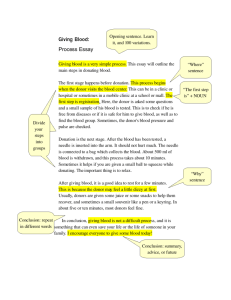
I. Blood Collection donor blood
advertisement

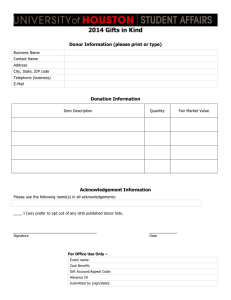
I. Blood Collection An overview of the process involved in collecting donor blood Donor Screening Starts with the donor and first impressions are critical Clean, well lit donation facility from waiting room to collection area Pleasant, professional staff who can ask the appropriate questions, observe and interpret the responses, and ensure that the collection process is as pleasant as possible Blood Bank versus Blood Center Confusion exists and terms are sometimes used inappropriately Blood bank in a hospital is also known as the transfusion service, performs compatibility testing and prepares components for transfusion Blood Center is the donation center, screens donors, draws donors, performs testing on the donor blood, and delivers appropriate components to the hospital blood bank Standards, Regulations, Governing Bodies Strict guidelines exist and inspections are performed in both blood centers and blood banks to ensure the safety of the donors and patients Some or all of the following agencies may be involved: AABB – American Association of Blood Banks FDA – Food and Drug Administration CAP – College of the American Pathologists JCAHO - Joint Commission on the Accreditation of Hospital Organizations NCCLS – National Committee for Clinical Laboratory Standards Donor Screening Medical History based on a standardized questionnaire obtains critical information about the donor’s health and risk factors which may make it unsafe for donation Physical Exam which includes blood pressure, temperature, pulse and screen for anemia are performed to ensure donor is healthy enough to donate. Two goals of screening Protect the health of the potential donor Protect the health of the potential recipient Donor Registration Donor signs in Written materials are given to the donor which explains high risk activities which may make the donor ineligible Donor must be informed and give consent that blood will be used for others unless they are in a special donor category First time donors must provide proof of identification such as SS#, DL#, DOB, address and any other unique information. Repeat donors may be required to show DL or some other photo ID Frequency of donation Whole blood or red blood cells 8 weeks Plateletpheresis – up to 24 times/year Plasmapheresis– once every 4 weeks, can be done twice a week Granulocytes Medical History A thorough history is obtained each time Standardized universal questionnaire is used Questions are asked that are very intimate in nature but are critical in assessing HIV or HBV risks Medications the donor taking are present in plasma, may cause deferral Infections the donor has may be passed to recipient, may be cause for deferral 12 Month Deferral Any intimate sexual relations with HIV positive, HBV positive, hemophiliacs, drug users or individuals receiving drugs/money for sex. Recipient of blood, components or blood products such as coagulation factors Sexually transmitted disease-if acquired indicates safe sex not practiced and donor at risk for HIV and HBV Travel to malarial endemic country Temporary Deferrals Certain immunizations 2 weeks -MMR, yellow fever, oral polio, typhoid 4 weeks -Rubella, Chicken Pox 2 months – small pox Pregnancy – 6 weeks upon conclusion Certain medications Proscar/Propecia, Accutain – 1 month Avodart – 6 months Soriatane – 3 years Tegison - permanent Permanent Deferrals HIV, HBV, or HCV positive Protozoan diseases such as Chagas disease or Babesiosis Received human pituitary growth hormone Donated only unit of blood in which a recipient contracted HIV or HBV Was the only common donor in 2 cases of posttransfusion HIV or HBV in recipient Lived in a country where Creutzfeld-Jacob disease is prevalent Most cancers except minor skin cancer and carcinoma insitu of the cervix Severe heart disease, liver disease Helpful Hint Permanent deferral – any member of high risk group such as: HIV/HBV/HCV pos, drugs/sex for money, cancer, serious illness or disease, CJD, Chagas disease, Babesiosis 12 month deferral – sex with any high risk group, any blood exposure, recipient of blood/blood products, STD, jail/prison, rabies vaccine after exposure, HBIG, malaria Have to memorize: medications and vaccinations Self-Exclusion Two stickers “Yes, use my blood” “No, do not use my blood” After interview the donor will place the appropriate bar coded label on the donation record If “no” selected the unit is collected, fully tested, but not used for transfusion Allows donors who know they are at risk to “save face” if pressured to donate by friends and family Donor Categories “Allogeneic”, “homologous” and “random donor” terms used for blood donated by individuals for anyone’s use Autologous – donate blood for your own use only Recipient Specific Directed donation – donor called in because blood/blood product is needed for a specific patient Directed Donor – patient selects their own donors Therapeutic bleeding – blood removed for medical purposes such as in polycythemia vera. NOT used for transfusion. Auto/Directed Blood Labels Donor Categories Safest is autologous, blood is your own, no risk of disease acquisition Most dangerous is Directed Donor, you select a donor who may, unknown to you, be in a high risk category but feels obligated to follow through and donate Blood Collection Collection of Blood Materials used are sterile and single use. Most important step is preparing the site to a state of almost surgical cleanliness. Bacteria on skin, if present, may grow well in stored donor blood and cause a fatal sepsis in recipient Use 16-17 gauge needle to collect blood from a single venipuncture within 15 minutes Collect 450 +/- 45 mLs of blood Donor Reactions Syncope (fainting) Hyperventilation Remove needle immediately Have donor rebreathe into paper bag. Nausea/vomiting Twitching/muscle spasms Hematoma Convulsions – rare, get immediate assistance Cardiac difficulties Post-Phlebotomy Care Donor applies pressure for 5 minutes Check and bandage site Have donor sit up for few minutes Have donor report to refreshment area for additional 15 minutes of monitoring Post-Phlebotomy Instructions Eat/drink before leaving Wait until staff releases you Drink more fluids next 4 hours No alcohol until after eating Refrain from smoking for 1 hour If bleeding continues apply pressure and raise arm Faint or dizzy sit with head between knees Abnormal symptoms persist contact blood center. Remove bandage Testing Donor Blood CANNOT rely on previous testing Records must be kept for 5 years Serological Testing ABO/D typing Antibody Screen – if positive, ID antibody, cannot make plasma products Antibodies to other blood group antigens which are present in the donor may react with recipient red cells resulting in a reaction. Disease Testing Disease testing include: HBsAG HBc HCV HIV 1&2 HTLV I/II RPR NAT for HIV-1, HCV & WNV Results of Testing Tests for disease markers must be negative or within normal limits. Donor blood which falls outside these parameters must be quarrantined. Repeat testing, if still abnormal must dispose. Transfusion Service Testing The only repeat testing required is: ABO on red cell products D typing (IS) on D negative red cell products Plasma products (FFP, CRYO, PLTS) do not require any testing. Donor samples must be stored at 1-6C for at least 7 days after transfusion ADSOL unit transfused today must save sprig for one week Many facilities will pull a sprig from each donor during processing and save all sprigs for 49 days, regardless of expiration of unit Summary Blood collection starts with screening of the donor to: Ensure they are healthy enough to donate Ensure they do not have transmissible diseases Many organizations set standards and monitor all aspects of blood collection and administration. Collection of blood must be done in such a manner as to ensure sterility of the component. Testing of donor blood includes serological testing for ABO/D typing, antibody screening, and testing for markers indicating infection. The blood supply is NOT safe, only careful screening and testing can prevent, as much as possible, disease transmission.