Third Trimester Bleeding, Postpartum Hemorrhage, & Shock Management UNC School of Medicine
advertisement

Third Trimester Bleeding, Postpartum
Hemorrhage, & Shock Management
UNC School of Medicine
Obstetrics and Gynecology Clerkship
Case Based Seminar Series
Objectives for Third Trimester Bleeding
List the causes of third trimester bleeding
Describe the initial evaluation of a patient with third
trimester bleeding
Differentiate the signs and symptoms of third trimester
bleeding
Describe the maternal and fetal complications of placenta
previa and abruption placenta
Describe the initial evaluation and management plan for
acute blood loss
List the indications and potential complications of blood
product transfusion
Objectives for Postpartum Hemorrhage
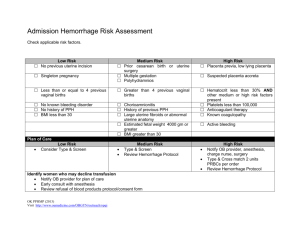
Identify the risk factors for postpartum hemorrhage
Construct a differential diagnosis for immediate and
delayed postpartum hemorrhage
Develop an evaluation and management plan for the
patient with postpartum hemorrhage
Rationale (why we care….)
4-5% of pregnancies complicated by 3rd trimester
bleeding
Immediate evaluation needed
Significant threat to mother & fetus (consider
physiologic increase in uterine blood flow)
Consider causes of maternal & fetal death
Priorities in management (triage!)
Vaginal Bleeding: Differential Diagnosis
Common:
Abruption, previa, preterm labor, labor
Less common:
Uterine rupture, fetal vessel rupture, lacerations/lesions,
cervical ectropion, polyps, vasa previa, bleeding disorders
Unknown
NOT vaginal bleeding!!!
(happens more than you think!)
Initial Management for Third Trimester
Bleeding
Stabilize patient – two large bore IVs if bleeding is heavy, EBL is
significant or patient is clearly unstable
Auscultate fetal heart rate - Confirm reassuring pattern
Focused history
PE
Vitals
Brief inspection for petechiae, bruising
Careful inspection of vulva
Speculum exam of vagina and cervix – NO DIGITAL EXAM until r/o
previa
Labs – CBC, coag profile, type and cross match
Ultrasound exam to assess placental location and fetal condition
Placental Abruption: Definition
Separation of placenta from uterine wall
Incidence
0.5-1.5% of all pregnancies
Recurrence risk
10% after 1st episode
25% after 2nd episode
Placental abruption: Risk factors and
associations
Cocaine
Prolonged PROM
Maternal hypertension
Uterine decompression
Abdominal trauma
Short umbilical cord
Smoking
Chorioamnionitis
Prior abruption
Multiparity
Preeclampsia
Multiple gestation
Placental Abruption: Symptoms
Vaginal bleeding
Abdominal or back pain
Uterine contractions
Uterine tenderness
Placental Abruption: Physical Findings
Vaginal bleeding
Uterine contractions
Hypertonus
Tetanic contractions
Non-reassuring fetal status or demise
Can be concealed hemorrhage
Placental Abruption: Laboratory Findings
Anemia
May be out of proportion to observed blood loss
DIC
Can occur in up to 10% (30% if “severe”)
First, increase in fibrin split products
Followed by decrease in fibrinogen
Placental Abruption: Diagnosis
Clinical scenario
Physical exam
NOT DIGITAL PELVIC EXAMS UNTIL RULE OUT PREVIA
Careful speculum exam
Ultrasound
Can evaluate previa
Not accurate to diagnose abruption
Placental Abruption: Management
Physical exam
Continuous electronic fetal monitoring
Ultrasound
Assess viability, gestational age, previa, fetal position/lie
Expectant mgmt
vaginal vs cesarean delivery
Available anesthesia, OR team for stat cesarean
delivery
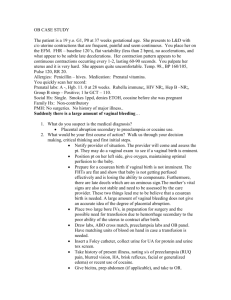
Placenta Previa: Definition
Placental tissue covers cervical os
Types:
Complete - covers os
Partial
Marginal - placental edge at margin of internal os
Low-lying
placenta within 2 cm of os
Placenta Previa: Incidence
Most common abnormal placentation
Accounts for 20% of all antepartum hemorrhage
Often resolves as uterus grows
~ 1:20 at 24 wk.
1:200 at 40 wk.
