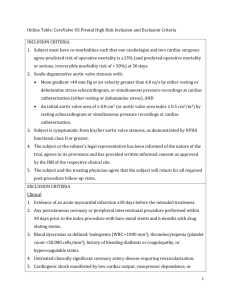
Board Review Vikram Chhokar MD University of Tennessee Division of Cardiology
advertisement
Board Review Vikram Chhokar MD University of Tennessee Division of Cardiology Question An 80-year-old Asian woman awakens at 2 a.m. feeling as if she were being smothered. She is brought to the ED and is found to be in pulmonary edema. She has a history of a heart murmur, discovered 20 years before. Prior to this episode she says she was in good health, although she has not been physically active due to arthritic discomfort for the past 5 years. On careful questioning she admits to brief episodes of pressure-like sensation in her chest especially when she becomes aggravated. Question Physical examination: BP 150/110 mmHg, pulse 120/min, respirations 24/min. Neck veins 10cm. Lungs have rales 3/4 the way up posteriorly bilaterally. Carotids are difficult to feel. PMI is in the 5th intercostal space just outside the midclavicular line and sustained. There is a grade II/VI systolic ejection murmur at the base and a grade II/VI diastolic blowing murmur at the 3rd left intercostal space. There is an S4 and an S3 gallop. There is no hepatomegaly and no pedal edema. Question Laboratory : Chest X-ray: slightly enlarged cardiac silhouette, pulmonary vascular redistribution and pulmonary edema. ECG: QS in V1, a small r in V2, a 25mm R wave in V5 and a 30mm R wave in V6. There is 2mm ST-segment depression in V4-6 . Echo: estimated EF 55%, first troponin <0.3 ng/ml. The patient is given O2, Lasix, digoxin, and enalapril and becomes less dyspneic. Her pulse decreases to 90/min and BP to 110/85 mmHg. Question The most probable diagnosis in this case is: A. Severe AR B Severe aortic stenosis C. Hypertensive cardiovascular disease. D. Acute non-ST-elevation myocardial infarction. E. Congestive heart failure with diastolic dysfunction. Answer The correct answer is B. The pulses and BP are against severe aortic regurgitation. Although the patient probably has angina, and even may have coronary artery disease, the presence of the systolic murmur, the poor arterial pulses, the severe LVH on ECG make aortic stenosis the likely diagnosis. Although the BP was elevated when she was in severe failure due to the excessive sympathetic stimulation and activated renin angiotensin system, when the patient was treated the BP returned to normal, inconsistent with acute heart failure due to hypertensive disease. Aortic Stenosis Etiology based on location Supravalvular SubvalvularValvular Supravalvular Aortic Stenosis Supravalvular Associated Elfin facies Hypercalcemia Peripheral pulmonic stenosis Thrill palpation in suprasternal notch or R but not L carotid artery Increased A2 Subvalvular Aortic Stenosis Subvalvular Presents with a high doppler velocity on outflow tract with normal AV on echo. Frequent AR due to aortic valve jet Looks like HOCM on echo with LAM Two subtypes Discrete- 10%, sec to subvalvular ridge Tunnel Valvular Aortic Stenosis Valvular Congenital (1-30 yrs old) Bicuspid (40-60 yrs old) Rheumatic (40-60 yrs old) Senile degenerative (>70 yrs old) Bicuspid Aortic Valve The most common congenital cardiac abnormality is bicuspid aortic valve affecting 12% of the U.S. population. Over time, one-third to one-half of such valves become stenotic, with significant narrowing of the aortic orifice typically developing in the 5th and 6th decades of life. Aortic Stenosis Key Points MCC of AS is senile degenerative changes In patients with AS due to rheumatic dz r/o “silent” mitral stenosis. Bicuspid or rheumatic should be suspected in pt with AS presenting in 5th or 6th decade of life. Pathophysiology Increase in afterload Decrease in systemic and coronary flow from obstruction Progressive hypertrophy Classic symptom triad Dyspnea Angina Syncope Classic symptom triad Once any of these classic symptoms develop, prognosis dramatically worsens. Thus, within 5 years of the development of angina, approximately 50% of patients will die unless aortic valve replacement is performed. For syncope, 50% survival is 3 years For congestive heart failure, 50% survival is only 2 years unless the valve is replaced. Angina 5, Syncope 3, and CHF 2. Characteristic Physical findings Dampened upstroke of carotid artery Sustained bifid left ventricular impulse Absent A2 Late-peaking systolic