue volume of distribution allows relatively high mucosal concentrations of HSO3- to be attained. Only a small fraction of inhaled SO2 reaches the lower airways but this fraction can be significantly increased by increasing inspiratory flow rate (e.g., during exercise). The dose to the lower airways also depends on the concentration of SO 2 in the inspired air, the duration of exposure and the volume of minute ventilation. The latter is also increased during exercise. Clearly, any effects of a given concentration of SO2 on the lower airways will be greatly enhanced by exercise or by voluntary hyperventilation. The fact that the nose is increasingly bypassed in favor of the oral route as ventilation increases also increases the fraction of the inhaled SO2 that reaches the lower airway. At high concentrations SO2 causes acute bronchitis with remodeling of the airways epithelium into a goblet cellrich, mucus-secreting state. Sub-lethal inhalational injury has been found to cause permanent airways damage in severely exposed individuals. At low concentrations (< 1ppm), SO2 inhalation appears to be innocuous for healthy adults. However, in some adult asthmatics, concentrations as low as 0.25 ppm have been shown to cause symptomatic bronchospasm when inhaled at a minute ventilation of at least 30-40 liters. The degree of SO2 hyper-responsiveness among asthmatics varies widely, but as a group they are much more sensitive to SO2-induced bronchoconstriction than are healthy individuals. Several other features of this response are noteworthy: 1. the bronchoconstriction develops after only a very few minutes of exposure, but attains a maximum after 5-10 min which is not exceeded (and may even decline) despite continued exposure; 2. the bronchoconstriction responds promptly to inhalation of conventional beta-adrenergic agents; 3. there is no “delayed phase” of bronchospasm ENVR732-001 Fall 2009 36 several hours after the exposure (as is often the case following specific antigen inhalation challenge or following inhalation of di-isocyanates in sensitized individuals); 4. there are many similarities between the phenomenon of “exercise-induced bronchospasm” and SO2 (plus hyperventilation)-induced bronchospasm. These observations (made during the 1980’s) led EPA to consider establishing a short term NAAQS for SO2, but this was not done for reasons to be discussed. IV. Transformations of SO2 in the atmosphere: SO2 undergoes fairly rapid oxidation to SO3 which is enhanced by the oxidant-rich conditions characteristic of photochemically driven transformations of primary emissions of NOx and hydrocarbons to produce oxidants like ozone and hydroxyl radical. (This connection presumably accounts for the fairly close association of atmospheric ozone concentrations with finely particulate sulfate levels). The oxidation of SO2 can occur in the gas phase, but under high humidity conditions can also occur in water droplets. In the presence of water, SO3 is converted to H2SO4 which can attack metal oxides (e.g., ZnO) to convert them to water-soluble (bioavailable) sulfates. Jang and Kamens at UNC have shown that H2SO4 is an important catalyst for the formation of complex, polar oxy-organics from volatile, non-polar hydrocarbons. The former are responsible for de novo particle formation as well as condensing on the surface of other available particles (e.g., elemental carbon particles). Their toxicologic properties are under investigation. Molina’s group at MIT suggests that H2SO4 may form stable, doubly hydrogen-bonded adducts with organic acids in the atmosphere and that organic acids catalyze atmospheric H2SO4 formation. Thus, SO2 products may be playing a much more important role in generating toxic species than has been suspected in the past. Of course, the role of SO 2 emissions and their long-range atmospheric transport in the generation of acid rain (and