Nulliparous - 0.2%
Multiparous - 0.5%
Placenta Previa: Risk factors and
associations
Prior cesarean delivery/myomectomy
Prior previa (4-8% recurrence risk)
Previous abortion
Increased parity
Multifetal gestation
Advanced maternal age
Abnormal presentation
Smoking
Placenta Previa: Symptoms
Painless vaginal bleeding
Spontaneous
After coitus
Contractions
No symptoms
Routine ultrasound finding
Avg gestational age of 1st bleed, 30 wks
1/3 before 30 weeks
Placenta Previa: Physical Findings
Bleeding on speculum exam
Cervical dilation
Bleeding a sx related to PTL/normal labor
Abnormal position/lie
Non-reassuring fetal status
If significant bleeding:
Tachycardia
Postural hypertension
Shock
Placenta Previa: Diagnosis
Ultrasound
Abdominal 95% accurate to detect
Transvaginal (TVUS) will detect almost all
Consider what placental location a TVUS may find that was
missed on abdominal
Physical/speculum exam
remember: no digital exams unless previa RULED OUT!
Placenta Previa: Management
Initial evaluation/diagnosis
Observe/admit to L&D
IV access, routine (maybe serial) labs
Continuous electronic fetal monitoring
Continuous at least initially
May re-evaluate later if stable, no further bleeding
Delivery???
Placenta Previa: Management
Less than 36 wks gestation - expectant management if
stable, reassuring
Bed rest (negotiable)
No vaginal exams (not negotiable)
Steroids for lung maturation (<32 wks)
Possible mgmt at home after 1st bleed
70% will have recurrent vaginal bleeding before 36
completed weeks requiring emergent cesarean
Placenta Previa: Management
36+ weeks gestation
Cesarean delivery if positive fetal lung maturity by
amniocentesis
Delivery vs expectant mgmt if fetal lung immaturity
Schedule cesarean delivery @ 37 weeks
Discussion/counseling regarding cesarean hysterectomy
Note: given stable maternal and reassuring fetal
status, none of these management guidelines are
absolute (this is why OB is so much fun!)
Placenta Previa: Other considerations
Placenta accreta, increta, percreta
Cesarean delivery may be necessary
History of uterine surgery increases risk
Must consider these diagnoses if previa present
Could require further evaluation, imaging (MRI
considered now)
NOT the delivery you want to do at 2 am
Vasa Previa: Definition
In cases of velamentous cord insertion fetal vessels
cover cervical os
Vasa Previa: Incidence
0.1-1.0%
Greater in multiple gestations
Singleton - 0.2%
Twins - 6-11%
Triplets - 95%
Vasa Previa:
Symptoms, Findings, Diagnosis
Painless vaginal bleeding
Fetal bleeding
Positive Kleihauer Betke test
Ultrasound
Routine vs at time of symptoms
Vasa Previa: Management
If bleeding, plan for emergent delivery
If persistent bleeding, nonreassuring fetal status,
STAT cesarean… not a time for conservative
mgmt!
Fetal blood loss NOT tolerated
Third Trimester Bleeding: Other Etiologies
Cervicitis
Infection
Cervical erosion
Trauma
Cervical cancer
Foreign body
Bloody show/labor
Perinatal Morbidity and Mortality
Previa
Decreased mortality from 30% to 1% over last 60 years
Now emergent cesarean delivery often possible
Risk of preterm delivery
Abruption
Perinatal mortality rate 35%
Accounts for 15% of 3rd trimester stillbirths
Risk of preterm delivery
Most common cause of DIC in pregnancy
Massive hemorrhage --> risk of ARF, Sheehan’s, etc.
Postpartum Hemorrhage:
Definition and Differential Diagnosis
EBL >500 cc, vaginal delivery
EBL >1000 cc, cesarean delivery
Differential Diagnosis:
Uterine atony
Lacerations
Uterine inversion
Amniotic fluid embolism
Coagulopathy
Risk Factors for Postpartum Hemorrhage
Prolonged labor
Augmented labor
Rapid labor
h/o prior PPH
Episiotomy
Preeclampsia
Overdistended uterus (macrosomia, twins, hydramnios)
Operative delivery
Asian or Hispanic ethnicity
Chorioamnionitis
Uterine Atony
(same overall mgmt regardless of delivery type)
Recognition
Uterine exploration
Uterine massage
Medical mgmt:
Pitocin (20-80 u in 1 L NS)
Methergine (ergonovine maleate 0.2 mg IM)
Not advised for use if hypertension
Hemabate (prostaglandin F2 mg IM or intrauterine)
Uterine Atony
B-lynch suture (to compress uterus)
Uterine artery ligation
Must understand anatomy
Risk of ureteral injury
Uterine artery embolization
Typically an IR procedure
Plan “ahead” and let them know you may need them
Hysterectomy (last resort)
Anesthesia involved
Whether in L&D room or the OR!!!
Lacerations
Recognition
Perineal, vaginal, cervical
All can be rather bloody!
Assistance
Lighting
Appropriate repair
Control of bleeding
Identify apex for initial stitch placement
Uterine Inversion
Uncommon, but can be serious, especially if
unrecognized
Consider if difficult placental delivery
Consider if cannot recognize bleeding source
Consider… always!