ejection murmur A concomitant systolic thrill indicates the presence of AS (mean gradient >50mm Hg) Of note if you have significant Physical finding and symptoms, you must rule out severe AS. Aortic Stenosis Patients with the physical findings of AS should undergo selected laboratory examinations, including an ECG, a chest x-ray, and an echocardiogram. The 2-D echocardiogram is valuable for confirming the presence of aortic valve disease and determining left ventricular (LV) size and function, degree of hypertrophy, and presence of other associated valve disease. EKG Usually shows NSR with LVH Note: If AF is present, concomitant mitral valve disease or thyroid dz must be suspected. Recommendations for Echocardiography in AS •Class 1 •Diagnosis and assessment of severity of AS. •Assessment of LV size, function, and/or hemodynamics. •Reevaluation of patients with known AS with changing symptoms or signs. •Assessment of changes in hemodynamic severity and ventricular compensation in patients with known AS during pregnancy. •Reevaluation of asymptomatic patients with severe AS. •Class IIa •Reevaluation of asymptomatic patients with mild to moderate AS and evidence of LV dysfunction or hypertrophy. •Class III •Routine reevaluation of asymptomatic adult patients with mild AS having stable physical signs and normal LV size and function. ECHO Modified Bernoulli equation (P=4v2) used to calculate gradient. A maximal instantaneous and mean AV gradient is derived from the continuous-wave Doppler velocity across the aortic valve. AVA can be estimated by continuity equation: AVA=LVOTarea LVOTTVI AVTVI ECHO/Doppler Pit Falls Will underestimate AS if Doppler beam is not parallel to AS velocity jet. Will rarely over-estimate mean gradient Severe anemia (hemoglobin <8.0 g/dl) Small aortic root Sequential stenoses in parallel (coexistent LVOT and valvular obstruction) Severity of AS Severity Mild Mean gradient AV area (mm Hg) (cm2) <25 >1.5 Moderate 25-50 1-1.5 Severe >50 <1.0 Critical >80 <0.7 Cath data “Pull back” tracing can be used in pt with NSR but not accurate in irregular rhythms or low-out put states. In low cardiac output, the stenosis may be severe, with a mean gradient <50mm Hg per echo. Gorlin equation can be used to calculate AVA from pressure gradients, independent of CO. AVA= (1000)(CO) (44)(SEP)(HR)(√P) Hakke formula Simple way to do things! Used to calculate AV area AVA=CO/(p-p gradient) Treatment AVR is clearly indicated in symptomatic patients. Management decisions are more controversial in asymptomatic patients. Patients with severe AS, with or without symptoms, who are undergoing CABG should undergo AVR at the time of revascularization. There is general consensus that patients with moderate AS (e.g., mean pressure gradient ≥30 mm Hg) should undergo AVR at the time of CABG, but controversy persists regarding the indications for concomitant AVR at the time of CABG in patients with milder forms of AS. Treatment Key Points Aortic valve replacement is indicated for patients with symptoms of severe AS, regardless of the LV ejection fraction. Coronary angiography may not be required preoperatively in younger patients without risk factors for CAD. Percutaneous aortic balloon valvuloplasy is reserved only for critically ill patients as a “bridge” to surgery. Asymptomatic patients with Severe AS “The most common cause of death in patients with severe aortic stenosis is an operation” The prevailing notion. Surgery should be performed at the onset of symptoms or LV systolic dysfunction. AS w/ low output/low gradient Exercise testing maybe performed to document exercise tolerance and hemodynamic response in pts with low CO. AS w/ low output/low gradient Question 55yo presents with DOE for past 6 months which is worsening. Pt has no significant PMH. PE: carotid upstroke 2+ delay but full volume, Second heart sound is single. There is a 3/6 SEM at RSB with mid-peak which ends at second heart sound. Echo: mild LVH, EF 65%, AV calcified and restricted. LVOT diameter is 2.0cm. Peak AV velocity is 2.5 m/sec with mean gradient of 18mm HG. LVOT velocity is 1.0 m/sec. What is the AVA? A. 0.5 cm2 B. 0.8 cm2 C. 1.0 cm2 D. 1.2 cm2 Answer AVA can be estimated by continuity equation: LVOT diameter is 2.0cm. Peak AV velocity is 2.5 m/sec with mean gradient of 18mm HG. LVOT velocity is 