Hormonal Regulation of Growth
advertisement

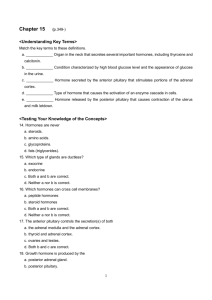
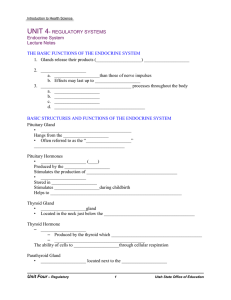
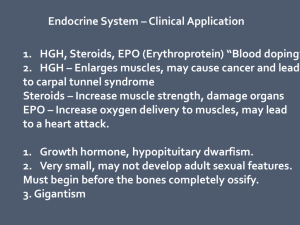
Hormonal Regulation of Growth Hormonal Actions Definition Chemical messengers secreted by various tissues, not necessarily secreted by ductless glands. Hormones act in an endocrine manner when secreted by cells and then transmitted via the bloodstream to act on distant target cells Types of action Neurocrine Hormone is synthesized in a cell body of a neuron and stored in axons such as neurotransmmitters, but secreted into the bloodstream to act on distant target cells A key regulator of animal growth and development by the hypothalamicpituitary-peripheral gland axes Types of action (cont.) Local conveyance – site action Paracrine- when a hormone from one cell is conveyed to an adjacent cell of different type over a short distance via interstitual fluid Autocrine – where a hormone from one cell acts on itself or a neighboring cell of the same type Intracrine – acts intracellularly and does not require secretion to alter the process Types of action (cont.) Tissue specificity Allows hormones to act on target tissues without affecting other tissues or organs Receptors – has an affinity for specific hormones that may be located at the cell Hormones will bind and act through various enzyme systems, ion transport or gene regulation Negative feedback loops may also regulate hormonal function Chemical Nature of Hormones Classification Peptides/amino acid derivatives Water soluble Ex. Thyroxine, LH, FSH Steroid/cholesterol derivatives Ex. Estrogen, testosterone, progesterone Fat soluble Hypothalamic-Pituitary-Peripheral Gland Axis Hypothalamus – the central organ of the neuroendrocrine system Secretions from the Hypoth. Regulate the secretions from the pituitary Located at the base of the brain Two sections: adenohypophysis and neurohypophysis Pituitary Adenohypophysis Pars tuberalis, pars intermedia, and pars distalis (anterior = distalis) Neurohypophysis – Pars nervosa and pars eminens (posterior= nervosa and intermedia) Consists of axons whose cell bodies are in the hypothalamus Posterior lobe Antidiuretic hormone (ADH) and oxytocin are both synthesized in the hypothalamus but are stored in the posterior pituitary ADH regulates water balance and oxytocin regulates smooth muscle contractions in mammary and uterine tissues Intermediate lobe is responsible for MSH (melanocyte-stimulating hormone) Anterior lobe Certain hormones are secreted as tropic hormones that act on endocrine glands and are synthesized in the hypothalamus neuron cell bodies and stored in nerve terminals (synaptosomes) Synaptosomes release hormones into the hypothalamic-hypophyseal portal system for transport to the anterior pituitary GHRH (growth hormone releasing hormone) stimulates synthesis of GH (somatotropin) whereby somatostatin inhibits synthesis of somatotropin Anterior Pituitary cont. GnRH (gonadotropin-releasing hormone) induces gonadotrophs to produce FSH and LH – these act on gonads Corticotropin-releasing hormone (CRH) produces adrenocorticotropic hormone (ACTH) – acts on adrenal gland Thyroponin-releasing hormone (TRH) produces TSH (Thyroid Stimulating Hormone) – act on thyroid glandProlactin is synthesized by lactotrophs - Acts on mammary and gonads Anterior Pituitary cont. The tropin hormones are synthesized by the anterior pituitary hormones to target organs Typical target organs are: thyroid, pancreas, adrenal glands, gonads, etc. Androgens Two types: testicular and adrenal Testicular hormones are testosterone and androstenone Testosterone is produced in the Leydig cells of the testes. Androstenone is a pheromone Known to contribute to the boar taint odor in pork Androgens Androstenone is stored in the salivary gland and accumulates in fat depots Adrenal androgens are 17 keto steroids and are synthesized by in the cortex of the adrenal gland Growth effects are seen by the influence of testosterone of bone and muscle. This is seen by the increasing deposition of bone salts. Thus, increased bone mass is seen more in males Androgens Muscle development is seen through androgen secretions in three ways In utero, declines after birth, and increases at puberty Prenatal androgens affects myogenesis Castrated males have lower circulating GH than intact males Androgens increase both protein synthesis and degradation, yet synthesis is stimulated greater so we see an increase in protein accretion Androgens Androgens synthesis induces the development of mature male characteristics such as: larger muscles in the forequarter, neck and crest region. Castration diverts energy from growth of muscle development to fat deposition Castration helps improve quality by less muscle and more fat development at an earlier age Estrogens General classification for three hormones: Estrone, Estriol, Beta-estradiol Responsible for: growth, maturation of repro tract, female behavior, mammary development Impact: bone, fat, and muscle tissue growth Females have shorter