Eliminating Barriers to Minority Participation in Clinical Trials Debra Wujcik, RN, PhD
advertisement

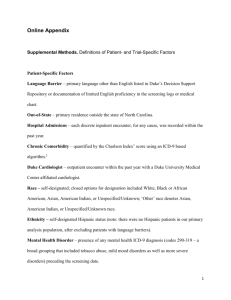
Eliminating Barriers to Minority Participation in Clinical Trials Debra Wujcik, RN, PhD Director Clinical Trials at Meharry Assistant Professor of Nursing History of Mistrust Background • Approximately 20% of adult cancer patients are medically eligible for a cancer clinical trial. • Less than 3% of adult cancer patients participate in a cancer clinical trials. – Accrual is even less for minority and medically underserved populations. • Studies show minority groups are as willing to participate as whites, but are less likely to be invited to participate. • Those who participate in clinical trials are more likely to be insured and have higher socioeconomic status. Presentation Outline • Cancer Clinical Trials Unit at Nashville General Hospital at Meharry • ENACCT Community Partners Project Program Development • 1998 – Nashville General Hospital moved to Meharry Medical College Campus • 2000 – Research team formed at MMC under U54 Partnership grant • 2003 – Minority Based Community Clinical Oncology Program Grant (MBCCOP) Assumptions • Vanderbilt studies would be opened at NGH and accrual would begin. • Minority and underserved persons don’t want to participate in research. Identification of Barriers to Care and Clinical Trial Participation • Missed appointments. – How does the patient enter the system? – Who makes the appointments? – Who reminds the patient? • Missed communication. – How does the physician know the pathology results? – How does the patient find out? • Missed rides. – Does the patient have transportation? – How reliable is the transportation? Identification of Barriers (cont.) • Lack of insurance. – Most patients present with no insurance • Indigent • Self pay on sliding scale and/or with discounts • TN Care • Lack of understanding. – Assess what the patient knows/understands. – Who influences patient? What do they know/understand? Procedure for Screening • All patients diagnosed at MMC are evaluated for study eligibility. – Cancer committee requested all patients with cancer be evaluated. • Pathology reports are sent to research staff. • Cases are identified and “managed” by the research team. – Team reports progress through the system and arranges appointments and referrals as needed for diagnostic work up and staging. Clinical Trial Accrual Rates 2001-2004 Year Screened Study Available Placed on study Total Accrual Rate Actual Accrual Rate 1 154 32 15 10% 47% 2 108 38 17 16% 45% 3 145 44 27 19% 43% 4 162 50 36 22% 44% Reasons patients did not go on study (2001-2004) • • • • • • • • • • • Co-morbidity Eligibility Performance status Refused treatment Dept of corrections Refused research Refused specific trial Returned to local MD Insurance Lost to follow up Transportation 19 17 12 8 5 3 3 2 1 1 1 72 27% 23% 17% 11% 7% 4% 4% 3% 1% 1% 1% Cases are identified and managed by the research team • • • Every patient is identified and screened. – Pathology reports are reviewed. – Abnormal screening results are reviewed. Information is entered into a database for review at weekly research team meeting. Patients are navigated through the system using: – Nurse navigator – Research nurse Model of Care Refined • Every patient is identified and screened. – – Pathology reports are reviewed. Abnormal screening results are reviewed. • Information is entered into a database for review at weekly research team meeting. • Patients are navigated through the system using: – – Nurse navigator Research nurse Model of Care Refined (cont.) • Physician is advised if a clinical trial available. – A plan to address obstacles such as transportation or medications is developed. • Clinical trial option is offered during initial treatment discussion. – Clinical trial is not an afterthought. – Patient is not referred elsewhere for clinical trial participation. Screened Patients Racial/Ethnic Distribution of Screened Patients 0% 1% 8% Black 46% White Hispanic Asian 45% Alaskan Screened Patients Insurance Distribution of Screened Patients 18% 38% 4% Uninsured Indigent TN Care 8% Medicare Commercial TDOC 16% 16% Screened Patients Gender Distribution of Screened Patients 36% Male Female 64% All Patients on Study 2005-2008 Racial/Ethnicity Distribution in Cancer Trials 120% 100% Hispanic 80% Pac Islander 60% White 40% Black 20% 0% 2005 2006 2007 2008 All Patients on Study 2005-2008 Gender Distribution in Cancer Trials 120% 100% 80% Female 60% Male 40% 20% 0% 2005 2006 2007 2008 Clinical Trial Accrual Rates Year Screened Study Available Placed on study Total Accrual Rate Actual Accrual Rate 1 154 32 15 10% 47% 2 108 38 17 16% 45% 3 145 44 27 19% 43% 4 162 50 36 22% 44% 5 138 29 19 14% 66% 6 184 59 53 29% 90% 7 234 91 66 28% 73% 21% 68% Ave Outcome of Screened Patients 2005-2007 Study available, pt. eligible 33% On study 30.0% Refused research 2.5% Treat off study 0.5% Study available, pt not eligible 5% Treat off study 4.5% No treatment offered 0.5% Study not applicable 8% Treat off study 7.0% No treatment offered 1.0% Study not available 50% Treat off study 46.5% No treatment offered Refused Treatment 3.5% 3% Wujcik, D & Wolff, SN. (2010). Recruitment of African Americans to national oncology clinical trials through a clinical trials shared resource. Journal of Health Care for the Poor and Underserved, 21: 37-52. Summary • Racial/ethnic minority and underinsured patients are willing to