1.0 m/sec. The first step is to calculate the cross-sectional area of LVOT, as follows: CSA (LVOT) = π r2 = π(d/2)2. CSA (LVOT) = π r2 = π(d/2)2 = π(2/2)2 = π(1)2 = π The formula for calculated aortic valve area (AVA) is: AVA (cm2) = CSA (LVOT) x (Vmax LVOT) ÷ Vmax AoV. In this case, AVA = π cm2 x (1.0 m/sec ÷ 2.5 m/sec) = 3.14 cm2 x (0.4 m/sec) = 1.2 cm2 Question What is the most likely etiology of this patient valve disease? A. Bicuspid. B. Inflammatory process. C. degenerative calcific disease. D. Congenital unicuspid valve. Question What is the most likely etiology of this patient valve disease? A. Bicuspid. B. Inflammatory process. C. degenerative calcific disease. D. Congenital unicuspid valve. Question What is the next step in the management of this patient? A. Dobutamine Echo. B. Medical treatment. C. Medical treatment but repeat study in 6 months. D. R/L heart cath with CO, AV gradient and coronary angio. E. Coronary angiogram and AVR. Answer What is the next step in the management of this patient? A. Dobutamine Echo- only for Low CO pt with EF 65% B. Medical treatment-pt with symptoms, C. Medical treatment but repeat study in 6 months. D. R/L heart cath with CO, AV gradient and coronary angio. Gives you more info E. Coronary angiogram and AVR- AVA 1.2 per echo need more info before AVR Question Cardiac Cath: Aortic pressure 130/70 mmHg. LV pressure 180/15 mmHg. CO via thermo-dilutioon is 3.5 L/min. SEF is 280 ms at HR of 70bpm. Oxygen consumption is 270 cc/min. Pulmonary artery saturation is 64% and femoral artery saturation is 98%. Coronary arteries are normal What is the calculated AVA? A. B. C. D. 0.5 cm2 0.8 cm2 1.0 cm2 1.2 cm2 Answer Cardiac Cath: Aortic pressure 130/70 mmHg. LV pressure 180/15 mmHg. CO via thermo-dilutioon is 3.5 L/min. What is the calculated AVA? A. B. C. D. 0.5 cm2 0.8 cm2 1.0 cm2 1.2 cm2 Use Hakke formula AVA=CO/(p-p gradient) AVA=3.5 /(180-130) 3.5/7= 0.5 cm2 Question What is the next step in the management of this patient? A. Medical therapy B. AVR- homograft C. AVR- mechanical D. AVR - Ross procedure Answer What is the next step in the management of this patient? A. Medical therapy B. AVR- homograft C. AVR- mechanical D. AVR - Ross procedure Less then 65yo without CI Mechanical valve TOC. Question The calculated aortic valve area using LVOT diameter = 2cm, Vmax AV = 4 m/sec, and Vmax LVOT = 0.8 m/sec is: A. 0.6cm². B. 1.0cm². C. 2.0cm². D. 1.2cm². E. 1.5cm². Answer The correct answer is A. The first step is to calculate the cross-sectional area of LVOT, as follows: CSA (LVOT) = π r2 = π(d/2)2. The formula for calculated aortic valve area (AVA) is: AVA (cm2) = CSA (LVOT) x (Vmax LVOT) ÷ Vmax AoV. In this case, AVA = π cm2 x (0.8 m/sec ÷ 4 m/sec) = (3.14)(0.2)= 0.6cm2 Question A 50-year-old man is referred with a murmur of aortic stenosis--an incidental finding on a routine physical examination. The patient denies cardiac symptoms. The physical examination was unremarkable except for a grade IV/ VI late crescendo murmur typical of aortic stenosis and an S4 gallop. The resting ECG showed minimal ST and T changes but no voltage criteria for LVH. The Doppler echocardiogram showed a mean gradient of 60 mmHg with thickening of the ventricular walls but a normal ejection fraction. The patient underwent a Bruce protocol exercise test and quit after 5 minutes because of dyspnea. The thallium image showed no localized defect. Question What is the most appropriate management strategy at this time? A. Follow the patient with echocardiography every 6 months. B. Perform a dobutamine stress echo. C. Start enalapril. D. Follow the patient with an exercise stress test every 6 months. E. Recommend aortic valve replacement. Answer The correct answer is E. This patient has severe aortic stenosis. Although the patient claims to be asymptomatic, his poor performance on the exercise test indicates he is not. In fact, patients with "asymptomatic" aortic stenosis have a 2-4% risk of cardiac death. Usually, however, symptoms develop 1-3 months before death. In view of the low surgical risk and good long-term result of mechanical prosthetic valves, plus the definite incidence of sudden death in symptomatic patients who are not operated upon, the prudent course is to recommend aortic valve replacement. This patient has a low risk of associated coronary artery