skeletons due to: earlier epiphyseal closure that is a result of chondrocyte proliferation and a function of bone formation Estrogens Facilitates fat deposition Anabolic for ruminants Effective in castrate males for growth, yet is less effective in non-ruminants Have little effect on intact males In steers, estrogens increases muscle protein Table 10.1 Progestins Classified as steroid hormones Progesterone is a member of the progestin family which is responsible for maintenance of preg. And mammary growth and devlepment MGA is a synthetic progestin that is 100X more potent than progesterone Improves F:G ratios in heifers and suppresses estrus Synthetic Hormones Anabolic steroids – those that result in increased tissue accretion Androgens – improve growth, FE, carcass protein esp. in heifers Testosterone is anabolic Combined with estrogens, testosterone is more effective for growth parameters Synthetic Hormones TBA – Trenbolone Acetate – a synthetic steroid is weak, yet when combined with estrogen it is real effective in steers It binds to testosterone and estrogen receptors in skeletal muscle. This yields a slight decrease in protein synthesis and a significant result in (decrease) in protein degradation, thus an increase in protein accretion Growth Hormone GH or Somatotrophin (ST) Produced by the anterior pituitary Acts in an endocrine manner Liver can synthesize growth factors to help regulate growth, acts as a mediator GH stimulates the production of IGF-I Insulin-like growth factor-1; also called somatomedin Growth Hormone High concentrations of IGF-I inhibits GHRH and GH, thus reduces production of IGF-I If IGF-I is too low then GHRH & GH are not inhibited so they produce IGF-I Somatostatin is produced by the hypothalamus and delta cells of the pancreas that decreases GH secretion thus decreases IGF-I production Table 10.5 Summary of GH Effects Growth Hormone GH affects bone by using IGF-I to increase chondrocyte proliferation and osteoblast activity. GH increases lean growth by increasing rates of muscle protein synthesis and decreasing protein degradation Increases in RNA & DNA accompany increased protein accretion Growth Hormone IGF-I actions on muscle include increased uptake of glucose and amino acids IGFBP (IGF binding proteins) help transport IGF-I to target tissue like muscle GH also increases lipolysis of fatty acids from adipocytes Growth Hormone GH is a protein hormone Therefore, it is not a orally active hormone and admin. Via injection GH has been shown to increase wt. gain, feed conversion while decreasing feed intake When nutrients are limited, GH increases lipolysis, and decreases growth because IGF-I becomes uncoupled from GH, therefore IGF-I decreases. These changes causes a transfer of calories from adipose to vital functions IGF’s Are peptides that are structurally similar to proinsulin and exhibit some affinity for insulin receptors Insulin, at high conc., will bind to IGF receptors. IGF’s are secreted by the liver and by some other tissues in response to GH but they are not stored in the liver Insulin and Glucagon Islets of Langerhans within the pancreas contains four types of cells Alpha cells that synthesize glucagon Beta cells that synthesize insulin Delta cells that synthesize somatostatin ???? That synthesizes a pancreactic polypeptide Insulin At high conc. can stimulate general body growth through low-affinity binding to IGF receptors Even though there may a deficiency of insulin receptors, the number of IGF receptors are normal High circulating levels of insulin cause overgrowth of extremities and enlargement of the kidney and adrenal glands by cross reacting with IGF receptors Action of Insulin The actions of insulin on the global human metabolism level include: Control of cellular intake of certain substances, most prominently glucose in muscle and adipose tissue (about ⅔ of body cells). Increase of DNA replication and protein synthesis via control of amino acid uptake. Modification of the activity of numerous enzymes (allosteric effect). The actions of insulin on cells glycogen synthesis – insulin forces storage of glucose in liver (and muscle) cells in the form of glycogen; lowered levels of insulin cause liver cells to convert glycogen to glucose and excrete it into the blood. This is the clinical action of insulin which is directly useful in reducing high blood glucose levels as in diabetes. Increased fatty acid synthesis – insulin forces fat cells to take in blood lipids which are converted to triglycerides; lack of insulin causes the reverse. Increased esterification of fatty acids – forces adipose tissue to make fats (ie, triglycerides) from fatty acid esters; lack of insulin causes the reverse. The actions of insulin on cells Decreased proteinolysis – forces reduction of protein degradation; lack of insulin increases protein degradation. Decreased lipolysis – forces reduction in conversion of fat cell lipid stores into blood fatty acids; lack of insulin causes the reverse. Decreased gluconeogenesis – decreases production of glucose from various