of its ecologic effects) is well recognized. Finally it should be noted that emissions of NH3 gas (e.g., from fertilizer use) can effectively neutralize the acidity of H2SO4 in the atmosphere so that measurements of atmospheric acidity at a given time may grossly underestimate the importance of prior H2SO4 generation. The inhalation of aerosols of H2SO4 at a concentration of at least 100 μg/m3 can provoke bronchoconstriction in some asthmatics (again, not in normals), but this phenomenon appears to depend on the acidity since NH4HSO4 is much less effective and (NH4)2SO4 is ineffective. Thus, unlike the HSO3- ion, the HSO4- ion appears to be much less reactive from a toxicologic standpoint. Required reading: 1. D. H. Horstman, L. J. Roger, H. Kehrl & M. Hazucha. Airway sensitivity of asthmatics to sulfur dioxide. Toxicol. Ind. Health 2: 289-298, 1986. 2. R. A. Bethel et. al. Effect of exercise rate and route of inhalation on sulfur dioxide-induced bronchoconstriction in asthmatic subjects. Am. Rev. Respir. Dis. 128: 592-596, 1983. ENVR732-001 Fall 2009 37 Nov. 3 ---Health effects of nitrogen oxides. M.J.Hazucha I. Sources and Emissions II. Measurement Techniques III. Standards (NAAQS, WHO, ACGIH, NIOSH) IV. NOx and NOy V. Morbidity and Mortality from Accidental Exposures (NO2 and N2O4) A. Silo Filler’s Disease B. Industrial Exposures and Oxidizer Spills C. Sample Case Reports VI. Animal Toxicology A. Morphological effects of NO2 B. Physiological responses C. Effects of NO2 on viral and bacterial infectivity VII. Human Exposure Studies A. Cardiovascular Responses B. Pulmonary function and symptom responses 1. Healthy Subjects a. Symptoms b. Lung Function responses c. Airway responsiveness d. Mechanisms of response e. Infectivity studies 2. “At-risk” populations (asthmatics, children, elderly) a. Lung function responses b. Airway reactivity VIII. Epidemiology A. Outdoor studies B. Indoor Studies a. Lung Function b. Respiratory Infectivity IX. Nitrates, Nitric and Nitrous Acid, Nitric Oxide, Nitrous Oxide Required reading: 1. Hazucha, M.J. Controlled exposures to ozone, nitrogen oxides and acids. In: Air Pollution and Health, Eds. Holgate,S.T., Koren,H.S., Samet, J.M., and Maynard,R.L., Academic Press, London, UK, 1998. 2. Nitrogen Oxides. In: Air Quality Guidelines for Europe, WHO, (draft, 1995) Optional Reading: 1. Air Quality Criteria for Oxides of Nitrogen. vol III (Chapters 13-16, covering animal toxicology, epidemiology, controlled human exposures, risk assessment). US EPA Document #EPA600/8-91/049cF 2. Patty’s Industrial Hygiene and Toxicology (v. 2. Pt. F) pp 4566-4591 (In reference) TAKE HOME EXAM ENVR732-001 Nov. 5 Fall 2009 38 --- Kinetics, mechanisms of action and health effects of exposure to CO. M.J.Hazucha I. Sources, emissions, transport, measurements, trends, NAAQS A. Population exposures (outdoor, indoor) B. Personal and biological monitoring II. Pharmacokinetics of CO A. Kinetics of COHb formation in lung 1. Endogenous production 2. Absorption, distribution, elimination B. Determinants of toxicity C. Intracellular effects (myoglobin, cytochromes) III. Modeling of COHb formation (Coburn-Foster-Kane and other) IV. Physiologic effects A. Cardiovascular system (response to exercise, cardiovasc. and blood disease) B. Neurobehavioral effects (CBF, sensory effects, vigilance, cognition) C. Perinatal effects, developmental toxicity (fetotoxicity, SIDS, body mass) D. Adaptation, habituation E. Other systemic effects V. CO interaction with other pollutants and factors A. CO and drugs B. CO and Environmental Tobacco Smoke C. CO and altitude Required reading: 1. Turino, G. M. Effect of carbon monoxide on the cardiorespiratory system. Circulation. 63: 253A259A, 1981. 2. Air Quality Criteria for Carbon Monoxide. Chapter 5: Kinetics and mechanisms of action. EPA/1999. Optional reading: 1. Coburn, R. F., R. E. Forster, and P. B. Kane. Considerations of the physiological variables that determine the blood carboxyhemoglobin concentration in man. J. Clin. Invest. 