Vomiting, Diarrhea & Constipation Mark J. Koruda, MD Professor of Surgery
advertisement

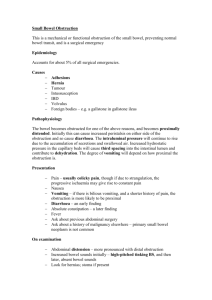
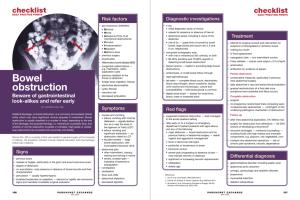
Vomiting, Diarrhea & Constipation Mark J. Koruda, MD Professor of Surgery Case 1 • A 54-year-old woman presents with a two day history of crampy abdominal pain followed by episodes of bilious emesis. • Important Items in the History? • Previously hysterectomy for treatment of cervical cancer. Small Bowel Obstruction Small Bowel Obstruction Signs & Symptoms • • • • • • • Intermittent, Crampy Abdominal Pain Nausea / Emesis Distension Obstipation Peristaltic Rushes on Auscultation Focal Tenderness Diffuse Peritonitis Case 1 • What findings should be looked for on physical exam? • Distended • No peritoneal signs Case 1 • What laboratory tests should be ordered? Small Bowel Obstruction Laboratory Evaluation • May see hypochloremic, hypokalemic metabolic alkalosis if having frequent emesis (proximal obstruction). • May see evidence of contraction alkalosis – Increased H/H, BUN. • WBC usually normal early. Case 1 • What laboratory tests should be ordered? • What diagnostic tests should be ordered? Small Bowel Obstruction Radiologic Evaluation • Xrays: ? AFLs, ? Free Air, ? Distal Gas • UGI / SBFT: Identify mechanical obstruction • Enteroclysis: Independent of gastric emptying • CT Scan: ? Free Air, ? Pneumatosis, ? Small Bowel Obstruction Etiologies • Adhesions • Malignancy • External or Internal Hernia • Volvulus • Crohn’s Disease • Intra-abdominal Abscess Small Bowel Obstruction Etiologies (Cont.) • • • • • • • Radiation Stricture Foreign Body Gallstone Ileus Meckel’s Diverticulum Intramural Hematoma Mesenteric Ischemia Intussusception Intestinal Ileus Etiologies • • • • • • • • • Postoperative State Sepsis Electrolyte Imbalance Drugs Ureteral and Biliary Colic Retroperitoneal Hemorrhage Spinal Cord Injury Myocardial Infarction Pneumonia Case 1 • What is the initial management plan? Small Bowel Obstruction Partial vs. Total • Why Not Just Wait?? – Potential for Closed Loop Obstruction – Risk of Ischemia / Perforation (4-6 hrs) Small Bowel Obstruction Treatment • • • • Correct intravascular volume deficit NGT vs. Miller-Abbott or Cantor Tubes Serial Exams Operation if no improvement or if signs of complete (closed loop) obstruction or incarceration. • Evaluation of Bowel Viability Small Bowel Obstruction Special Cases • Early Postoperative SBO – <1% risk in first month – Must be considered after 7 days of “ileus” since adhesions become dense in 2-3 weeks. • Recurrent SBO (5-15%) • Malignant Obstruction • Radiation Fibrosis Case 2 • A 72-year-old man presents with a two month history of gradually increasing constipation. • Key Points in History? Large Bowel Obstruction Diagnosis • Crampy Pain • Onset may be acute or insidious • Distension (50-60% have competent ileo-cecal valve and develop severe distension) • Xrays: 12-14 cm cecum, perforation risk • Contrast enema: Obstruction vs Oglive’s • Consider rigid sigmoidoscopy to r/o and treat sigmoid volvulus Case 2 • Physical Exam • What further tests are indicated Case 2 • Differential Diagnosis – Colonic Obstruction • Malignant • Benign – Colonic Dysfunction Large Bowel Obstruction Large Bowel Obstruction Etiologies • • • • • • • Colon Cancer Diverticulitis Extrinsic Cancer Fecal Impaction Intussusception Volvulus Incarcerated Hernias Large Bowel Obstruction Colon Cancer • 20% of colon cancers present with obstruction • Left-sided lesions are more prone to obstruct (more narrow lumen, more solid fecal stream) Large Bowel Obstruction Treatment • IVF • NGT • Operation – Emergently if signs of peritonitis / perforation – Prep bowel if possible • Is an ostomy necessary? – Right vs. Left-sided Lesions – Traditional vs. Newer Attitudes Large Bowel Dysfunction • Inflammation • Colonic Inertia • Etc Oglive’s Syndrome (Colonic Pseudo-Obstruction) • May mimic mechanical obstruction • Associated Conditions • Treatment: – Rectal tube / enemas /exams (work in most) – Colonoscopic decompression (80-90% eff.) – Surgery (Cecostomy vs. Resection) cecum >12 cm or peritoneal signs Case 3 • A 54-yo Caucasian male with history of ileocolonic Crohn's disease, s/p ileocolectomy in 1979, who has not been on any Rx for CD. Presents to the UNC ER complaining of crampy abdominal pain that began at 8 hrs earlier located in the right lower and left lower quadrant. He also had nausea and vomiting as well as decreasing flatus associated. The patient stated his last BM was on the day of admission. He stated that the pain feels like his previous obstructions. Occurring every couple of months, recently increasing in frequency. No fevers. About 10 lb weight loss. • Key Points in History What Is Crohn’s Disease? Esophagus Small Intestine Stomach Large Intestine (Colon) Rectum Appendix • Crohn’s disease (CD) is an inflammatory bowel disorder that may affect any part of the gastro-intestinal (GI) tract • The inflammation penetrates the lining of the GI tract and often causes ulcers to form Case 3 • Key Points in History Case 3 • Key Points in History – Crohn’s disease – Previous surgical history – No Crohn’s Rx – Chronic symptoms – Weight loss – No fevers – Crampy pain Case 3 • Physical Exam • Diagnostic Studies? • Differential Dx Crohn’s Disease Crohn’s Disease Crohn’s Disease • Medical vs Surgical Management Case 4 • 22yo UNC student presents with 3 mos of increasing “bloody diarrhea”, going to the bathroom 15-20x/day. “It rules my life!” • Key Points in History Case 4 • 22yo UNC student presents with 3 mos of increasing “bloody diarrhea”, going to the bathroom 15-20x/day. “It rules my life!” • Key Points in History – Diarrhea – Bleeding Case 4 • Physical Exam • Diagnostic Studies? Ulcerative Colitis