substrates in liver; lack of insulin causes glucose production from assorted substrates in the liver and elsewhere. The actions of insulin on cells Increased amino acid uptake – forces cells to absorb circulating amino acids; lack of insulin inhibits absorption. Increased potassium uptake – forces cells to absorb serum potassium; lack of insulin inhibits absorption. Arterial muscle tone – forces arterial wall muscle to relax, increasing blood flow, especially in micro arteries; lack of insulin reduces flow by allowing these muscles to contract. Insulin cont. There are two types of mutually antagonistic metabolic hormones affecting blood glucose levels: catabolic hormones (such as glucagon, growth hormone, and catecholamines), which increase blood glucose and one anabolic hormone (insulin), which decreases blood glucose Insulin cont. Mechanisms which restore satisfactory blood glucose levels after hypoglycemia must be quick, and effective, because of the immediate serious consequences of insufficient glucose (in the extreme, coma, less immediately dangerously, confusion or unsteadiness, amongst many other effects). This is because, at least in the short term, it is far more dangerous to have too little glucose in the blood than too much. Somatostatin Somatostatin is classified as an inhibitory hormone, whose main actions are to: Inhibit the release of growth hormone (GH) Inhibit the release of thyroidstimulating hormone (TSH) Somatostatin Suppress the release of gastrointestinal hormones Gastrin Cholecystokinin (CCK) Secretin Motilin Vasoactive intestinal peptide (VIP) Gastric inhibitory polypeptide (GIP) Enteroglucagon (GIP) Somatostatin Lowers the rate of gastric emptying, and reduces smooth muscle contractions and blood flow within the intestine. Suppress the release of pancreatic hormones Inhibit the release of insulin Inhibit the release of glucagon Suppress the exocrine secretory action of pancreas. Somatostatin opposes the effects of Growth Hormone-Releasing Hormone (GHRH) Insulin and Glucagon Glucagon and Insulin act on a negative feedback system When one goes up the other goes down Functions to mobilize glucose, fatty acids, and increase amino acid catabolism Insulin dominates the system in mammals Leptin Has been found to regulate body energy storage It is a peptide produced by adipose tissue Appears to be important in providing signals to the hypothalamus Ex. An increase in adipose tissue mass will induce production of leptin and in return will target the hypoth. to decrease food intake, increase energy expenditure and modulate other hormones such as insulin, GH, cortisol, etc., thus ultimately reducing adipose tissue mass Glucocorticoids Glucocorticoids are a class of steroid hormones characterised by an ability to bind with the cortisol receptor and trigger similar effects. Glucocorticoids are distinguished from mineralocorticoids and sex steroids by the specific receptors, target cells, and effects. Technically, the term corticosteroid refers to both glucocorticoids and mineralocorticoids, but is often used as a synonym for glucocorticoid. Cortisol Cortisol is a corticosteroid hormone produced by the adrenal cortex that is involved in the response to stress; it increases blood pressure, blood sugar levels, may cause infertility in women, and suppresses the immune system. Synthetic cortisol, also known as hydrocortisone, is used as a drug mainly to fight allergies and inflammation. Glucocorticoids Cortisol (or hydrocortisone) is the most important human glucocorticoid. It is essential for life and regulates or supports a variety of important cardiovascular, metabolic, immunologic, and homeostatic functions. Glucocorticoid receptors are found in the cells of almost all vertebrate tissues. Glucocorticoids Stimulation of gluconeogenesis, particularly in the liver: This pathway results in the synthesis of glucose from non-hexose substrates such as amino acids and lipids and is particularly important in carnivores and certain herbivores. Enhancing the expression of enzymes involved in gluconeogenesis is probably the best known metabolic function of glucocorticoids. Glucocorticoids Mobilization of amino acids from extrahepatic tissues: These serve as substrates for gluconeogenesis. Inhibition of glucose uptake in muscle and adipose tissue: A mechanism to conserve glucose. Stimulation of fat breakdown in adipose tissue: The fatty acids released by lipolysis are used for production of energy in tissues like muscle, and the released glycerol provide another substrate for gluconeogenesis. Glucocorticoids Glucocorticoids bind to the cytosolic glucocorticoid receptor. This type of receptor gets activated upon ligand binding. After a hormone binds to the corresponding receptor, the newly formed receptor-ligand complex translocates itself into the cell nucleus, where it binds to many glucocorticoid response elements (GRE) in the promoter region of the target genes. The opposite mechanism is called transrepression. Glucocorticoids The activated hormone receptor interacts with specific