AACN Task Force Focus Groups on Academic-Practice Partnership with members... (Association of State and Territorial Directors of Nursing) May 3, 2011
advertisement

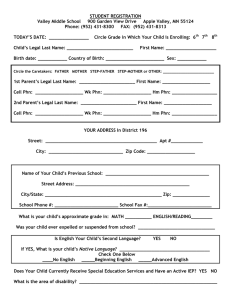
AACN Task Force Focus Groups on Academic-Practice Partnership with members of ASTDN (Association of State and Territorial Directors of Nursing) May 3, 2011 Facilitator: Susan Swider, PhD, APHN-BC Recorder: Pamela Levin, PhD, APHN-BC Participants: state and local Health Departments; Directors of Nursing and supervisory staff States: CA, OH, GA, CT, MA, Del (N=6) All have had some experience with partnerships with local schools Characteristics that facilitate current A-P partnerships MOU with each nursing program in state & some surrounding states; establishing MOU right away Identify nurse consultant or particular nurse in county that works on arrangements (still issue need to work out) Desire between Health Department and school to get something off ground Communicating clearly to Health Department what they would need to provide to support students, tried to minimize effect on daily operations; aim to be a win for both parties Have established relationships at state and regional levels, Longstanding relationships: work together on common issues, position statement around immunizations for pre licensure student, why students need that type training, education for non BSN w/out pop assessment course, arrange for new employees to take that same course at Univ [at Health Dept. level, arrange to pay for that course, work out waiver process] practice and education chairs – designated people (volunteer 2 years, 1 seasoned, 1 new] Dedication of staff, desire to do as much as possible Having champions in place for students. Educating academia as what is available for students (program, opportunities) at state, local level. Building relationships important to work through issues State board of nursing requires certificate and 90 clinical hours in PHN in order practice in PHN. Some PHN supervisors arranged furlough time and were hired by Univ as ‘instructors’. Instructors are onsite, certified, trained and there to work w students. Contracts/formal agreements with university Community advisory board – meet with ADN, BSN programs to discuss issues about student nurses, issues within practice setting… try to resolve.. like how to deal with EHR Helpful to have course objectives right up front to see if they can be met in setting Assigning someone to serve as a liaison…. Having a nursing faculty on site…. If on site, then can make a home visit with student, helps with site workload Recognition for preceptor…. It encourages the nurse to take a student from that school again Barriers in current A-P partnerships Student schedules: Matching a project to students academic year schedule… graduate or RNBSN students working and want to do weekend hours, but not feasible Lack of Standard curriculum…. Set of student activities, What I can keep them busy with in my location Schools contacting individually at local level (Home Rule issue)– takes a lot of time/energy when no liaison type person available Regional level – academic & practice is not reciprocal; the MOU, practice is not getting as much back as giving…. We ask that Schools of nursing provide some CE, some staff training… Lack of Communication from educational system (because of home rule at times) getting requests from online programs … have to create multiple MOU… would be helpful if sent students in cohorts Faculty teaching content with no background, no knowledge in Public Health… don’t get it “I have to spend a day in a Health Department” requests from individual students. Sites don’t have the time to do this; lots of calls; Have to get something back when working with students… I can’t show anything for use of time in our current business model Cost… critical need in getting something back. Asking university for reimbursement for time spent…. For liaison who interacts with students – on regional level, it is a fulltime job – and at expensive pay level. Payment to help sustain… have had one county being successful at getting reimbursement from university… Health Departments are developing their business model and need to see some return on investment School needs to plan what the student is to do… more direction from school…. But then many faculty don’t have Public Health background, don’t know what to plan for.; ‘dumbing down of graduate program in community/phn’ nursing exists; Faculty don’t know the content; An example given of an MSN project that was really at the BSN level, not at the master’s level. Schools don’t understand local government, understand parameters at local level government that may affect what can do as PHN Alternative, web based programs… do not provide instructor on site…. RN-BSN programs do this Ways to overcome barriers Using local/state association to help with student placement Joint meetings annually with academic deans, Health Department leaders Something back from spending time w student Reciprocity agreement in the MOU… may take a while to get it signed, Have faculty on site!!! When on site, can go out in pairs, with something more than observation experiences Faculty with knowledge and skills at BSN & MSN level in PH… so can collaborate with PHN unit to work on project independently Dream/Ideal Partnerships Characteristics Staff nurses /preceptors need access to what the students get exposed to; the up to date info, on a variety of topics. Get staff Link to a library system !!!!!!!!!!!!!; access to the (expensive) databases Access to grant writers Summits – with academia and practice in attendance to strategize Work with them on the curriculum, to identify what is needed and …. Input into curriculum Having conversations about real world and how gets applied to students work… ongoing, as PHN world has changed Has to get something out of it…. Graduate students have to try to do something… not just observational Standardized, free preceptor training (have access through MI, but can’t pay for everyone, $25). Something available for all field preceptors… additional bonus pay so can reward those who take on the extra burden. hospitals get bonuses Staff development… faculty with some type of joint practice, work with on research.. don’t know how to read research, need access to researchers, as how to read, access to research… need to help get published… need to get our name out there….. we need to let public see us making a differences in outcomes… faculty in practice will keep them up to date and help Health Department with research Match up grad students to carry out project… match up grad student with PHN to do research For decentralized states, have been trying to get advisory board with local Schools of Nursing Boards of nursing requiring certification for PHN… make BSN requirement to practice in PH Joint practice – what Jeanne Mathews had done in Virginia. Minimally adequate = MOU has to have instructor on site Appreciate our limitations; may not need an instructor on site, but can only take a few students Appreciation – show it – appreciate our strengths State PHN association, needs to more involved in this Making sure understanding partnership is two way Having ongoing discussions like at ACHNE/ASTDN – great joint meeting time