disease, but this would need to be evaluated by catheterization preoperatively Question Which one of the following is the most reliable measurement of the severity of aortic stenosis in a 75-year-old patient with congestive heart failure, a calcified aortic valve, and an ejection fraction of 25%? A. Aortic valve area at the time of cardiac catheterization. B. Pressure gradient across the valve. C. Angiographic appearance of the valve. D. Dobutamine stress echo Doppler. E. Radionuclide exercise study. Answer The correct answer is D. For reasons that are not totally clear, the Gorlin formula for aortic valve area becomes less reliable in patients with calcific valves and a low ejection fraction and a low cardiac index. Such patients typically have only a modest pressure gradient across the valve. The angiographic appearance of the valve is not reliable for distinguishing between moderate and severe disease when the valves are calcified. Likewise, a radionuclide angiogram would be of limited use in this setting (and the patient probably could not perform it). Recent evidence suggests that a dobutamine echo-Doppler study is a more reliable method of calculating aortic valve severity when the cardiac output is increased by dobutamine. When the aortic stenosis is significant, the gradient will significantly increase. Question Which of the following is least likely to be a determining factor in the operative risk of valvular aortic stenosis? A. An aortic valve area of less than 0.7 cm². B. The presence of coronary artery disease. C. Left ventricular systolic dysfunction. D. The presence of atrial arrhythmias. E. Coexisting aortic regurgitation. Answer The correct answer is A. The valve area defines severity of aortic stenosis, but not the risk of operation. The presence of coronary artery disease increases risk in most studies--up to 2X in some. Failure to bypass significant disease at the time of valve replacement substantially increases risk. Severe LV dysfunction with its associated symptoms and signs of congestive heart failure increases risk, which parallels functional class. Patients in atrial fibrillation have a higher risk of surgery. They are generally later in the natural history of the disease and have other cardiovascular morbidity. Coexisting aortic regurgitation does increase risk in some studies. Question The following hemodynamic data were obtained in patients with isolated valvular aortic stenosis. Which of the following is consistent with severe aortic stenosis? A. Mean gradient across the aortic valve of 23 mmHg with cardiac index of 3.0 l/min/m², and normal left ventricular function. B. Mean gradient across the aortic valve of 28 mmHg, cardiac index of 1.8 l/min/m², left ventricular ejection fraction of 29%; after dobutamine infusion, the aortic valve gradient is 28 mmHg, and the cardiac index is 3.2 l/min/m². C. Mean gradient across the aortic valve of 32 mmHg, cardiac index of 1.5 l/min/m², and LV ejection fraction of 28%; after dobutamine infusion, mean gradient across the aortic valve is 50 mmHg and cardiac index 3.0 l/min/m². D. Mean gradient across the aortic valve of 25 mmHg, cardiac index of 3.5 l/min/m² with an LV ejection fraction of 35%. Answer The correct answer is C. The interpretation of pressure gradients must include an analysis of flow. The difficult clinical question is whether the low gradient, usually in the 20-30 mmHg range, is associated with severe aortic stenosis masked by low flow. The flow may be so low that even in the presence of a severe anatomic narrowing, the gradient is low-thus the need to remeasure the gradient after inducing an increase in flow. In the first example, a mean gradient of 23 mmHg with normal LV function and cardiac index is consistent with mild aortic stenosis. Question A 62-year-old man presents with chest pain typical of angina pectoris, New York Heart Association functional class II. Physical examination reveals a grade III/VI musical systolic ejection murmur at the left sternal border, radiating to the neck. A2 is decreased but present. Echocardiography shows left ventricular hypertrophy, a normal ejection fraction, and a calcified aortic valve with a valve area of 0.8cm2. He undergoes a coronary arteriogram, which shows a diffusely calcified aortic valve with reduced mobility and a pressure gradient