Unit 3 Immunology and Complement Part 1 Terry Kotrla, MS, MT(ASCP)BB
advertisement

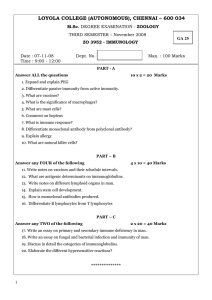
Unit 3 Immunology and Complement Part 1 Terry Kotrla, MS, MT(ASCP)BB Overview of Immunity Immunologic Response Three functions: Defense Homeostasis Surveillance Components of the Immune System Four components to be discussed: Cells and tissues of the immune system Monocyte-Macrophage Cell System T Lymphocytes (T cells) B lymphocytes (B cells) Cells and tissues of the immune system Pluripotential hematopoietic stem cells Located within the bone marrow, fetal liver and yolk sac of the fetus Stem cells differentiate into 2 types of “committed” stem cells Those which produce platelets, erythrocytes (red blood cells), monocytes or granulocytes. Those which produce cells of the lymphoid line only Hematopoietic Stem Cells Cells and Tissues of the Immune System Cells of the immune system are found within the blood, body tissues, thymus, spleen, liver, lymph nodes and body areas exposed to the external environment. These organs comprise the reticuloendothelial system (RES). Reticuloendothelial System Monocyte-Macrophage Cell System Derived from stem cell in the bone marrow. Monocytes circulate to sites of inflammation or migrate to various tissues. Macrophages have cell surface receptors, one of them being a receptor for the Fc portion of the immunoglobulin molecule. Tissue macrophages possess a receptor for the complement component C3b. The presence of antibody and/or complement enhances phagocytosis. The term used to describe any substance which enhances phagocytosis is “opsonin”. Macrophages Have receptors for Fc portion of immunoglobulin molecule. Antigens coated with antibody will be bound to macrophages. Causes removal through phagocytosis Have receptors for complement component C3b Antigens coated with C3b will bind to macrophages. Some blood group antibodies, especially ABO, are capable of activating complement. RBCs will be destroyed, cytolysis. Involved in cellular immunity, important in rejection of transplanted tissues. Monocyte-Macrophage Cell System Macrophages participate in phagocytosis, inflammation, and cellular immunity. Macrophages are mainly involved in nonspecific immunity and include the phagocytic cells: mononuclear phagocytes, polymorphonuclear phagocytes (neutrophils), eosinophils and mediator cells: basophils, mast cells and platelets. T Lymphocytes (T cells) Derived from stem cells in the bone marrow. Leave bone marrow and travel to the thymus to mature Approximately 75 to 80% of lymphocytes are T cells. Important in recognizing foreign material that is fixed in the tissues of cells. Do NOT secrete antibody Important in transplant rejection. Differentiate into different types. T Lymphocytes (T cells) Play an important role in regulating the production of antibodies by B cells T Helper cell T Suppressor cell T Cytotoxic cells (Killer T cells) T cells have surface proteins known as cluster determinants (CDs) Helper T cells are CD4 positive cells enhance and promote the action of other immune cells. Suppressor T cells are CD8 positive and have suppressive or cytotoxic effects 65% helper and 35% suppressor, ratio of 2:1, important in monitoring HIV infection. T Lymphocytes (T cells) Two T-cells, one which recognizes a target Activated T Cell B lymphocytes (B cells) Derived from stem cells in the bone marrow. Involved in humoral immunity Transform into plasma cells. Produce a family of proteins known as antibodies or immunoglobulins. Activated B cells begin antibody production and undergo a process called clonal expansion. Overview of Antibody Production Antigen presented to T cell and processed. Presented to B cell B cell produces specific antibody Antibody attaches to specific antigen Final Phase Memory Cells Immune Response Two types of immunity: Innate or nonspecific immune response. Adaptive or specific immune response. Innate immunity Involves the body’s first line of defense. Physical barriers which include intact skin and mucous membranes. Physiological factors. HCL in stomach Ciliated epithelium Flushing action of urine Unsaturated fatty acids on skin Sweat Tears Commensal normal flora Inflammation Inflammation is the body's reaction to injury and is known as the body's second line of defense which results in: Increased blood supply to the area. Increased capillary permeability. Migration