transcription factors and prevents the transcription of targeted genes. Glucocorticoids are able to prevent the transcription of any of immune genes, including the IL-2 gene. Glucocorticoids Generally exhibit catabolic effects Decreases muscle protein synthesis Increases muscle protein degradation Makes amino acids more available for glucose production and increases lipolysis by enhancing GH and catecholamine-stimulated lipolysis Catecholamines Catecholamines, adrenalin, norepinephrine are all stored in the adrenal medulla and is released when stimulated by nerve fibers Acts on responses to stress Adrenalin (epinephrine) acts thru the beta adrenergic receptors whereas norepinephrine act on the alpha & beta adrenergic receptors Catecholamines Effects of epinephrine include mobilization of glycogen for energy, increased blood flow, respiration, and body temp. Epinephrine induces muscle anabolic glycolysis to meet energy needs for muscle contraction Stress induced situations lead to DFD and PSE due to metabolic changes that create a final pH alteration Long term stress leads to DFD while short term or acute stress leads to PSE Catecholamines Phenethanolamines are catecholamine like synthethic cmpds that enhance growth and compositional factors in animals Feeding of beta-adregenic agonists like Ractopamine will increase lipolysis and decrease lipogenesis, thus increasing muscle by decreasing fat deposition and enhancing protein synthesis to increase muscle mass These changes may be a result of calpain proteolytic activity Catecholamines Calpains are a family of calciumdependent, non-lysosomal cysteine proteases (proteolytic enzymes) expressed ubiquitously in mammals and many lower organisms. Calpain is also involved in skeletal muscle protein breakdown due to exercise and altered nutritional states (Belcastro et al, 1996). Catecholamines Zilpaterol is another beta agonists approved in other countries but not the U.S. Table 10.10 Thyroid Hormones T 3 (Thyroxine) and T 4 (triiodothyronine) are produced in the thyroid glands They initiate insulin production in CHO metabolism They work with GH to initiate protein and nitrogen synthesis They stimulate both lipolysis & lipogenesis, yet lipolysis is greater, thus adipose tissue breakdown is greater Parathyroid hormones PTH (Parathyroid hormone) is produced by Chief cells in the parathyroid gland PTH increase bone resorption to increase calcium Calcium concentration in the muscle are important in the contraction process Parathyroid hormones It enhances the release of calcium from the large reservoir contained in the bones, enhances reabsorption of calcium from renal tubules; and enhances the absorption of calcium in the intestine by increasing the production of vitamin D Parathyroid hormones PTH also acts to decrease the concentration of phosphate in the blood, primarily by reducing reabsorption in the proximal tubules of the kidney. The decreased phosphate enhances bone demineralization. Increased calcium concentration in the blood acts (via feedback inhibition) to decrease PTH secretion by the parathyroid glands. This is achieved by the activation of calcium-sensing receptors located on parathyroid cells. Parathyroid hormones Bone resorption is the normal destruction of bone by osteoclasts, which are indirectly stimulated by PTH. Stimulation is indirect since osteoclasts do not have a receptor for PTH; rather, PTH binds to osteoblasts, the cells responsible for creating bone. Adrenal Glands In mammals, the adrenal glands (also known as suprarenal glands) are the triangle-shaped endocrine glands that sit atop the kidneys. They are chiefly responsible for regulating the stress response through the synthesis of corticosteroids and catecholamines, including cortisol and adrenaline. Adrenal Glands It is separated into two distinct structures, the adrenal medulla and the adrenal cortex, both of which receive regulatory input from the nervous system. As its name suggests, the adrenal medulla is at the center of the adrenal gland surrounded by the adrenal cortex. Adrenal Medulla The adrenal medulla is the body's main source of the catecholamine hormones adrenaline (epinephrine) and noradrenaline (norepinephrine). Composed mainly of hormone-producing chromaffin cells, the adrenal medulla is the principal site of the conversion of the amino acid tyrosine into the catecholamines adrenaline (epinephrine) and noradrenaline (norepinephrine). Adrenal Cortex Some cells of the adrenal cortex belong to the hypothalamic-pituitaryadrenal axis and are the source of cortisol synthesis. Other cortical cells produce androgens such as testosterone, while some regulate water and electrolyte concentrations by secreting aldosterone. Adrenal Cortex Situated along the perimeter of the adrenal gland, the adrenal cortex mediates the stress response through the production of mineralocorticoids and glucocorticoids, including aldosterone and cortisol respectively. It is also a secondary site of androgen synthesis. All adrenocortical hormones are synthesised from cholesterol.