Chapter 21 – Chlamydia, Mycoplasma, & Ureaplasma Species
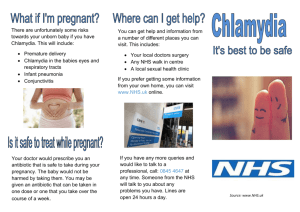
advertisement

Chapter 21 – Chlamydia, Mycoplasma, & Ureaplasma Species MLAB 2434 – Clinical Microbiology Cecile Sanders & Keri Brophy-Martinez Chlamydia Characteristics Unique growth cycle because they are deficient in independent energy metabolism; therefore they are obligate intracellular parasites Replication involves elementary body (EB) and reticulate body (RB) Life Cycle of Chlamydia EB infects host cell by inducing energyrequiring active phagocytosis EB organize into large, reticulating initial bodies, which divert the cells’ synthesizing functions to their own needs and begin to multiply by binary fission Organisms begin reorganizing into infective EBs. Disrupted host cell dies, releasing new EBs Life Cycle of Chlamydia Chlamydia pneumoniae Most recognized species of Chlamydia Important respiratory pathogen (acute respiratory disease, pneumonia, and pharyngitis) Implicated in asthma Risk factor for Guillain-Barre’ syndrome Chlamydia pneumoniae (cont’d) Common (50% of adults have antibodies) College age students most susceptible Reinfection common Prolonged sore throat and hoarseness, followed by flu-like lower respiratory symptoms Can be following by pneumonia and bronchitis Third most common respiratory infection Chlamydia pneumoniae (cont’d) If cultured, must be in cells (obligate intracellular pathogen) and then visualized with fluoresceinconjugated antibodies Serologic tests are method of choice for detection (Four-fold rise in titer) Chlamydia trachomatis Most commonly sexually transmitted bacterial pathogen in U.S. Only HPV is a more commonly sexually transmitted disease Adult males • Non-gonococcal urethritis (NGU) • Epididymitis and prostatitis Chlamydia trachomatis (cont’d) Adult females • Urethritis, follicular cervicitis, endometritis, proctitis, salpingitis, PID and perihepatitis (Fitz-Hugh-Curtis syndrome) Major cause of sterility in U.S. May be transmitted to newborns during delivery Chlamydia trachomatis (cont’d) Other sites of infection Trachoma – infection of the conjunctiva, resulting in scarring and blindness (Mostly in India and Egypt) Lymphogranuloma verereum – STD found in immigrants Chlamydia trachomatis (cont’d) Laboratory Diagnosis Direct microscopic examination to find EBs (p. 646) Cell culture Enzyme immunoassay Nucleic acid probes with and without amplification (PCR) Serologic (antibody) assay Chlamydia psittaci Causes psittacosis (parrot fever) Identification based on history of close contact with birds and serologic evaluation Mycoplasma and Ureaplasma Species General Characteristics Once thought to be viruses because of size Mycoplasmas are the smallest freeliving organism in nature Three human pathogens • Mycoplasma pneumoniae - respiratory • Mycoplasma hominis - urogenital • Ureaplasma urealyticum - urogenital Mycoplasma and Ureaplasma Species (cont’d) Pleomorphic organisms – do not have a cell wall (resistant to cell-wallactive antibiotics) Slow growing, highly fastidious, facultative anaerobes Require complex media for growth Clinical Infections Mycoplasma pneumoniae Causes bronchitis, pharyngitis, or primary atypical pneumonia (a.k.a. “walking pneumonia”) Usually infects school-age children and young adults in close quarters (dorms, military barracks, etc.) 50% of infections produce “cold agglutinins” Most often diagnosed by serologic evaluation M. hominis & U. urealyticum Most often associated with urogenital tract infections May be isolated from asymptomatic individuals Can be transmitted to the fetus at delivery Laboratory Diagnosis Cultures must be delivered immediately to the lab, because the organisms are very susceptible to drying Should be placed in transport media If not plated immediately, should be frozen at -70°C Most infections detected via serologic evaluation