Unit 1 Part 1 Blood Collection Terry Kotrla, MS, MT(ASCP)

Unit 1 Part 1 Blood Collection
Terry Kotrla, MS, MT(ASCP)
MLAB 2431 Immunohematology
Introductory Comments
An overview of the process involved in collecting donor blood
Donor Screening
All blood comes from VOLUNTEER donors.
Screening performed to ensure donor is healthy.
Starts with the donor and first impressions are critical
Clean, well lit donation facility from waiting room to collection area
Pleasant, professional staff who can ask the appropriate questions, observe and interpret the responses, and ensure that the collection process is as pleasant as possible
Blood Bank versus Blood Center
Confusion exists and terms are sometimes used inappropriately
Blood bank in a hospital is also known as the transfusion service, performs compatibility testing and prepares components for transfusion
Blood Center is the donation center, screens donors, draws donors, performs testing on the donor blood, and delivers appropriate components to the hospital blood bank
Standards, Regulations, Governing Bodies
Strict guidelines exist and inspections are performed in both blood centers and blood banks to ensure the safety of the donors and patients
Some or all of the following agencies may be involved:
FDA – Food and Drug Administration – CBER and CFR
AABB
CAP – College of the American Pathologists
Joint Commission – inspects hospitals, lab included
CLSI – Clinical Laboratory Standards Institute
Donor Screening
Two goals or purposes for screening
Protect the health of the potential donor
Protect the health of the potential recipient
Four outcomes
Acceptance
Temporary deferral
Indefinite deferral
Permanent deferral
Three components of screening
Registration
Health history interview
Limited physical examination.
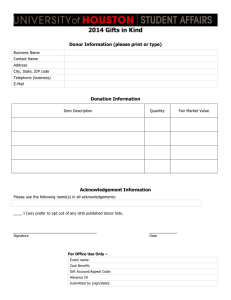
Donor Registration
Donor signs in
Written materials are given to the donor which explains high risk activities which may make the donor ineligible
Donor must be informed and give consent that blood will be used for others unless they are in a special donor category
First time donors must provide proof of identification such as
SS#, DL#, DOB, address and any other unique information.
Repeat donors may be required to show DL or some other photo
ID.
Donor Registration
Additional useful information
Name of patient or group to credit
Race
Unique donor characteristics
Donor must be provided with
HIV high risk activities
Warnings about donor reactions
Tests that will be performed and notification
Post phlebotomy care instructions
Medical History
Frequency of donation
Whole blood or red blood cells 8 weeks
Two unit red cell unit 16 weeks
Plateletpheresis – up to 24 times/year
Plasmapheresis– once every 4 weeks, can be done twice a week
Medical History
A thorough history is obtained each time
Standardized universal questionnaire is used
Questions are asked that are very intimate in nature but are critical in assessing HIV or HBV risks
Has donor ever been deferred, if “yes”, why.
Medications the donor is taking are present in plasma, may cause deferral
Infections the donor has may be passed to recipient, may be cause for deferral
Permanent Deferrals
Males who had sex with males OR engaged in sex for drugs or money since
1977.
Used IV drugs even ONCE in lifetime.
Taking clotting factors.
Hepatitis after age 11.
Cancer deferrals vary, some accept after period of being disease free others do not accept.
Lived in a country where Creutzfeld-Jacob disease is prevalent or family member with CJD.
Protozoan diseases such as Chagas disease or Babesiosis
Received human pituitary growth hormone.
Positive test for: HBsAg, Hepatitis C, HTLV I/II or HIV.
Donated only unit of blood in which a recipient contracted HIV or HBV
Was the only common donor in 2 cases of post-transfusion HIV or HBV in recipient
12 Month Deferral
Recipient of blood, components or blood products such as coagulation factors
Sexually transmitted disease-if acquired indicates safe sex not practiced and donor at risk for HIV and HBV
Received HBIG.
Accupuncture, tattoo, ear piercing
Needle stick
Rabies vaccine
Any intimate sexual relations with HIV or HBV positive, hemophiliacs, drug users or individuals receiving drugs/money for sex.
Temporary Deferrals
Certain immunizations
2 weeks -MMR, yellow fever, oral polio, typhoid
4 weeks -Rubella, Chicken Pox
2 months – small pox
Pregnancy – 6 weeks upon conclusion
Certain medications
Proscar/Propecia, Accutane – 1 month
Avodart – 6 months
Soriatane – 3 years
Tegison – permanent
Feldene – no platelet donation for 2 days.
Plavix and Ticlid – no platelet donation for 14 days
Malaria 3 years
West Nile virus 28 days
Helpful Hint
Permanent deferral – any member of high risk group such as: HIV/HBV/HCV pos, drugs/sex for money, cancer, serious illness or disease, CJD, Chagas disease,
Babesiosis
12 month deferral – sex with any high risk group, any blood exposure, recipient of blood/blood products,
STD, jail/prison, rabies vaccine after exposure, HBIG, malaria
Have to memorize : medications and vaccinations
Physical Examination
Evaluate general appearance
Weight – 110 1bs national, 123 lbs. Austin – eff. Jan 2010
Temperature 37.5 C OR 99.5F
Blood pressure
Systolic </= to 180 mm Hg
Diastolic </= 100 mm Hg
Hemoglobin and Hematocrit
Allogenic 12.5 g/dL or 38%
Autologous 11.0 g/dL or 33%
Self-Exclusion
Rescinded by FDA in 1992 but some blood centers may still use.
Two stickers
“Yes, use my blood”
“No, do not use my blood”
After interview the donor will place the appropriate bar coded label on the donation record
If “no” selected the unit is collected, fully tested, but not used for transfusion
Allows donors who know they are at risk to “save face” if pressured to donate by friends and family
Donor Categories
“ Allogeneic ”, “homologous” and “random donor” terms used for blood donated by individuals for anyone’s use
Autologous – donate blood for your own use only
Recipient Specific Directed donation – donor called in because blood/blood product is needed for a specific patient
Directed Donor – patient selects their own donors
Therapeutic bleeding – blood removed for medical purposes such as in polycythemia vera. NOT used for transfusion.
Auto/Directed Blood Labels
Donor Categories
Apheresis – removal of 1 component, return the rest
Leukapheresis
Plateletpheresis
Plasmapheresis
Stem cells
Bone marrow
Apheresis
Donor Categories
Safest is autologous, blood is your own, no risk of disease acquisition
Most dangerous is Directed Donor, you select a donor who may, unknown to you, be in a high risk category but feels obligated to follow through and donate
References
http://www.fda.gov/cber/dhq/dhq.htm
AABB Technical Manual 17 th edition.