It’s Leaky... MITRAL REGURGITATION Rami Khouzam, MD

It’s Leaky...
MITRAL REGURGITATION
Rami Khouzam, MD
Mitral Regurgitation
• Anatomy:
3 basic mechanisms of MR:
1- Alteration of Mitral leaflets, commissures, or annulus
2- Defective tensor apparatus
3- Alterations of LV and LA size & function
1- Alteration of Mitral leaflets, commissures, or annulus:
• MVP: most common cause of isolated MR.
Posterior leaflet more frequent and severe.
Greater in men. Increases with age.
• Rheumatic fever
• Mitral annulus calcification: age-related
• Infective endocarditis
• Congenital: cleft of anterior MV associated with primum ASD
2- Defective tensor apparatus:
• Abnormal chordae tendineae: Idiopathic/ endocarditis/ MVP/ Trauma
• Papillary muscle dysfunction:
Posteromedial > anterolateral (vulnerability to ischemia & infarction): single blood supply
3- Alterations of LV and LA size & function:
• Alteration of position and axis of papillary muscle
• Mitral ring dilatation
Key points...
• Mitral prolapse is the most common cause of isolated MR
• Ischemia:
dysfunction/rupture of papillary muscle. Posteromedial > anterolateral
• LV enlargement & abnormal contractile function are common causes of MR
Pathophysiology of MR
1. Acute Stage
2. Chronic Compensated Stage
3. Chronic Decompensated Stage
Key points...
• Acute severe MR is characterized by normalsized chambers, high EF, & pulmonary congestion.
• Chronic compensated severe MR is typified by few symptoms, enlargement of the LV &
LA, and high EF
• Chronic decompensated severe MR is typified by enlargement of the LV & LA, pulmonary congestion, and normal to low EF
• A “normal range” EF in the setting of severe
MR usually implies LV systolic dysfunction
Clinical syndrome of MR
Acute MR
• If severe: pulmonary congestion
• S3 S4
• Systolic murmur: short, soft or absent
Chronic MR
Prolonged asymptomatic interval.
Fatigue/ generalized weakness
Laterally displaced, enlarged apical impulse
Severe MR: apical thrill
Early aortic closure
Holosystolic murmur: intensity does not correlate with severity of regurgitant flow
Anterior leaflet MR: Radiates to axilla frequently
Posterior leaflet abnormality:
regurgitant flow anteriorly
radiation to aortic area, and all precordium
Short diastolic apical rumble in the absence of MS: high diastolic transmitral flow & severe MR
Key points...
• Acute severe MR: short or soft murmur because of low LV-LA pressure gradient
• Nonspecific fatigue & weakness may represent early symptoms of chronic severe MR
• Duration of apical impulse in chronic severe MR is related to LV systolic function
• Posterior leaflet prolapse: murmur to aortic area
• Amyl nitrite distinguishes diastolic rumble of mixed MS & MR (
) from that due to isolated severe MR (
)
Evaluation of MR
LAE
Atrial fibrillation
LVH
Nonspecific ST-T changes
EKG
CXR
LVE
LAE (straightening left border, atrial double density, elevation of left main-stem bronchus)
Pulmonary venous congestion
Echocardiography
In some cases, TEE is better to assess the anatomy of the MV, to rule out atrial thrombus, gather supplemental data in quantitative & qualitative measures of regurgitation severity (but not always necessary).
Determination of severity
Over 20 variables described.
Color flow Doppler
Atrial side:
Small jet occupying < 20 % of LA: mild
20- 40 %: moderate
Large jet > 40 % and extending into the pulmonary veins): severe
Ventricular side: PISA proximal flow acceleration (proximal isovelocity surface area): concentric series of hemispheric rings of alternating colors, each ring denoting an isovelocity of aliasing.
The diameter of the ring closest to the regurgitant orifice is measured and, in severe mitral regurgitation, usually approaches
1 cm .
