Aerobic Gram-Positive Cocci Assessment 1.
advertisement

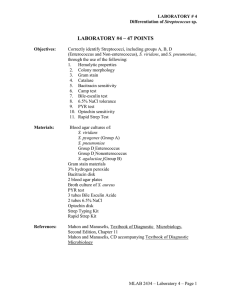
Aerobic Gram-Positive Cocci Assessment 1. What type of hemolysis on blood agar is described as complete clearing of blood around a colony? a. Alpha b. Beta c. Gamma d. Alpha-prime 2. Growth on media and colony morphology: BAP - Abundant small, white, glistening, opaque, entire, raised and buttery colonies; non-hemolytic Mac - No growth Gram stain - G+ cocci in cluster Of the organisms listed, which is the most probable? a. b. c. d. S. epidermidis S. aureus E. coli There is no way to determine the possible identification with the information provided. 3. Which of the following are NOT characteristic of Staphylococcus species? a. Catalase positive b. Gram positive c. Appear singly, in pairs and in clusters d. Lactose positive 4. A multisystem infection caused by S. aureus characterized by high fever, hypotension, and shock that has been associated with the use of tampons is: a. Scalded skin syndrome (SSS) b. Impetigo c. Toxic shock syndrome (TSS) d. Topic epidermal necrosis 5. The main type of infection caused by S. epidermidis is: a. Impetigo b. Osteomyelitis c. Hospital acquired infection resulting from instrumentation procedures, such as catheterization 6. Pathogenicity of S. epidermidis is increased by the organism=s ability to produce: a. Slime b. Lipid A c. Capsule d. Acid-fast properties 7. The main type of infection caused by S. saprophyticus is: a. Osteomyelitis b. Urinary tract infections in young, sexually active females c. Endocarditis d. Food poisoning 8. What is the NEXT test that should be performed to identify this organism? BAP - Abundant white, entire, glistening, raised, opaque, buttery colonies MAC - No growth Gram stain - G+ cocci in clusters a. Wet prep b. Catalase c. Coagulase d. Novobiocin susceptibility 9. S. saprophyticus can be differentiated from other coagulast-negative staphylococci by what test? a. Catalase b. Wet prep c. Coagulase d. Novobiocin susceptibility 10. The serious resistant strain of S. aureus that is becoming commonly seen in such places as high school gym classes is: a. MRSA b. MRSE c. VRSA d. VRSE 11. Match the following organisms with the correct Lancefield grouping: 1. Streptococcus pyogenes a. Group A 2. Enterococcus faecalis b. Group B 3. Streptococcus pneumoniae c. Group D 4. Streptococcus agalactiae d. Does not possess Lancefield antigens 12. Which of the following is strongly beta hemolytic? a. Group A b. Enterococcus c. Streptococcus pneumoniae d. viridans streptococcus 13. A throat culture is ordered on a 9 year-old boy who has fever and sore throat over a 3 day period. The culture has the following results: Abundant beta hemolytic colonies on BAP which are resistant to bacitracin. What is the most probable organism? a. Group A strep b. Group C strep c. Group D strep d. Based on these results, the organism cannot be identified. 14. A sputum culture is ordered on an elderly patient with symptoms consistent with pneumoniae. Alpha-hemolytic colonies that are sensitive to optochin are found in the culture. The infecting organism is: a. Group A strep b. Group B strep c. Streptococcus pneumoniae d. viridans streptococcus 15. A wound culture after 24 hour incubation produces tiny beta-hemolytic colonies on BAP. Gram stain reveals them to be G+ cocci in pairs, clusters and chains. The NEXT step in identifying this organism is: a. Bacitracin sensitivity b. Bile esculin hydrolysis c. Coagulase d. Catalase 16. A surgical wound infection has produced G+ cocci on BAP. The colonies are small, light grey, semi-opaque, and non-hemolytic. Catalase is negative. What is the next test that should be performed to identify this organism? a. Bacitracin sensitivity b. Optochin sensitivity c. Bile esculin or PYR d. Repeat the catalase, as it should not be negative 17. You suspect this urine is growing Group D Enterococcus. You have performed a bile esulin test and get blackening on the bile esculin slant. To confirm this organism is Group D Enterococcus, what test should be performed next? a. 6.5% salt tolerance b. Bacitracin sensitivity c. Optochin sensitivity d. Blackening on the bile esculin slant does not indicate that this organism is Enterococcus 18. Timmy Jo=s mother brings him to the pediatrician with a sore throat and fever. The pediatrician suspects strep throat and collects a swab for a rapid strep test, which is negative for strep. What should the pediatrician do? a. Assume the rapid strep test results are incorrect and go ahead and put Timmy Jo on antibiotics b. Assume the rapid strep test results are correct and do NOT prescribe antibiotics for Timmy Jo c. Collect another swab and repeat the rapid strep test d. Collect another swab for a throat culture 19. Which of the following best describes Group B strep? a. Non-hemolytic, optochin sensitive b. Hemolytic, CAMP test positive c. Hemolytic, PYR positive d. Non-hemolytic, bacitracin sensitive, optochin resistant 20. If untreated or poorly treated, what are the sequelae resulting from streptococcal pharyngitis? a. Rheumatic fever b. Acute glomerulonephitis c. Impetigo d. a and b