Austin Community College Medical Laboratory Technology MLAB 2360 Clinical I Urinalysis Objectives
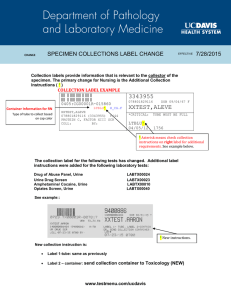
advertisement
Austin Community College Medical Laboratory Technology MLAB 2360 Clinical I Urinalysis Objectives The ACC MLT student is required to meet the following cognitive (knowledge), psychomotor (skill) and affective (attitude) objectives upon completion of the rotation. This document outlines the affective, cognitive and psychomotor objectives of the rotation. The student shall have the opportunity to demonstrate the ability to: I. Automated Urinalysis 1. 2. 3. Perform the analysis of patient urine specimens using the automated system. Perform or verify calibration or standardization of the instrument. Recognize instrument problems and warnings and perform procedures to correct these problems. following clinical preceptor demonstration and using the instrument manual and maintenance manual, perform, with minimal supervision, maintenance and troubleshooting procedures assigned by the clinical preceptor. Following clinical preceptor demonstration and using the procedure manual, perform without direct assistance, urine sample preparation prior to testing. 4. II. Physical and Chemical Urine Testing 1. Following clinical preceptor demonstration and using the procedure manual, perform without direct assistance, urine sample preparation prior to testing. 2. Using the procedure manual, perform without direct assistance assessment of physical characteristics of urine. 3. Using the procedure manual, perform without direct assistance, manual chemical testing of urine. 4. Using the procedure manual, perform without direct assistance, reducing substance testing of urine. III. Microscopic Urine Exam 1. Using the procedure manual, perform without direct assistance, urine sample preparation prior to microscopic examination. 2. Using the procedure manual, perform with minimal supervision, proper adjustment of the microscope to be used for microscopic exam. 3. Using the procedure manual, perform with minimal supervision, routine microscopic urine exam. 4. Compare chemical results to microscopic findings to verify results. Page 1 IV. Urine Pregnancy Test 1. Using the procedure manual, perform without direct assistance, urine sample preparation prior to pregnancy testing. 2. Using the procedure manual, and following clinical preceptor demonstration, perform with minimal supervision, pregnancy testing of urine V. Fecal Occult Blood (if applicable) 1. Using the procedure manual, state patient diet instructions prior to collecting sample for testing. 2. Using the procedure manual, state patient instructions for appropriate collection and application of sample to the fecal occult blood test cards. 3. Using the procedure manual, and following clinical preceptor demonstration, perform with minimal supervision, fecal occult blood testing. AFFECTIVE OBJECTIVES 1. Demonstrate initiative by reviewing objectives, theory and procedures prior to and regularly through out the rotation. 2. Demonstrate professionalism by: a. Report to clinical time on all scheduled days at assigned times b. Notify clinical preceptor as soon as possible of anticipated tardy. c. Notify clinical preceptor and MLT faculty of absence at least 30 minutes prior to scheduled arrival time. d. Using cell phones and MP3 only during designated break times. 3. Demonstrate enthusiasm and interest in the profession of clinical laboratory science. 4. Demonstrate an understanding of the concepts underlying clinical laboratory tests. 5. Use time in the clinical laboratory effectively to maximize productivity and learning. 6. Offer to help with the work load of the clinical laboratory when appropriate. 7. Use instructional guidance and constructive criticism to correct deficiencies and improve performance. 8. Work cooperatively with clinical preceptors, other laboratory personnel and other health care professionals. 9. Demonstrate the ability to concentrate and avoid distractions while performing laboratory work. 10. Perform laboratory work independently and without distractions. 11. Follow written and verbal instructions. 12. Perform laboratory work with accuracy, efficiency and precision. 13. Communicate in a clear and concise manner and record data accurately and legibly. 14. Recognize, report and resolve problems that may arise and take appropriate corrective action. 15. Demonstrate diligence in working through and resolving problems. 16. Assure that the laboratory work area is clean and well stocked. 17. After appropriate time and training, perform laboratory work with organization, accuracy, efficiency, precision and confidence. 18. Complete work on time and meet deadlines for assignments. Page 2 19. Maintain the confidentiality of patient information.. 20. Follow all safety guidelines of the MLT program and clinical site. 21. Conform to the clinical dress code. 22. Conform to the ASCLS Code of Ethics. SPECIMEN HANDLING AND PROCESSING 1. Following departmental protocol, demonstrate safe work practices by: a. Wearing personal protective equipment (PPE) as required. b. Handling and disposing of contaminated materials according to standard precautions. c. Handling chemicals according to safety procedures. 2. Explain the importance of proper collection and transport of specimens. 3. List criteria for evaluating specimen quality and corrective actions to resolve problems. 4. Evaluate specimen suitability for analysis using established criteria in the procedure manual. 5. Prepare specimen for analysis, mixing completely prior to allocating portions for macroscopic and microscopic testing. QUALITY ASSURANCE AND QUALITY CONTROL 1. Perform quality control analysis in the urinalysis laboratory. 2. Evaluate, with 95% accuracy, quality control results from a minimum of 4 days of testing. 