44:1899-1910, 1965. 2. Mcgrath, J. J., R. M. Schreck, and P. S. Lee. Carboxyhemoglobin Levels in Humans - Effects of Altitude. Inhal Toxicol. 5: 241-249, 1993. 3. Fechter, L. D. Neurotoxicity of prenatal carbon monoxide exposure. Res Rep Health Eff Inst. 3-22, 1987. 4. Mennear, J. H. Carbon Monoxide and Cardiovascular Disease - An Analysis of the Weight of Evidence. Regul Toxicol Pharmacol. 17: 77-84, 1993. ENVR732-001 Fall 2009 39 Nov. 10 --- Health impacts of secondhand smoke. D. Diaz-Sanchez To be provided ENVR732-001 Fall 2009 40 Nov. 12 --- Systemic poisons; Lead and other metals. D. Otto I. Sources, emissions, measurements, NAAQS (briefly) II. Pharmacokinetics of Pb Routes of exposure Absorption Retention Excretion III. General mechanisms of action IV. Physiologic response to Pb Hemopoietic system Nervous system (central, peripheral) Renal system Endocrine system Cardiovascular system Immune system Required reading: 1. Pueschel, S.M., Linakis, J. G., Anderson, A.C. Pathophysiology of lead poisoning. In: Lead poisoning in childhood, Eds. Pueschel, S.M., Linakis, J. G., Anderson, A.C., Paul H. Brooks Publ. Co., London, pp. 75-96, 1996. 2. Royce,S.E. Lead toxicity. Ed. Needlene, H.L. US DHHS, pp. 1-25, 1992. Optional reading: 1. Measuring lead exposure in infants, children, and other sensitive populations. National Research Council, National Academy Press, Washington, DC 1993. 2. Pounds, J.G., Cory-Slechta, D.A., Cranmer, J.M., (eds.) New dimensions of lead neurotoxicity: Redefining mechanisms and effects. Neurotoxicology vol.14, #2 and 3, 1993. ENVR732-001 Fall 2009 41 Nov. 17 ---Health effects of pollutant mixtures. P.A. Bromberg Do controlled pollutant exposure studies of humans or animals produce health effects that are concordant with the observational studies of populations spontaneously exposed to varying levels of ambient air pollution? [The observational studies take advantage of exposure gradients either in time (in a given location) or in space (multiple separate locations concurrently, each location having a different general pattern of pollution composition or intensity)]. If not, why not? 1. Are the health effects observed in human populations “driven” by a group of “susceptible” individuals who were not represented in the controlled studies? [“Susceptibility” might be conferred by the presence of preexisting disease, by some other environmental exposure, or by genetic polymorphisms]. If “susceptibility” is the answer, would non-susceptible individuals challenged with a controlled exposure to the agent in question exhibit some detectable changes, or would they show no detectable effects at all? Animal toxicology studies are always difficult to apply directly to human health risk evaluation not only because of questions about the extrapolation of tissue dosimetry from animal to man, but because of different susceptibility. 2. Are the controlled exposures really representative of ambient air pollution? Ambient air pollution almost invariably represents a very complex mixture of gases and particulate matter. Many of the components are newly synthesized in the atmosphere from primary emissions by complex chemical, photochemical and physical processes. Can controlled exposures ever adequately mimic naturallyoccurring exposure? 3. Are the apparently significant associations between morbidity and acute/subacute mortality and ambient air pollution levels real or are they artefactual? I. A. 1. 2. 3. 4. 5. 6. Ozone: Symptoms, effects on lung function and airways inflammation in healthy individuals. 