MLAB 2401: Clinical Chemistry Renal Assessment
advertisement

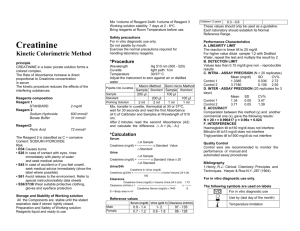
MLAB 2401: Clinical Chemistry Renal Assessment Nonprotein Nitrogen Compounds • What are they? – Products from the catabolism of proteins and nucleic acids – Consist of a molecule that contains nitrogen but are not part of a protein – Useful to evaluate renal function Clinically Significant NPN’s Analyte Plasma Concentration (%) Blood Urea Nitrogen (BUN) 45 Amino Acids 20 Uric Acid 20 Creatinine 5 Creatine 1-5 Ammonia 0.2 BUN • Blood Urea Nitrogen – Urea is the nitrogenous end-product of protein & AA metabolism. – Urea is formed in the liver when ammonia (NH3) is removed and combined with CO2. – Rises quickly as compared to creatinine – Majority excreted in urine – Most widely used screening test of kidney function BUN: Clinical Significance • Reference range 7-18 mg/dL • Decreased BUN – – – – Late pregnancy Decreased protein intake Severe liver disease Overhydration • Increased BUN – Azotemia • Occurs when BUN concentration exceeds 20 mg/dL • Not always due to kidney malfunction BUN / Creatinine Ratio – Normal BUN / Creatinine ratio is 12 – 20 to 1 – Pre-renal Azotemia Increased BUN due to non-renal causes Congestive heart failure, high protein diets, dehydration Increased Ratio- BUN is high/ creatinine is normal – Renal Azotemia Disease directly affects nephron Glomerulonephritis, Nephrotic syndrome, uremia, etc. Normal Ratio- both BUN and creatinine are proportionally elevated – Post-renal Azotemia Occurs after urine has left the kidney- due to obstruction Increased Ratio- BUN is high Plasma creatinine also elevated Specimen Requirements: BUN • • • • Plasma Serum 24-hour Urine nonhemolyzed BUN: Methodology • Kjeldahl – a classical method for determining urea concentration by measuring the amount of nitrogen present • Berthelot reaction - Good manual method - that measures ammonia – Uses an enzyme (urease ) to split off the ammonia • Diacetyl monoxide ( or monoxime) – Popular method but not well suited for manual methods • because ➵ Uses strong acids and oxidizing chemicals Creatinine/Creatine • Creatinine is formed from creatine and creatine phosphate in muscle • Metabolic product cleared entirely by glomerular filtration • Not reabsorbed • In order to see increased creatinine in serum, 50% kidney function is lost • Creatinine levels are affected by muscle mass, creatine turnover, and renal function Advantages of Creatinine • • • • Formed at a constant rate Readily excreted Not reabsorbed Not affected by diet Reference Range/Significance: Creatinine Significance • Evaluates renal function • Follows progress of renal disease Reference Range • Urine – 0.8-2.0gm/ 24 hour • Serum • Increased results – – – – Renal disease Decrease in GFR Obstruction in urinary system Decreased muscle mass – 0.5-1.5mg/dL Specimen requirements: Creatinine • • • • • Plasma Serum Urine ( 24 hour or random) Avoid hemolysis Avoid icterus Creatinine: Methodology • Jaffe reaction – basic reaction for creatinine – Kinetic • Principle: Protein-free filtrate(serum/urine) mixed with alkaline picrate solution forms a yellow-orange complex of creatinine picrate which absorbs light at 520 nm, proportional to the amount of creatinine present • Issues – Subject to interferences from proteins, glucose, uric acid, medications and others – Enzymatic • New technology involving coupled reactions Clearance Measurements • Evaluation of renal function relies on waste product measurement, specifically the urea and creatinine • Renal failure must be severe, where only 20% of the nephron is functioning before concentrations of the waste products increase in the blood • The rate that creatinine and urea are cleared from the body is termed clearance Clearance • Definition – Volume of plasma from which a measured amount of substance can be completely eliminated into urine per unit of time – Expressed in milliliters per minute • Function – Estimate the rate of glomerular filtration Creatinine Clearance • Used to estimate GFR ( glomerular filtration rate) • Most sensitive measure of kidney function • Mathematical derivation taking into effect the serum creatinine concentration to the urine creatinine concentration over a 24- hour period Creatinine Clearance Specimen requirements • 24-hour urine – Keep refrigerated • Serum/Plasma – Collected during 24-hour urine collection Instructions for urine collection • Empty bladder, discard