of 45mm across the valve. The left ventricle appears normal. There is, however, an 85% diameter stenosis of both the proximal left anterior descending and proximal right coronary artery. Question Which one of the following therapeutic approaches offers the most favorable long-term result for this patient? A. Medical therapy with beta blockers, aspirin, and enalapril and followup every 6 months until the aortic stenosis worsens. B. Coronary artery bypass grafting, including a left internal mammary artery and aortic valve replacement with a bioprosthesis. C. Coronary artery bypass grafting, including an internal mammary artery and aortic valve replacement with a mechanical prosthesis. D. Coronary artery bypass grafting, including an internal mammary artery, but delaying aortic valve replacement until the lesion is more severe. E. Multivessel angioplasty now, following the patient until the aortic valve disease becomes more severe. Answer The correct answer is C. This patient has severe coronary artery disease requiring interventional treatment. He has concurrent, moderately severe aortic stenosis that is nearly bad enough to warrant surgical repair on its own. There would be a high surgical risk to fixing the coronary lesion but not the aortic valve, as there would be also for multivessel angioplasty. He probably is not a candidate for medical therapy, in view of the severity of both his valve and coronary artery disease. Postponing aortic valve surgery and performing bypass only now would expose him to operative mortality in the excessively high 15-25% range. Answer This patient might be expected to live 20 years, in view of his normal left ventricle and the favorable results of internal mammary bypass. Thus, his best outcome would be to have a coronary artery bypass operation and simultaneous aortic valve replacement. Although the combined surgery slightly increases the operative mortality for aortic valve replacement (510%), it is still significantly less than that for a re-do operation to replace the aortic valve sometime after the bypass procedure has been performed. Question An 18-year-old college freshman presents with 3 days of flu-like symptoms and sharp right chest pain with inspiration. Physical examination shows BP 100/70, pulse 88 regular, temp 100F, respiration rate 20. HEENT is negative except for boggy nasal mucosa. JVP is normal. Carotids with slow upstrokes, palpable systolic thrills, and systolic bruits. Normal breath sounds, lungs clear, but he splints inspiration, complaining of pain on inspiration along right costal margin. S1 is normal, S2 with increased A2, ejection click and grade IV/VI systolic ejection murmur upper right sternal border radiating to the neck. No diastolic murmur. Abdomen negative. Extremities with 2+ pulses, no brachial-femoral delay. No edema, cyanosis, clubbing. Question ECG shows increased precordial voltage. Chest x-ray normal. Echo-Doppler study shows a 50 mmHg aortic valve gradient, mobile "doming" leaflets, mild aortic regurgitation, aortic valve area 1.0 cm2, mildly increased LV mass, LV ejection fraction 75%. No pericardial effusion. Question Which one of the following is appropriate next? A. Treat him symptomatically for viral infection, discuss antibiotic prophylaxis, and arrange follow-up visit. B. Refer for aortic valve replacement as soon as possible. C. Treat with penicillin and aspirin and start rheumatic fever prophylaxis. D. Eliminate balloon valvotomy as a therapeutic option due to age and presence of aortic regurgitation. E. Draw blood cultures and initiate IV antibiotics for treatment of endocarditis. Answer The correct answer is A. Because the patient has viral pleurisy and an exam consistent with moderate aortic stenosis, likely congenital, prophylaxis and regular follow up are important. Referring for aortic valve replacement is inappropriate because aortic stenosis is moderate and asymptomatic, so follow-up is appropriate. You could consider a valvotomy, as gradient is 50mm and he has LVH, but not valve replacement. There are insufficient criteria for rheumatic fever and the echo findings are classic for congenital AS. Although he could have a valvotomy, he has a mobile, bicuspid valve with mild and inaudible aortic regurgitation and no contraindications. Making a distinction between whether he is an