90% of inhaled ozone is absorbed by chemical reaction along airway surfaces. Ozone has been shown to react with unsaturated foleic acid residues present in a fraction of glycerophosphocholine lipids associated with pulmonary surfactant. The resulting 1-palmitoyl-2-(9′-oxo-nonanoyl)glycerophosphocholine is a potent, biologically active product which can cause epithelial cells to release PGE2, release IL-8, activate PLA2, and induce apoptosis (W. Pryor, M. Friedman et al; C. White, R. Murphy et al). . C•t•V dosimetric model Sensitization of mucosal nociceptive nerves (C-fibers); (? by PGE2); involuntary inhibition of inspiration (decreased FVC and FEV1)(effects of age) Damage/death of ciliated epithelial cells (? apoptosis) Acute mucosal inflammation (neutrophilic) Bronchial hyperreactivity to inhaled methacholine or histamine B. Respiratory morbidity in populations exposed to low levels of ambient ozone (D.V. Bates; R. Burnett et al). [Note the potential confounding association of ozone pollution with fine particulate sulfate]. C. Controlled exposures of normals to ozone with HNO3 vapor or H2SO4 aerosol fail to reveal major differences in lung function or inflammatory airways response as compared to exposure to ozone alone (R. Aris et al). ENVR732-001 Fall 2009 42 D. Lung function decrements provoked by L.A. smog are mimicked accurately by controlled exposure to pure ozone at the same concentration as was present in the smog (0.16 ppm). [Suggests that the only important toxic substance in the smog was ozone gas]. E. Short controlled exposure of asthmatics to ozone alone does not reveal major response differences as compared to responses of normal volunteers. F. Newer exposure studies in asthmatics. i. prolonged exposure (0.16 ppm for 7-8 hours) (Horstman et al). ii. ozone followed by inhaled specific antigen challenge (Molfino et al; Jorres et al; Peden et al). II. A. PM: London disaster, December 1952. SO2 and PM (as high as 4000 μg/m3). B. Population studies: 1. Time-series statistical models applied to daily non-traumatic mortality in urban areas (death certificates) vs. daily average PM concentration (less than 150 μg/m3). Increased pulmonary and cardiovascular mortality diagnoses in older adults. (J. Schwartz et al). 2. Time-series analysis applied to daily respiratory morbidity. (D. Dockery, J. Schwartz). 3. “Six Cities” study (Dockery et al) 4. American Cancer Society data base analysis (Pope et al) 5. Utah Valley study (Pope et al) 6. Atlanta during 1996 summer Olympic games (restricted vehicular traffic). 7. Dublin, Ireland experience with change in fuel burning. C. Major components of ambient air "respirable" PM include: elemental carbon; organic carbon; inorganic sulfates and nitrates; metal salts (Fe; Zn; smaller amounts of Cu, Ni, V, Pb, As). But, controlled exposure to "relevant" doses of: elemental carbon; inorganic sulfates and nitrates; soluble metal compounds, provokes little toxicity! Why? The answer to this question is important for several reasons: 1. The plausibility of the conclusions drawn from the observational population studies would be enhanced. 2. Understanding the nature of the toxic species responsible for PM pollution-associated health effects would focus efforts related to air quality monitoring, regulation and mitigation, and give greater confidence that the costs involved would be rewarded by improved public health. 3. Understanding the underlying toxicologic mechanisms would facilitate finding “markers” of effect and point toward factors (including genetic) that could increase individual susceptibility to adverse health effects. In addition, chemoprophylactic approaches could be suggested for protection against adverse health effects in susceptible individuals. D. Newer controlled exposure studies: 1. Concentrated ambient air particles (CAPS) 2. Ultrafine particles dosed by number (not mass) concentration 3. "One atmosphere" smog chamber (Jeffries, Sexton, Kamens, Jang, Jaspers). [?role for organic carbon compounds]. ENVR732-001 Fall 2009 43 Nov. 19 --- Cardiovascular effects of air pollutants. W. Cascio