urine, note exact time • Collect, save and pool all urine produced in the next 24-hours. • Exactly 24 hours from start time, empty bladder and add this sample to the collection Creatinine clearance Procedure – Determine creatinine level on serum/plasma - in mg/dL – Determine creatinine level on 24 hour urine • • • • measure 24 hr. urine vol. in mL, take a aliquot make a dilution (usually X 200) run procedure as for serum multiply results X dilution factor – Plug results into formula Formula Ucr(mg/dL) X V Ur(mL/24 hour) X P Cr(mg/dL) X 1440 minutes/ 24 hours 1.73 A • U cr= urine creatinine • P cr= serum creatinine • 1.73= normalization factor for body surface area in square meters • A= actual body surface area Nomogram 1. 2. 3. 4. Left side, find patient’s height( in feet or centimeters) On right side, find patient’s weight (lbs or kg) Using a straight edge draw a line through the points located Read the surface area in square meters, on the middle line Reference ranges • Males 97 mL/min- 137 mL/min • Females 88 mL/min-128 ml/min Creatinine Clearance Exercise • Female Patient: 5'6“ & 130 lbs. – Urine Creatinine – 98 mg/dL – Serum Creatinine – 0.9 mg/dL – 24 Hour Urine Volume – 1,200 mL – Set up calculation Drawbacks of Creatinine Clearance • Overestimates the GFR by 10-20% • Timing of serum/urine collection for accurate analysis • Patients/Health care workers must follow detailed instructions for proper collection New Ways to Evaluate eGFR • Estimates GFR from serum creatinine • Patients age, sex, weight, or race included in the equation • Common equation used include: – Modification of Diet in Renal Disease (MDRD) – Cockcroft-Gault – CKD-EPI Uric acid • Final breakdown product of nucleic acid catabolism - from both the food we eat, and breakdown of body cells. • Uric acid is filtered by the glomerulus, majority reabsorbed • Roles – Assess inherited purine disorders – Confirm diagnosis and treatment of gout – Assist in diagnosis of renal calculi – Prevent uric acid nephropathy during chemotherapy – Detect kidney dysfunction Clinical Significance: Uric Acid •Gout –Increased plasma uric acid –Painful uric acid crystals in joints –Usually in older males ( > 30 years-old ) –Associated with alcohol consumption –Uric acid may also form kidney stones • Other causes of increased uric acid – Leukemias and lymphomas » ( DNA catabolism ) – Megaloblastic anemias » ( DNA catabolism ) – Renal disease ( but not very specific ) Specimen Requirements: Uric Acid • • • • • Plasma Serum Urine Serum should be removed from cells ASAP Avoid lipemia Uric Acid: Methodology 1. Phosphotungstic Acid Reduction — This is the classical chemical method for uric acid determination. In this reaction, urate reduces phosphotungstic acid to a blue phosphotungstate complex, which is measured spectrophotometrically. 2. Uricase Method — An added enzyme, uricase, catalyzes the oxidation of urate to allantoin, H2O2, and CO2. The serum urate / uric acid may be determined by measuring the absorbance at 293 nm before and after treatment with uricase. (Uricase breaks down uric acid.) Uric acid + 2H2O + O2 Uricase > Allantoin + H2O2 + CO2 (Absorbs at 293 nm) (Nonabsorbing at 293 nm) Reference Range: Uric Acid • Reference values Men 3.5 - 7.2 mg/dL Women 2.6 - 6.0 mg/dL Other Screening Test for Renal Disease • Urinalysis – Routine urinalysis good indicator of renal disease • Microalbumin – Albumin is another sign of renal disease – Usually performed on a random urine Ammonia • Formed from the breakdown of amino acids and bacterial metabolism • Metabolized by the liver • Increases due to renal failure or liver disease are toxic to the CNS Specimen Requirements: Ammonia • Whole blood – EDTA – Heparin – Patient should not smoke several hours prior to collection, results in contamination Ammonia: Methodology 1. Glutamate dehydrogenase- enzymatic procedure 2 Oxoglutarate + NH4+ + NADPH Glutamate dehydrogenase Glutamate + NADP+ + H2O 2. NADP + is measured at 340 nm and it is directly proportional to ammonia. One final note… • Remember the Renal panel – – – – – – – – – – Albumin Glucose BUN Creatinine Calcium Chloride Potassium CO2 Sodium Phosphorus References • Bishop, M., Fody, E., & Schoeff, l. (2010). Clinical Chemistry: Techniques, principles, Correlations. Baltimore: Wolters Kluwer Lippincott Williams & Wilkins. • Sunheimer, R., & Graves, L. (2010). Clinical Laboratory Chemistry. Upper Saddle River: Pearson . 35