Pulsed and continuous wave Doppler of mitral inflow
E > 1.4 m/sec
E/A ratio > 2
(Finding an A-wave dominant pattern of mitral inflow makes severe mitral regurgitation very unlikely).
Uniformly dense jet throughout its duration, well-defined envelope
TR peak velocity: pulmonary hypertension.
Doppler of pulmonary veins: show systolic flow reversal
Doppler of pulmonary veins
(pulse Doppler of the left and right upper pulmonary veins from the apical four-chamber view). Normal pulmonary venous flow is antegrade during both ventricular systole and diastole (ventricular systolic component dominates), with slight retrograde flow during atrial systole. In hemodynamically severe mitral regurgitation, the flow in one or more pulmonary veins
(depending upon the direction of the jet) will show systolic flow reversal
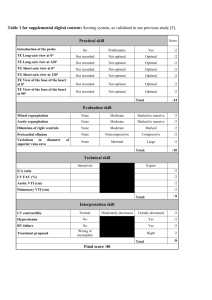
Index of severity
Based on 6 variables, each scored on a scale of 0 to 3 then averaged
1Color Doppler regurgitant jet width and penetration
2Color Doppler PISA diameter
3Continuous wave Doppler characteristics of the regurgitant jet
4Continuous wave Doppler TR derived PAP
5Pulse wave Doppler pulmonary venous flow pattern
6- Left atrial size by 2D- echocardiography
(Mild MR: index 1.7, Severe MR (regurgitant fraction >40 percent) : index 1.8
, A value 2.2
identified patients with severe mitral regurgitation with a sensitivity, specificity, and positive predictive value of 90, 88, and 79 percent, respectively).
Cardiac catheterization
Right heart cath:
Prominent “V” wave on
PCWP tracing
Left heart cath/ Ventriculogram: Only when
- noninvasive data are discordant or
- technically limited or
- differ from the clinical perception of the severity of MR or ventricular function.
Angiographic grading: many variables..
Sellars criteria
Key points...
• No EKG or CXR findings pathognomonic of MR
• Echo is invaluable for assessing cause & severity of MR, size and function of LV, LA,
RV
• Left ventriculography is most useful when noninvasive data discordant or technically limited or differ from clinical impression of the severity of MR, or ventricular function
Mitral valve prolapse
• Click: systolic billowing of a portion of mitral leaflet into LA
• Maneuvers that ventricular preload (Valsalva, standing): prolapse, click & murmur earlier in cardiac cycle.
• Progression to severe MR: more in men, and advancing age
• MVP & severe MR: managed as severe MR
• Antibiotic prophylaxis: when?
- Click & murmur, or
- Click & echo: significant leaflet thickening or regurgitation
• B-Blocker: for MVP/palpitations/atypical CP/anxiety
• ASA:
TIA in the setting of MVP
Natural history of MR
• Depends on its cause
• Time course of progressive LV dysfunction in chronic MR is variable & unpredictable
• Acute worsening of MR suggests chordal rupture, infection, new arrhythmia, or ischemia
Outcome after surgical correction of MR
(The unnatural history)
• Current surgical practice is to operate on patients with severe MR before the development of heart failure or ventricular dysfunction, if possible
• Preoperative EF: best predictor of long-term mortality,
CHF, & postoperative LV function
• End-systolic dimension: significant predictor
• A. fib more than 3 months preoperatively associated with high risk of postoperative arrhythmia persistence and need for long-term anticoagulation
Treatment of Acute severe MR
• i.v. vasodilators (Na nitroprusside), i.v. inotropes, IABP
• Mitral valve Repair or Replacement
• Endocarditis: delay surgery if possible (risk of recurrence), unless progressive heart failure, unresponsive to antibiotics, intracardiac abscess, recurrent systemic embolization
Treatment of Chronic Nonischemic MR
• Dental hygiene/ Antibiotic prophylaxis
• Treat contributing underlying disease
• No data to indicate diuretics or vasodilators
(or both) provide morbidity or mortality benefit
• Every patient should be considered for surgery
Indications for surgery for chronic mitral regurgitation
SYMPTOMS LV EF LVESD
NYHA II - IV > 60 % < 45 mm
Asymptomatic or symptomatic 50 - 60 % = 45 mm
Asymptomatic or symptomatic < 50 % or = 45 mm
Pulmonary artery systolic pressure = 50 mmHg
MV REPAIR
Who gets it??