To be provided ENVR732-001 Nov. 24 Fall 2009 Asthma and allergic disease. D. Peden Not provided. Nov. 26 THANKSGIVING RECESS 44 ENVR732-001 Dec. 1 Fall 2009 45 ---Approaches and challenges in health risk assessment. C. Shoaf I. Principles of Risk Assessment and Risk Management A. What is Risk? B. What is Environmental Risk? II.Elements of health risk assessment and Risk Management A. Research a. Utility of acute laboratory and clinical studies b. The role of epidemiology B. Risk assessment a. Hazard identification b. Dose-response evaluation c. Dose-response curve d. Exposure assessment (direct and alternative methods) Reference Concentration: RfC Inhalation Reference Concentration Benchmark Dose Human Exposure Evaluation Exposure Assessment Analysis Format Concentration-Duration-Severity Modeling Schematic Exposure Duration Exposure Assessment Residential Exposure: Inhalation of Airborne (vapor phase) Chemicals C. Risk management III. NAS Risk Assessment Paradigm A. Risk Characterization B. Presentation of Risk C. Widespread Use D. Risks of Living E. Annual Risks of Dying F. Lower Level Risks (Annual) G. The Johnston Amendment Required Reading: Haber, L.T., Dollarhide, J.S., Maier A., Dourson, M.L. (2001) Ch. 5, Noncancer Risk Assessment: Principles and Practice in Environmental and Occupational Settings. In: Bingham, E., Cohrssen, B., and Powell, C.H., eds. Patty's Toxicology, Fifth Edition, Volume 1 John Wiley & Sons, Inc., New York.; pp. 169-232. ENVR732-001 Dec. 3 Fall 2009 46 ---Protection of susceptible population. P.A. Bromberg For detailed description see Bromberg_Suscept.pdf at HSL reserves site ENVR732-001 Dec. 8 Fall 2009 47 Developmental and reproductive toxicology. J.Rogers I. The Link Cancer Genetic Toxicology Developmental Toxicology Reproductive Toxicology II. Air Pollution and Toxicology Cancer Genetic Toxicology Developmental Toxicology Reproductive Toxicology III. Chemical Carcinogenesis Neoplasia Malignant Cancer Tumors Benign Neoplasms Malignant Neoplasms IV. Genetic Toxicology A. History B. Sources of Genotoxic Air Pollution Some of the Genotoxic Air Pollutants Source vs. Exposure Examples of Research Studies Pulling it all together C. Type of effects Heritable effects Somatic cell effects D. Consequences of Mutation Heritable effects Somatic cell effects E. Kinds of Genetic Damage F. Means of Influencing Genetic Mechanisms Alter the Genetic Material Alter Control of Genetic Material V. Developmental Toxicology History Wilson’s General Principles of Teratology VI. Reproductive Toxicology VII. Types of Compounds Found in Source and Ambient Air ENVR732-001 Fall 2009 A. B. C. D. 48 Chemical Species Detected in Ambient Air Sources Having High Numbers of Compounds with Positive Assays Compounds from Tobacco Smoke Giving a Positive Assay Relative Potency of Organic Matter from Various Combustion Sources VIII. Atmospheric Transformation A. UNC Outdoor Chamber Study B. Fractionating Organic Environmental Emissions C. Fractionating Cigarette Smoke Condensate and Bioassay D. Comparing Relative Mutagenicity for Environmental Emissions IX. Human Studies A. Nasal Mucosa, Single Strand Breaks and Urban Pollution (3rd Study) B. DNA Migration Length for SW Mexico City Groups Required reading: 1. Calderon-Garciduenas, L., N. Osnaya-Brizuela, L. Ramirez-Martinez, and A. Villarreal-Calderon. DNA Strand Breaks in Human Nasal Respiratory Epithelium Are Induced upon Exposure to Urban Pollution. Environ. Health Perspect. 104:160-168, 1996. 2. Kamens, R.M., G.D. Rives, J.M. Perry, D.A. Bell, R.F. Paylor Jr., R.G. Goodman, and L.D. Claxton. Mutagenic Changes in Dilute Wood Smoke as It Ages and Reacts with Ozone and Nitrogen Dioxide: An Outdoor Chamber Study. Environ. Sci. Technol. 18:523-529, 1984. 3. Graedel, T.E., D.T. Hawkins, L.D. Claxton. In: Atmospheric Chemical Compounds. Chapter 1, pp. 1-40, 1986. FINAL TAKE HOME EXAM