participate in cancer clinical trials. • A team approach and case management (navigation) strategies ensure success. • A proactive rather than reactive approach is needed. ENACCT Implementation Partners Project Education Network to Advance Cancer Clinical Trials • The only national organization solely devoted to community-centered approaches to cancer clinical trials education. • Dedicated to finding evidence based approaches that work to change attitudes, behaviors and ultimately, accrual. • http://www.enacct.org/ 25 Goals of Implementation Partners Project • To increase knowledge and improve attitudes about clinical trials among minority and underserved populations in Nashville, TN. • To identify community concerns and opportunities regarding clinical trials participation and make recommendations for future collaborations and interventions. • To identify community members interested in participating in ongoing initiatives. Objectives • Engage participants in discussion to identify common concerns and opportunities – Host six town hall meetings with guided discussion format – Show participants informational DVD. • Identify at least 6 community members interested in participating in ongoing initiatives such as advisory board members, IRB members, or community advocates Organizational Partners • Vanderbilt Ingram Cancer Center • Meharry-Vanderbilt-Tennessee State University Cancer Research Partnership • Clinical Trials Shared Resources – VICC CTSR – MMC/VICC Partnership CTSR • Tennessee Comprehensive Cancer Control Coalition – Middle TN Region Community Partners • Nashville Branch of the NAACP Health Committee • Cervical Cancer Coalition of Tennessee • Nashville Health Disparities Coalition • Nashville Latino Health Coalition • Super 60s of NGH • Dickson Community Health Council Town Hall Meetings • Sponsored by community partner • Target 20 participants • Agenda – Welcome and snacks – Educational DVD and print materials – Focused discussion, recorded for later transcription – Medical hero • Babysitting provided as needed • Participants receive $25 gift card Demographic Data • • • Attendance – Participants – F/U Volunteers Gender – Male – Female Education – Less than HS – Some HS – HS Graduate – College 96 49 • • 23 75 • 3 6 33 39 Average age 49 Race – White, Non Hispanic 7 – White, Hispanic 11 – Black 76 – Other 2 Research Exp – Yes 32 • Positive 23 • Negative 0 • Neutral 3 – No 64 In their own words…. • What is your experience with cancer – “It’s just amazing how fast it kills” – “I wanted to come today to say that I want to be a part of whatever I can to stop families from going through that” – “Men need to be teaching their families” In their own words…. • When you hear the word cancer, what comes to mind? – “The first thought that comes to mind is fight” – “I think about the connection between healing and spirituality” – “What comes to mind is what type, what stage, and what can be done because I know there’s hope” In their own words…. • What comes to mind when you hear the word research? – “We definitely need to get African American people involved” – “First thing I do is question the validity and then I question me doing it, and then I want to see somebody that looks like me doing it” – “…we still need to be careful about who’s doing the research” In their own words…. • When you hear the word research…. – “When we talk about the research, you can go back to Tuskegee and you have to remember, okay, the same people who we’re being asked to trust with our lives now, in research projects, are the same people who, you know, did this in Tuskegee” – “Once you figure out a treatment, am I going to be able to afford it? Is it going to be available to me? Is it going to be available to people like me? In their own words…. • What would motivate you to participate? – “Letting people know that we are furthering progress in treating something by the research” – “One of the main motivators in neighborhoods like where I come from is money…Money you know is the motivator and the thing is, there are people who are desperate enough in this time, black, white, whatever, but impoverished, who are going to say, you know what – I need that $20” – “The relationship with the primary physician” In their own words…. • What keeps you from participating? – “It’s the way it is presented – it is very intimidating and it’s overwhelming” – “A lot of times it’s the language that’s used because a lot times it’s lay people, it’s elderly people who don’t have a clue about the basic diagnosis, let alone a clinical trial” – “A lot of people can’t read” – “You know you need to be there, but due to the fact that you’re illiterate, the fact that you cannot understand, you’re not going to participate.” In their own words…. • What are thoughts about the video? – “It makes you want to sign up” – “It was a good video. But let’s not forget the fact that what this is, is basically targeted recruitment; you see what I am saying? And in recruitment, you have to look further than what you’re presented” – “As a people, especially African-American people, we need to be embraced, we need to be loved.” – “I feel we are seen and we are heard” Next Steps • Share findings with an advisory board made up of THM participants – Did we hear you correctly? – How can we use this information to change and improve the way we conduct our research? • Further engagement – Individual interviews exploring mistrust and fear – Train the trainer project – IRB training Questions?