• Repair should be performed preferentially whenever possible : favorable predictor of operative mortality, late survival, postoperative EF.
• High risk patients: severe LV dysfunction (EF < 35 %,
CI < 1.5 L/min per m2)
• MR: posterior leaflet, non-rheumatic, noninfective, noncalcific, nonischemic: most amenable to repair
Treatment of MR d.t. Ischemia or
Cardiomyopathy
• Maximal medical therapy: FIRST
• MVR (Mitral annular rings)
Key points...
• Patients with acute severe MR & hemodynamic instability require rapid evaluation, aggressive stabilization, & early valve operation
• Patients with acute severe MR & hemodynamic stability: semielective surgery
• Indications for valve surgery in endocarditis: progressive heart failure, resistance to antibiotics, intracardiac abscess, recurrent systemic embolization despite therapy
• Severe chronic MR & NYHA class III or IV, EF < 60 %,
End-systolic diameter > 45 mm, or end-systolic volume > 50 mL/m2: Definite Surgery
Key points...
• Emerging indications for MV Replacement:
Flail leaflet, paroxysmal or recent A. Fib, pulmonary HTN
• Impaired LV function: Valve repair preferred
• NO Repair in: rheumatic, ischemic, endocarditis, anterior or bileaflet prolapse, significant calcification
QUESTIONS
Question 20 of 264
Which one of the following statements about mitral valve prolapse is incorrect?
A. The degree of echocardiographic thickening of the mitral valve is related to long-term prognosis.
B. Clinical auscultatory phenomena as well as echocardiographic documentation should be present for the diagnosis of mitral valve prolapse.
C. Most symptoms in patients with the mitral valve prolapse syndrome are related to the severity of mitral regurgitation.
D. Echocardiographic mitral valve prolapse may be seen in normal individuals after volume depletion.
The correct answer is C.
Several clinical and autopsy studies have demonstrated that patients with mitral valve prolapse and thick mitral valve leaflets are at high risk for the development of complications. The diagnosis of mitral valve prolapse as a general rule should be based on auscultatory and confirmatory echocardiographic findings, and not on "soft" echocardiographic or nonspecific auscultatory findings.
Echocardiographic mitral valve prolapse may be seen in normal individuals after volume depletion or a decrease in intravascular volume. Symptoms in patients with mitral valve prolapse may be directly related to the severity of regurgitation. Certain patients with mitral valve prolapse, however, may have symptoms related to autonomic dysfunction (mitral valve prolapse syndrome). For the diagnosis of mitral valve prolapse syndrome, mitral valve prolapse should be present.
A 55-year-old African-American man is referred to you for evaluation of a murmur. The murmur was first noted five years ago. He denies any symptoms, but admits that he has always done little physical activity. He states that he no longer walks to the office, and does not have to walk stairs to the third floor because there is an elevator. Family history: Both his
78-year-old father and his 48-year-old brother have heart murmurs, but are doing well.
Physical examination: BP 110/70 mm Hg, pulse 80/minute, respirations 15/minute. Neck veins 5 cm. Carotid upstroke is normal without bruits. Lungs are clear to auscultation and percussion. Point of maximal impulse is diffuse in the 5th intercostal space in the midclavicular line and forceful. First and second heart sounds are normal. There is a grade
III/VI systolic murmur crescendo to the second sound, best heard at the apex, but radiating well to the base. There are no S
4 or S
3 gallops and no other abnormalities.
