Acute Myeloid Leukemias (AML) MLAB 1415: Hematology Keri Brophy-Martinez
advertisement

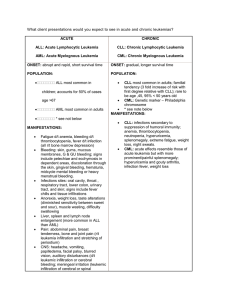
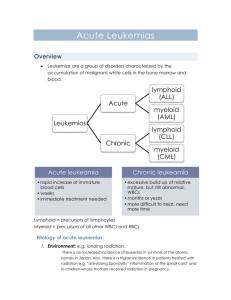
Acute Myeloid Leukemias (AML) MLAB 1415: Hematology Keri Brophy-Martinez Overview of AML Also known as Acute myelocytic leukemia Acute myelogenous leukemia Acute nonlymphocytic leukemia Stem cell disorder characterized by malignant neoplastic proliferation and accumulation of immature and nonfunctional hematopoietic cells in the BM Chemo/radiation Exposure to benzene History of MDS Overview of AML All acute leukemias begin BEFORE clinical signs and symptoms occur As the tumor volume expands, normal functional marrow cells decrease Characterized by two major features Ability to proliferate continuously Due to mutations affecting growth factors Transcription errors Arrested development of normal cells Lacks apoptosis Etiology • Classified by the cellular appearance of the primary stem cell • Common myeloid progenitor (CMP) • AML or ANLL • Common lymphoid progenitor (CLP) • ALL • Peak incidence in adults over 60 Clinical findings • CLASSIC TRIAD • Anemia • Infection • Bleeding/easy bruising/petechiae • Fever • Shortness of breath • Fatigue • Weight loss • Pallor Lab Features: Peripheral blood WBC count: variable at diagnosis ( 1-200 x 109/L) >20% blasts present Auer rods: fused primary granules in myeloblasts RBCs Decreased Hgb < 10g/dL Inclusions reflect rbc maturation defects Howell-Jolly, Pappenheimer, basophilic stippling nRBCs present Platelets Decreased Hypogranular, giant forms Megakaryocyte fragments Lab Features: MISC. • BONE MARROW • Hypercellular • Decreased fat content • >20 nonerythroid blasts • Fibrosis • MISC • Hyperuricemic • Increased LDH Who Classification of acute leukemia • • • • AML with recurrent genetic abnormalities AML with myelodysplasia- related changes AML and MDS- therapy related AML- not otherwise categorized WHO Classification of Acute Myelocytic Leukemias FAB Classification of Acute Leukemia Morphology MPO SBB Specific esterase Nonspecific esterase PAS M0 Acute myeloblastic leukemia: mimally differentiated >30% blasts No granules Not present Not present Not present Not present Not present M1 Acute myeloblastic leukemia with no maturation >30% blasts Few granules +/- Auer rods Present Present Can be Present Not present Not present M2 Acute myeloblastic leukemia with maturation >30% blasts Granules common + Auer rods Present Present Can be Present Not present Not present M3 Acute promyelocytic leukemia >30% blasts Prominent granules ++ Auer rods Faggot cells Present Present Present Not present Not present M4 Acute myelomonocytic leukemia >30% blasts >20%monocytes + Auer rods Present Present Present Present Not present M4 eo Acute myelomonocytic leukemia With eosinophilia >30% blasts >20%monocytes >5% abn eos + Auer rods Present Present Present Present Not present M5 Acute monoblastic leukemia with or withour maturation >30% blasts>80% monocytes with/without differentiation Can be Present Can be Present Can be Present Present Not present M6 Acute erythroleukemia >30% myeloblasts >50% megaloblasts + Auer rods Present: Myeloblasts Present: Myeloblasts Present: Myeloblasts Not Present Present: Erythroblasts M7 Acute megakaryocytic leukemia >30% Megakaryoblasts Cytoplasmic budding Not present Not present Can be Present Not present/Present Not present M1: AML without maturation • Myeloblast with Auer rod • High N:C ratio • Fine chromatin • Prominent nuclei M2: Aml with maturation All stages of neutrophil maturation >20% myeloblasts Auer rods common M3: promyelocytic leukemia (faggot cell) Faggot cells with bundles of Auer rods Genetic translocation t(15;17) Hypergranulation M4: Acute myelomonocytic leukemia (AMML) Monoblasts and promonocytes seen Some neutrophil precursors seen Vacuolization often seen M5: Acute monoblastic leukemia Monoblasts Promonocytes M6: Acute erythroid leukemia Striking poik High number of RBC precursors >20 Myeloblasts M7: Acute Megakaryoblastic Leukemia • Peripheral blood • • • • May see micromegakaryoblasts Megakaryocyte fragments Cytopenias Dysplastic segmented neutrophils and platelets • Bone marrow • Often get “dry tap” • Fibrosis Prognosis of all AMLs and therapy • Death often occurs from infection and hemorrhage in weeks to months unless therapy is started • Chemotherapy • Reduces tumor load • Bone marrow transplants References • McKenzie, Shirlyn B., and J. Lynne. Williams. "Chapter 21." Introduction. Clinical Laboratory Hematology. Boston: Pearson, 2010. Print