of leukocytes into the surrounding tissue. These three events manifest symptoms which include pain, heat, redness and swelling. Adaptive (specific) Immunity Involves ability to recognize self and non-self. Encounters with non-self or foreign materials results in production of antibodies (humoral immunity) or actions of Tcells (cell mediated immunity). Interaction between both humoral and cell-mediated. Immunohematology primarily concerned with the causes and effects of humoral immunity. Antigen Any substance which is recognized as foreign by the body and is capable, under appropriate conditions, of provoking a specific immune response. It is capable of: Stimulating the formation of antibody and the development of cell-mediated immunity. Reacting specifically with the antibodies or T lymphocytes produced. Physical Nature of Antigens Foreign nature Molecular size Molecular complexity and rigidity Genetic factors Route of administration and dose – although not a “physical nature” important for response Antigenic Determinants or epitopes Structures on antigens that are recognized as foreign by the immune system. An immune response is directed against specific determinants and resultant antibodies will specifically bind to them. Multivalent antigens may elicit antibodies of different specificities. Antibodies produced in response to one antigen may cross react with other antigens having a common determinant. Blood bank concerned with allogeneic antigens (from other humans) and autologous (self) antigens. Epitopes Blood group antigens Chemical structures embedded in or protruding from RBCs, WBCs, and platelets and have three common forms: Glycoproteins - HLA system. Glycolipids - ABH, Lewis, Ii, and P blood group systems. Proteins - Rh, M, N blood group systems. Haptens Substances, usually of low molecular weight, that can combine with antibody but cannot initiate an immune response unless it is coupled to a larger carrier molecule. Most important in drug-induced hemolysis covered later in this course. Cellular Immunity Important defense mechanism against viral infections, some fungal infections, parasitic disease and against some bacteria, particularly those inside cells. Responsible for delayed hypersensitivity, transplant rejection and possibly tumor surveillance. T cells involved, T helper and T suppressor regulate intensity of immune response. Review your Immunlogy notes from Fall for more information. Cellular Immunity Lymphokines Attract neutrophils and monocytes to site of infection. Cause aggregation of macrophages at site of infection. Activate macrophages to phagocytose and destroy. Combined result is amplification of inflammatory reaction. The Humoral Immune Response Production of antibodies induced when the host's immune system comes into contact with foreign antigenic substance and reacts to this antigenic stimulation. Two types of responses: Primary Secondary (anamnestic) Mediated by B lymphocytes Primary Immune Response Antigen ingested by antigen processing cell (APC). Presented to helper T cell which as receptor for antigen. Activated helper T cell present the antigen to the B cells and secrete lymphokines which activates B cells. B cells proliferate and differentiate into plasma cells (which secrete antibody) and memory cells. Initially low affinity and avidity. IgM produced first, followed by IgG. Takes weeks to months. Secondary Immune Response Exposure to same antigen agan. Activates B memory cells to proliferate into plasma cells. Production of IgG antibody with high affinity and avidity. Some production of IgM due to immune cells which have not seen this antigen, but IgG is predominant antibody produced. Rapid production with high titer. Takes hours to days. Humoral Immune Response Antibody production occurs in four phases following antigen challenge: Lag phase when no antibody is detectable. Log phase in which antibody titer rises logarithmically. Plateau phase during which the antibody titer remains steady. Decline phase during which antibody levels gradually decline. Humoral Immune Response You must be able to differentiate a primary vs secondary immune response based on the following: Time Antibody Titer Antibody Class Antibody affinity and avidity These are critical to understanding reactions obtained in Blood Banking The following chart nicely illustrates the concepts. Memorize! End of Unit 3 Part 1