Laboratory: Chest X-ray: Prominent LV, normal lung fields. ECG: LV hypertrophy by voltage, no ST-T wave changes. Valve 2D echo-Doppler: Floppy mitral valve, severe posterior leaflet prolapse, moderately severe mitral regurgitation (MR) with the jet directed anterior-medially. LV end-diastolic diameter is 5.8 cm and LA diameter 4.5 cm. His EF is estimated at 45-50%.
What is the most appropriate recommendation for treatment for this patient?
A. Follow medically with close observation and repeat echo if there is a clinical change.
B. Start enalapril and repeat echo in four months.
C. Send to surgery for mitral valve replacement.
D. Send to surgery for mitral valve repair.
E. Start long-acting nifedipine and repeat echo in one year.
The correct answer is D.
This man has MR and has the best pathology for successful mitral valve repair. To require mitral replacement would be very unusual with posterior leaflet prolapse and would be a harder decision to make in this man who claims to be asymptomatic, if it were necessary. Both options B and E are incorrect because this man has an EF at the lower limits of normal or mildly decreased, indicating a decreased myocardial contractility in the presence of moderately severe MR.
Question 51 of 264
A 36-year-old woman presents with sudden severe dyspnea. She had mitral valve replacement five years ago with a St. Jude valve and ran out of warfarin two weeks ago. Physical examination shows signs of pulmonary edema and right heart failure. She is afebrile, BP is 130/86, and pulse is 95 with sinus rhythm. TEE shows a large mass impairing the mobility of one of the bileaflets.
The best initial management strategy would be which one of the following?
A. Immediate valve replacement.
B. High-dose IV antibiotics.
C. A loading dose of heparin.
D. IV thrombolytic therapy.
E. IV enalapril.
The correct answer is D.
Acute valve thrombosis is a catastrophic complication of prosthetic valve replacement and is almost always a result of inadequate chronic anticoagulation. Because of the rarity of this problem (0.2% per patient-year), there is not a great deal of experience with any form of management. When clinical suspicion is high, cinefluoroscopy or TEE should be done to confirm the diagnosis. If thrombus is believed to be present and the patient is hemodynamically stable, thrombolytic therapy should be tried first followed by heparin, provided there are no contraindications to this approach. If there are contraindications to thrombolytics but not heparin, the latter can be tried first. If there is no improvement in 48-72 hours or if the patient decompensates, surgery is indicated.
Question 101 of 264
In which of the following diseases is pregnancy difficult, but not highly risky to the mother and fetus?
A. Eisenmenger's syndrome.
B. Primary pulmonary hypertension.
C. Mitral prolapse with significant mitral regurgitation.
D. Prior peripartum cardiomyopathy with heart failure.
E. The Marfan syndrome with dilated aortic root.
The correct answer is C.
The CV system must be able to handle a doubling of cardiac output during pregnancy. Thus, cardiopulmonary diseases that obstruct blood flow are usually contraindications to pregnancy because both the mother and fetus get inadequate blood flow. Thus, obstruction to pulmonary flow due to the
Eisenmenger reaction or primary pulmonary hypertension fits into this category, but hypertrophic cardiomyopathy does not. The increased cardiac output increases venous return to the left heart, resulting in LV enlargement and less obstruction. In fact, during pregnancy, the murmur of hypertrophic obstructive cardiomyopathy may lessen or even disappear, causing the diagnosis to be missed.
Prior peripartum cardiomyopathy with heart failure is a contraindication to pregnancy because of the high incidence of recurrent failure and death.
Hormonal changes during pregnancy alter vascular walls, making them more distensible. This is a normal mechanism to adapt to higher cardiac output; however, in the patient with the Marfan syndrome and an enlarged aortic root, it can lead to increased wall stress and aortic rupture or dissection.
Question 153 of 264
A 52-year-old woman goes into acute pulmonary edema after an auto accident. She has a mild concussion and bruises on her upper body. ECG shows sinus tachycardia and nonspecific ST-T wave changes. Physical exam shows BP 123/72, pulse 110 regular, diffuse pulmonary rales, a grade 2 early systolic murmur, and a third heart sound.
What is the most likely diagnosis?