3. Perform or discuss corrective action needed to be taken if quality control values are not within established limits. 4. Report or record quality control results according to the standard operating procedures of the laboratory with 95% accuracy. 5. List substances that will cause false negative and false positive results in a routine urinalysis. 6. State the confidentiality policy of the facility during testing procedure and reporting in accordance with HIPAA guidelines. 7. Observe basic computer applications where relevant. 8. Report all divergent or discordant results between quantitative and microscopic data to the clinical clinical preceptor. 9. Recognize all critical values and report these findings to the clinical clinical preceptor. TECHNICAL PROCEDURE - (PSYCHOMOTOR AND COGNITIVE) 1. Review the departmental procedure manual. 2. Perform a minimum of 40 analyses on urine specimens with 95% accuracy according to the following: a. Describe the physical appearance. noting and recording color and clarity of samples b. Perform specific gravity analysis using the refractometer and/or dipstick methods. c. Perform chemical analysis of the urine specimens. d. Interpret results obtained from chemical analysis. e. Where applicable, confirm abnormal results with appropriate confirmatory tests for a Page 3 minimum of 5 different abnormal urine specimens. f. Interpret the confirmatory test results. g. Perform a microscopic analysis. h. Compare results obtained from the chemical analysis with the microscopic analysis. i. Report discordant results between the chemical and microscopic analysis to the clinical preceptor. 3. Perform qualitative chemical tests using the test reagent strip correctly timing reactions according to the manufacturers instructions, reading and recording results. Results should agree to within 1 color block or 1/2 unit. 4. Perform microscopic analysis on urine specimens according to the standard operating procedure of the laboratory. 5. Compare results of reagent strip testing with microscopic data and bring discordant results to the attention of the clinical preceptor. 6. Identify and differentiate the common cell types found in urinary sediment. 7. Given a specimen or kodachrome, identify normal and abnormal constituents in a microscopic analysis of urine specimens with 95% accuracy. These constituents include: a. Erythrocytes b. Leukocytes c. Epithelial cells: squamous, transitional, renal d. Bacteria e. Yeast f. Casts: hyaline, fine and coarse granular, rbc, wbc, waxy g. Crystals: uric acid, calcium oxalate, triple phosphate, tyrosine, cystine, ammonium biurate h. Oval fat bodies i. Contaminants: fibers, talc, glass, etc. 8. Enumerate red blood cells and white blood cells in urinary sediment. 9. Identify the types of casts seen in urinary sediment and state the clinical significance associated with each finding. 10. Differentiate between crystals found in normal urine and crystals associated with clinical disease. 11. Describe typical urinary sediment findings and key biochemical findings associated with selected renal disorders. 12. Identify and differentiate the common cell types found in urinary sediment. 13. With 95% accuracy, correlate quantitative data with microscopic data 14. Correlate abnormal results with associated common disease states. 15. Operate automated dipstick readers with 100% accuracy. 16. State the reference (normal) values for all routine assays performed in the urinalysis laboratory. 17. For the following procedures perform with 95% accuracy in whichever department the procedure is performed: IF APPLICABLE a. Cerebrospinal fluid analysis to include cell count, differential b. Fecal occult blood c. Urine pregnancy test 18. Recognize cells specific to each body fluid type to include histiocytes, mesothelial cells, malignant cells, macrophage with inclusions, crystals, yeast, bacteria and others. If applicable. Page 4 19. Discuss or perform body fluid analysis on synovial, serous, and other fluids. 20. Interpret the results obtained from performing body fluid analysis on synovial, serous, and other fluids COGNITIVE OBJECTIVES 1. Define the following: a. oliguia b. anuria c. polyuria d. proteinuria e. glycosuria f. hematuria g. hemoglobinuria h. renal threshold i. diuresis j. orthostatic proteinuria k. nocturia l. diabetes insipidus m. Tamm-Horsfall protein n. glomerulonephritis o. pyelonephritis 2. For each of the following state the normal values, chemical reaction and correlate the origin and significance of the following chemical constituents usually found in urine by the multitest reagent strip methodology:: a. pH b. Blood c. Protein d. Nitrite e. Glucose f. Urobilinogen g. Ketone h. Specific gravity i. Bilirubin 3. State the principle and clinical significance of each of the following confirmatory tests: a. Sulfosalicylic acid test b. clinitest c. ictotest 4. State the clinical significance of each of the following: a. Erythrocytes b. Leukocytes c. Epithelial cells: squamous, transitional, renal Page 5 d. Bacteria e. Yeast f. Casts: hyaline, fine and coarse granular, rbc, wbc, waxy g. Crystals: uric acid, calcium oxalate, triple phosphate, tyrosine, cystine, ammonium biurate h. Oval fat bodies 5. Explain the principles of bright field, phase contrast, and polarized microscopy. 6. Explain the principle and methodology limitations of each test on the multi-test reagent strip. 7. Discuss the principle, methodology limitations, and clinical significance of the confirmatory tests used in the chemical analysis of urine, i.e., ictotest, sulfosalicylic acid, clinitest, and acetest. 8. Describe the anatomic structures involved in urine formation. 9. Describe the three parts of a complete urinalysis. 10. Describe three methods of enhancing the visualization of urinary sediment structures. 11. Explain the principle and methodology limitations of refractometry for urine specific gravity. Page 6