adolescent, reaching pediatric criteria for intervention, or an adult is of no consequence in this instance. Blood cultures and IV antibiotics are not called for because viral syndrome is likely. He should instead be instructed to monitor fever, report if high and chills, and be given no antibiotics. Blood cultures could be drawn, but likely will be negative. Question A 77-year-old man with chronic angina pectoris of 3 years duration has had increasing symptoms for the past 6 weeks with episodes at rest, nocturnal episodes, and prolonged episodes with effort often requiring two to three sublingual nitroglycerins (instead of the usual one or rest) for relief. His overall health is good. He is known to have aortic stenosis of moderate degree with typical findings. His blood pressure is 140/80, heart rate of 72, his carotid pulses show delayed upstroke. There is no jugular venous hypertension or basal thrill. The apical impulse is localized but enlarged and forceful. There is no aortic second sound and a typical musical murmur of calcific aortic stenosis. Question His electrocardiogram shows moderate voltage for LVH, flattening of the T waves, and left atrial abnormality and no suggestion of myocardial infarction. An angiographic study showed major narrowings in the proximal portions of all three of his coronary trunks, diffuse disease throughout the arteries but good distal vessels. There is moderate narrowing in the LMCA. A pullback mean gradient was 30 mmHg. The valve is heavily calcified. The ejection fraction was estimated at 55-60% Question Which of these management strategies is preferred? A. CABG without aortic valve replacement. B. Increase medical therapy adding a beta blocker. C. Perform a thallium test to localize ischemia, and perform intentionally incomplete revascularization utilizing PCI. D. Dobutamine stress test to study ischemia and evaluate the gradient during stress. E. CABG with aortic valve replacement. Answer The correct answer is E. This problem of senile calcific aortic stenosis with major coronary atherosclerosis is a vexing problem occurring with increasing frequency in the elderly population. The issue here is to predict the progression of his aortic stenosis. Although a spectrum of opinions exist, in centers with excellent cardiac surgery, option E, CABG with valve replacement, is preferred. Although the combination surgery modestly increases risk, the chance of a need for valve replacement during the next 3-5 years is quite high, so isolated CABG is problematic in reference to a "long term solution" to this elderly man’s problem. Though data are sparse and fragmentary, particularly in elderly patients, data indicate aortic stenosis of moderate severity, particularly with heavy calcification, is likely to become symptomatic and require valve replacement within 5 years. Avoiding an emergency operation is important, and the risk of two open-heart surgical procedures in patients over the age of 75 during a 3-5 year period is significantly more risky than doing a single procedure. Answer Although a PCI procedure in the elderly is appealing (C), the extent of disease in this patient coupled with his diabetes makes PCI problematic. However, if PCI were successful in relieving his angina, it would provide relief for several years during which the aortic stenosis could progress. There is no advantage and perhaps some minimal risk in dobutamine echo-cardiographic study (D) in this patient. Although its role in assessing aortic stenosis remains uncertain, its chief value is in patients who have a low gradient (such as this patient) but with reduced ventricular function (which is not the case in this patient) in an effort to differentiate the effects of afterload increase from reduced contractility on the ventricular dysfunction. Medical therapy (B) is extremely unlikely to be useful in this patient, with worsening of angina considering his age, AS, and overall duration of his complaint. Question All of the following are echocardiographic evidence for aortic stenosis except: A. Concentric LVH. B. Markedly thickened and restricted aortic valve leaflets. C. TVI LVOT/TVI AV < 0.25. D. V (max) AV > 4.5m/sec. E. TVI (AV)/TVI (LVOT) < 0.25. Answer The correct answer is E. The dimensionless index is TVI LVOT/TVI AV. If this is < 0.25, then a patient has severe