A. Ruptured papillary muscle.
B. AMI.
C. Cardiac contusion.
D. Noncardiogenic pulmonary edema.
E. Pulmonary contusion.
The correct answer is A.
Cardiac problems discovered following an auto accident raise the question of whether the cardiac condition caused the accident or vice versa. In this case, there is no cardiac history preceding or during the accident, but only later. The ECG is not suggestive of AMI, but it cannot be eliminated based on the information given. The physical examination is consistent with
CHF (i.e., rales and third heart sound), and myocardial contusion or ruptured papillary muscle could lead to pulmonary edema. The early systolic murmur is characteristic of severe acute mitral regurgitation due to papillary muscle rupture since the resultant severe regurgitation rapidly eliminates the gradient between the LV and atrium during systole, shortening what would ordinarily be a holosystolic murmur. Thus, the best answer is ruptured papillary muscle.
Question 163 of 264
A referring physician treating a patient with an inferior wall MI calls you. The patient received thrombolytic therapy and seemed to be stabilizing nicely. On the third day after the infarction, the patient became acutely short of breath and is now in pulmonary edema with a BP of 80 mm Hg systolic. On examination, the jugular venous pressure is normal and auscultation of the heart reveals no murmur or gallop. The ECG is unchanged.
The correct diagnosis in this case is:
A. Ruptured ventricular septum.
B. Papillary muscle rupture with severe mitral regurgitation.
C. Massive pulmonary embolism.
D. Infarct extension.
E. RV infarction.
The correct answer is B.
This is a typical presentation of a patient with inferior wall
MI and rupture of a papillary muscle several days after the initial event. This complication can be treated with great success if recognized and surgery to replace/repair the valve is accomplished without delay. The lack of a murmur is not unusual and probably relates to prompt equilibration of LV and LA pressures. Involvement of the posterior papillary muscle is more common as a result of a more common single artery supplying this structure. Infarct extension is unlikely in view of the unchanged ECG. An
RV infarction is unlikely in view of the normal jugular venous pressure.
A 68-year-old Caucasian male has been a patient of yours for 10 years. He has had insulin-treated diabetes mellitus for 14 years, known CAD with an MI 12 years ago, and
CABG 12 years ago. He follows his regimen of diet and exercises moderately, including playing golf. In the past six months he has noted new bilateral ankle edema toward the end of the day, as well as mild dyspnea on exertion. He denies chest discomfort. His medications have been furosemide 40 mg daily, atorvastatin 40 mg daily, metoprolol
6.25 mg bid, isosorbide mononitrate 60 mg daily, ezetimibe 10 mg daily, aspirin 325 mg daily, losartan/hydrochlorothiazide combination 100 mg/25 mg daily, dixogin 0.125 mg qd, and rosiglitazone metformin combination 2/500 mg daily.
Laboratory work has shown total cholesterol 177 mg/dl, LDL cholesterol 77 mg/dl,
HDL cholesterol 48 mg/dl, and triglyceride 92 mg/dl. Renal, hepatic, and hematologic functions were normal. Two-hour postprandial glucose was 134 mg/dl.
His ECG shows an old anterior MI and left anterior hemiblock; an echocardiogram shows an LVEF of 0.38. The LA is mildly enlarged. There is moderate mitral regurgitation. You should, as your first strategy:
A. Refer for mitral valve surgery.
B. Refer for biventricular pacing.
C. Increase his furosemide to 80 mg daily.
D. Begin spironolactone 25 mg daily.
E. Increase his losartan to 200 mg daily.
The correct answer is D.
The therapeutic issue is deciding what is maximum medical therapy in this man with left- and now right-sided heart failure. There is little to be gained by doubling his dose of losartan. While you may need to increase his furosemide for comfort due to fluid retention, the best first step is to add spironolactone, which should not only affect diuresis, but contribute to improvement in LV systolic performance through its renin-angiotensin effects. The device interventions may be considered after maximum medical therapy has been achieved in reference to both the number and dosage of the drugs. Mitral valve surgery is possible in many patients with advanced failure, but in this case, the degree of mitral regurgitation may lessen considerably with optimal medical therapy, and additional evaluation including catheterization is needed to make the decision if severe mitral regurgitation persists. He does not currently meet accepted indications for ICD placement with his EF above 35%.
