Animals and Allergens
advertisement

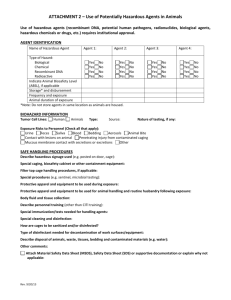
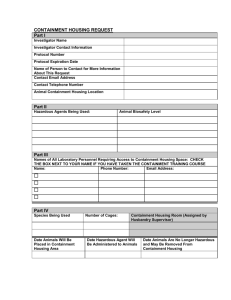
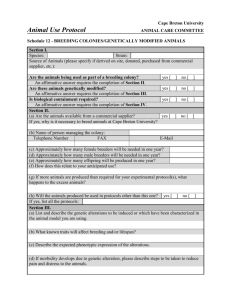
Animals and Allergens Risk Assessment for Work with Research Animals Risks associated with the research agent used in the animal chemical, physical, biological Risks associated with the species of animal used zoonotic agents Risks associated with animal maintenance ergonomic factors, bites, scratches, allergens Risks Associated with the Agent Used Chemical agents carcinogens, mutagens toxic chemicals anesthetics Physical agents radiation heat sound Risks Associated with the Agent Used Potentially biohazardous agents deliberate use of an infectious agent in animals for research purposes maintenance of infected animal for duration of experiment sacrifice, necropsy and harvesting of agent or infected tissue Transmission of Biohazards During Work with Animals Airborne Release of infectious aerosols by animal by sneezing, coughing Release during nasal infection or aerosol challenge Aerosolization from bedding and excreta During surgical procedures During birthing Transmission of Biohazards During Work with Animals Direct Inoculation Needlesticks during injection/inoculation process Bites and scratches from infected animal Transmission of Biohazards During Work with Animals Direct exposure of mucous membranes (by splash or splatter) During surgical procedures During injection During necropsy Transmission of Biohazards During Work with Animals Indirect transmission and ingestion From contaminated hands or gloves to mouth Facial contamination directly from animal Transfer of parasites by animal handling Indirect transmission with eye or mucous membrane exposure Dust from bedding Splash during cage washing “Dirty” environment Risk Reduction: Containment of Infectious Agent Containment must include: Primary containment Enclosed filtered caging system Biosafety cabinets Safety equipment PPE Secondary containment The containment facility • Negative pressurization • Nonrecirculated air supply • Ventilation must consider wellbeing of animal Containment Caging Systems No Containment Open (standard) cage Some Containment Filter top cage (microisolator cage) Full Containment Fully enclosed in ventilated rack Containment Caging Systems Microisolator Cage works like a Petri dish open gaps around lid edge allow limited air exchange may lead to more labor intensive husbandry due to moisture and ammonia buildup Containment Caging Systems Individual cages sealed into rack with supplied air under negative pressure Both supply and exhaust usually HEPA filtered Ventilation must control humidity and buildup of ammonia Containment Caging Systems Can install cages in class III biosafety cabinet Cages are completely contained with glove port access Very motion-limiting Transfer in and out may be an issue Containment Caging Systems BioBubble (Ft. Collins, CO) makes softwall ventilated enclosures Can be containment or barrier style Large equipment can be surface-mounted in wall Special Animal Housing Situations Barrier colonies Special breeds - often immunocompromised, “fragile”, expensive (SCID-Hu, nude athymics) Transgenics - often even more fragile and expensive (knockouts, microinjected, combos) Specific pathogen-free (SPF) - bred and raised to be missing certain specific microorganisms Isolation colonies Extensive SPFs and defined flora animals Gnotobiotes (an entirely different animal!) Zoonoses Zoonotic disease: A disease of animals that can be transmitted under natural conditions and cause disease in humans Wild caught animals most hazardous Random source animals (e.g., from a pound) are also a risk Purpose bred animals pose least risk Some Animals and Their Zoonoses Animal Macaque monkeys Sheep White mouse Dogs, cats, skunks, raccoons, bats Cattle, NHP Cats Parrots, macaws Chickens Disease Herpes B virus Q fever Hantavirus Rabies Tuberculosis Toxoplasmosis Psittacosis Avian influenza Rodent Zoonoses Rat bite fever (Streptobacillus moniliformis, Spirillum minus) transmission: direct contact (bites) Lymphocytic choriomeningitis (LCM, a virus) transmission: inhalation Leptospirosis (Leptospira spp.) transmission: inhalation Others include ringworm (fungal), scabies (mites, an ectoparasite) Transmission of Zoonoses Enteric route (fecal/oral) Salmonella, Shigella, Campylobacter, Giardia, Toxoplasma, Cryptosporidium, Entamoeba, Hepatitis A Respiratory route Q fever, Chlamydia, Measles Skin contact Ringworm (Tinea), Measles, Monkeypox Control of Zoonoses Get information on species and agent Quarantine animals prior to use Use Engineering controls written SOPs and manuals Use PPE facility construction and secondary barriers Consider the need for containment caging Use Administrative controls additional protection for worker Practice good facility and personal hygiene Provide staff training Laboratory Acquired Allergies (LAA) Significant occupational disease Affects >30% of all personnel working with animals No minimum safe exposure levels to allergens have been established Animal allergens found in hair, dander, urine, saliva, serum fel-d-l cat allergen (in saliva and thus on skin) is one of the strongest allergens known for humans Sources of Exposure to LAA Hair and dander shed from animal Urine and feces dried in bedding Particulates shed from bedding material Animal saliva Routes of Exposure to LAA Inhalation of airborne allergens during cage changing during animal handling Skin or eye contact usually indirect by touching skin, eyes Percutaneous exposure animal bites (saliva) Risk Factors for Development of LAA Exposure to allergens duration frequency intensity Previous allergic conditions Other predisposing conditions illness Immunocompromised pets LAA: Exposure Control Engineering Controls enclosure dilution ventilation Administrative Controls reduce time with animals reduce density of animals housekeeping practices Personal Protective Equipment respirators and clothing Medical Surveillance