aortic stenosis. Patients with significant aortic stenosis have LVH as a response to the increased workload on the LV. Patients with aortic stenosis have markedly thickened and restricted aortic leaflets unless they have an unusual form of congenital aortic stenosis, such as a unicuspid aortic valve. A Vmax > 4.5m/sec across the aortic valve would correspond to a peak pressure gradient of 81 mmHg, which would be consistent with severe aortic stenosis. Question You are responsible for the care of a vigorous 72-year-old man with acquired degenerative calcific valvular aortic stenosis, accompanied by mitral regurgitation and calcification of the mitral annulus. He has survived infective endocarditis with multiple positive cultures for Streptococcus mutans, which you judged to be of dental origin although there had been no specific dental intervention related temporally with the onset of symptoms. Based on catheterization data completed during his antibiotic course, you feel that aortic valve replacement and inspection of the mitral valve and adjacent structures are indicated. The patient has 11 remaining teeth that are in poor repair. Question Which one of the following is the best plan? A. Ignore the dental status in deference to the more serious valvular heart disease. B. Discharge the patient to the care of his dentist to permit cautious dental extraction of one to two teeth per visit. C. Schedule full-mouth extraction well in advance of the anticipated cardiac surgery. D. Schedule full-mouth extraction synchronous with cardiac surgery, thus avoiding a second anesthesia. E. Delay all dental procedures until after the cardiac surgery. Answer The correct answer is C. This patient's dental hygiene probably is the source of his endocarditis, demonstrating that a dental procedure is indeed not required for endocarditis to occur. In terms of his ongoing risk for recurrent endocarditis, proper management of his dentistry preoperatively is perhaps the most important factor. Once his prosthetic valve is implanted, he is then forever maximally at "high risk" such that any issues that can be addressed safely and reasonably before cardiac surgery should be done. Removal of all his teeth at once is a procedure that dental surgeons can accomplish with little difficulty, thereby undertaking the risk of extraction-related bacteremia once rather that several times. The serial approach, in addition to being unnecessary, would raise the additional issue of cumulative antibiotic resistance via the chemoprophylaxis regimens, which would need to be given for each of the procedures. Answer Performing this procedure in conjunction with the cardiac surgery (in any sequence) would simply add unnecessary stress (as well as bacteremia) to a time that is already high-risk in and of itself. Delaying the dentistry would simply make likely the occurrence of prosthetic valve endocarditis (PVE) via the same mechanisms responsible for the original infectious illness. Careful preoperative dental evaluation is recommended so that required dental treatment can be completed at least several weeks prior to cardiac surgery whenever possible. Such measures may decrease the incidence of late postoperative endocarditis. Question Catheter-delivered balloon expansion techniques are now the treatment of choice for which one of the following lesions in adults? A. Valvular pulmonic stenosis. B. Valvular aortic stenosis. C. Coarctation of the aorta. D. Ebstein's anomaly of the tricuspid valve. E. Severe mitral stenosis/regurgitation. Answer The correct answer is A. Although catheter balloon valvuloplasty and aortoplasty have been attempted in all these conditions, only pulmonary valvotomy has achieved a success level consistent with being the treatment of choice in adults. Aortic stenosis responds initially to balloon expansion and may serve as a bridge to valve replacement surgery, but is associated with rapid restenosis. Success rates with coarctation and Ebstein's anomaly are not uniform enough to displace surgery except in selected patients. Mitral stenosis in the absence of severe subvalvular disease can be successfully treated by balloon valvuloplasty, but the presence of moderate to severe regurgitation is an indication for surgery. Work Cited Mayo Board Review ACCSAP V Up-To-Date ACC/AHA Guidelines The End