Question 197 of 264
Which one of the following conditions is not considered a contraindication to pregnancy?
A. Eisenmenger's syndrome.
B. Moderate primary pulmonary hypertension.
C. The Marfan syndrome with aortic root dilatation.
D. Moderately severe mitral regurgitation.
The correct answer is D.
The risk of pregnancy to the patient with pulmonary hypertension is so great that pregnancy is not considered an option. Similarly, the risk of aortic dissection is quite high in those patients with the Marfan syndrome and aortic root dilatation, so that pregnancy is contraindicated. So long as LV function is normal, patients with mitral regurgitation tolerate the hypervolemia of pregnancy.
Question 116 of 264
A 30-year-old black woman suddenly develops severe tachypnea and tachycardia two days after open reduction of a comminuted fracture of the right femur. You are called to see her in the recovery room. Physical exam: BP is 85/40 mm Hg. Pulse is
120/minute and irregular. Respiratory rate is 28/minute. Neck veins are 15 cm.
Lungs: No rales. Cardiac: Left anterior precordial lift. S
2 widely split. A grade II/VI short systolic ejection murmur is heard loudest at the third intercostal space left sternal border. There is an S
3 that increases with inspiration. Liver is palpable 35 cm below the right costal margin. No pedal edema. Lab: Chest X-ray: Decreased vascular markings in the right lower lobe and left upper lobe. Small pleural effusion right costophrenic angle. ECG: Right axis deviation, RBBB, AF. Echo Doppler; dilated poorly contracting RV. Dilated RA. Normal size LA and LV.
The Doppler jet of tricuspid regurgitation is most likely to be:
A. 1 m/sec.
B. 2 m/sec.
C. 3 m/sec.
D. 4 m/sec.
E. 5 m/sec.
The correct answer is C.
The case is that of a patient with a fracture who develops the classical picture of acute massive pulmonary embolism. Such a patient with extreme increase in RV afterload has no opportunity to hypertrophy to compensate, dilates the RV, then fails. Such a ventricle cannot generate systolic pressures much above 50 mm Hg. The tricuspid jet by the modified Bernoulli equation:
P (m Hg) + 4x [Vcm/sec] 2
Where P = the pressure drop across the tricuspid value
And V = the maximum jet velocity that can be used to estimate the pulmonary artery systolic pressure
P + maximal RA pressure reflected by the jugular venous pressure = estimated RV systolic pressure, which in the absence of pulmonic infundibular and/or valvular stenosis equals the systolic pressure of the pulmonary artery.
Question 142 of 264
Abnormal septal motion can be seen in patients with each of the following except:
A. CABG, postop.
B. A pacemaker.
C. LBBB.
D. Severe mitral regurgitation.
E. Constrictive pericarditis.
The correct answer is D.
Abnormal septal motion can be seen in CABG patients or valve patients and is considered a "postop" septum. In addition, the septum has abnormal motion when it is electrically activated in an unusual fashion, as would be the case for a patient with an LBBB or a pacemaker (when the septum is activated right to left). Also, patients with constrictive pericarditis typically have an abnormal septal bounce. Patients with severe mitral regurgitation do not have abnormal septal motion unless they have one of the previously listed conditions (or severe pulmonary hypertension or right-sided volume overload as well) in addition to their mitral regurgitation.
Formulas for evaluation of MR
• RV = PISA x Velocity
(PISA determined as the aliasing velocity)
• PISA = 2 r2
• RV = ROA x VTI
• ROA = RV/VTI
[RV: Regurgitant Volume, PISA: Proximal
Isovelocity Surface Area, ROA: Regurgitant Orifice
Area or ERA: Effective Reugurgitant Area, VTI:
Velocity Time Integral]