Delayed recognition is bad news
Patient can have shock out of proportion to EBL
(though not all sources will agree on this)
Uterine Inversion
Management
Call for help
Manual replacement of uterus
Uterotonics to necessary to relax uterus & allow
thorough manual exploration of uterine cavity
IV nitroglycerin (100 g)
Appropriate anesthesia to allow YOU to manually
explore uterine cavity
Concern for shock… to be discussed (and managed by
the help you’ve called into the room!)
Exploratory laparotomy may be necessary
Amniotic Fluid Embolism
High index of suspicion
Recognition
Again… call for help!
Supportive treatment
Replete blood, coagulation factors as able
Plan for delivery (if diagnose antepartum) if able to
stabilize mom first
Management of Shock
Stabilize mother
Large-bore IV x 2
Place patient in Trendelenburg position
Crossmatch for pRBCs (2, 4, more units)
Rapidly infuse 5% dextrose in lactated Ringer’s
Monitor urine output
Ins/Outs very important
(and often not well-recorded prior to emergency situation --
how many times did she really void while in labor??? How
dehydrated was she when presented???)
By the way… get help (calling for help works quickly on
L&D!)
Management of Shock
Serial labs
CBC and platelets
Prothrombin time (factors II, V, VII, X {extrinsic})
Partial thromboplastin time (factors II, V, XIII, IX, X,
XI {intrinsic})
Management of Shock
Transfusion products
Product
Content
Volume
Whole blood
RBCs, 2,3 DPG, coagulation factors (50
V, VIII), plasma proteins
500 cc
Packed RBCs
RBCs
240cc
Platelets
55 x 106 platelets/unit
50cc
Fresh frozen plasma
Clotting factors V, VIII, fibrinogen
200-250cc
Cryoprecipitate
Factor VIII; 25% fibrinogen, von
Willebrand’s factor
10-40cc
Indications for Transfusion
No universally accepted guidelines for replacement of blood
components
If lab data available, most providers will transfuse patients with
hemoglobin values less than 7.5 to 8 g/dL
If no labs, it is reasonable to transfuse 2 units of packed red
blood cells (pRBCs) if hemodynamics do not improve after the
administration of 2 to 3 liters of normal saline and continued
bleeding is likely.
Management of Shock
Risks of blood transfusion
Infectious Disease
Risk Factor
Hepatitis B
1/200,000
Hepatitis C
1/3,300
HIV
1/225,000
CMV
1/20
MTLV-1/11
1/50,000
Management of Shock
Risks of blood transfusion
Immunologic reactions
Fever - 1/100
Hemolysis - 1/25,000
Fatal hemolytic reaction - 1/1,000,000
Management of Shock
Delivery
Vaginally unless other obstetrical indication, i.e.
fetal distress, herpes, etc.
Best to stabilize mother before initiating labor or
going to delivery
Bottom Line Concepts
Common causes of third trimester bleeding - Abruption,
previa, preterm labor, labor
NO DIGITAL EXAMS until placenta previa has been ruled out
Ultrasound – can use to evaluate previa but not accurate to
diagnose abruption
Postpartum hemorrhage refers to EBL >500 cc, vaginal
delivery or EBL >1000 cc, cesarean delivery
Most common cause of PPH – uterine atony
No universal rule for when to transfuse – decision made with
clinical judgment and based on each patient’s individual
circumstance and presentation
References and Resources
APGO Medical Student Educational Objectives, 9th edition, (2009), Educational Topic
23, 27 (p48-49, 56-57).
Beckman & Ling: Obstetrics and Gynecology, 6th edition, (2010), Charles RB
Beckmann, Frank W Ling, Barabara M Barzansky, William NP Herbert, Douglas
W Laube, Roger P Smith. Chapter 12, 21 (p133-39, 207-11).
Hacker & Moore: Hacker and Moore's Essentials of Obstetrics and Gynecology, 5th
edition (2009), Neville F Hacker, Joseph C Gambone, Calvin J Hobel. Chapter 10 (p128136).
Baron F, Hill WC. “Placenta previa, placenta abruption”, Clinical Obstetrics and
Gynecology, Sep 1998 41(3) pp527-532.
Benedetti T. Obstetric hemorrhage, in obstetrics: normal and problem pregnancies,
Gabbe S, Niebyl J, Simpson J, 3rd ed. New York: Churchill Livingston 1996, pp161-184.
Hertzberg B. “Ultrasound evaluation of third trimester bleeding,” The Radiologist, July
1997 4(4) pp227-234.
Sheiner E, Shohan-Vardi I. “Placenta previa: obstetric risk factors and pregnancy
outcome,” Journal of Maternal-Fetal Medicine, December 2001 10(6) pp414-418.
Jacobs, Allan J. “Management of postpartum hemorrhage at vaginal delivery.”
UpToDate. May 2011