Does Health Insurance Affect Health? Evidence of Medicare’s Impact on Cancer Outcomes
advertisement

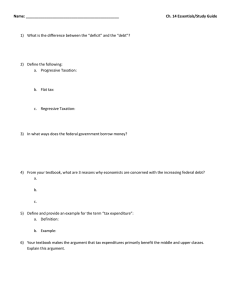
Does Health Insurance Affect Health? Evidence of Medicare’s Impact on Cancer Outcomes Srikanth Kadiyala, Ph.D. RAND Erin Strumpf, Ph.D. McGill University McGill Institute for Health and Social Policy March 27, 2013 Preliminary results: please do not cite . Draft available at: http://papers.ssrn.com/sol3/papers.cfm?abstract_id=2138454 Health Insurance and Health • Does health insurance affect health outcomes? – Lower price paid for medical care – Increased access to care – Higher quantity (quality?) of care consumed – If marginal health benefits from increased care are positive, then we expect an effect on health Measuring the Impacts • Empirically, identifying effects of health insurance on health is complicated – Many contexts have little to no variation in health insurance status (national HI systems) – In the U.S., insurance status is endogenous • Are the risk-averse and healthy more likely to be insured? • Or are the sick more likely? – If the benefits from marginal health care are small, detection of any health benefit is difficult How do we study this question? – Experimental designs are rare • RAND HIE (1970s), Oregon HIE (ongoing) – Descriptive studies lacking identification are plentiful – Better evidence from quasi-experimental studies* • Find that insurance reduces mortality and improves health status • Most focus on acute conditions: heart attack, stroke, car accidents, pregnancies – Suggests effects result from better treatment conditional on diagnosis • Some examine impact of insurance on differences by race, education, or previous insurance status * Currie and Gruber 1996, Decker and Rappaport 2002, Decker 2005, Doyle 2005, Polsky et al 2006, Card et al 2009, McWilliams et al 2009 Our Research Question • Does Medicare affect cancer health outcomes? – Approximately 12% of the U.S. population is uninsured at ages 55-64 (~4 million)* – At age 65 nearly everyone becomes eligible for Medicare • What is the effect of Medicare coverage on cancer detection? – Cancer is the 2nd leading cause of death in the U.S. – Medicare accounts for 45% of all spending on cancer treatment** – Cancer care is ~10% of Medicare spending *Kaiser Family Foundation, Health Insurance Coverage for Older Adults, May 2009 Birnbaum and Patchias 2008 estimate 5% of the age 65+ population is ineligible for Medicare **Cancer Action Network, ACS, Cancer and Medicare Chartbook 2009 Mechanisms: Detection vs. Treatment • Cancer is not necessarily a symptomatic condition – Does any effect of health insurance on health work via disease detection? – The fact that it’s not acute or symptomatic might make it more possible to identify differential effects for the uninsured • Medicare reduces the price of both screening tests and physician visits – Screening rates and physician visits increase at age 65* *Lichtenberg 2002, McWilliams et al 2003, Ward et al 2007 , Card et al 2008 Cancer Detection Data • U.S. Surveillance Epidemiology and End Results (SEER) database, 2000-2006 – Cancer detection from 25% of the U.S. population (12 states) • CA, CT, GA, HI, IA, KY, LA, MI, NJ, NM, UT, WA – Detailed information on staging, size of the tumor and other measures of cancer severity • Behavioral Risk Factor Surveillance System (BRFSS), 2000-2006 – Provides covariate data at year*age level Methodology • Regression Discontinuity Design – Uses the discontinuity in insurance status at age 65 and compares cancer detection rates on either side of this age threshold • Assumes: – Smoothness in other determinants of cancer detection across the cutoff • Education, marital status, employment, etc – In the absence of treatment (insurance), smoothness in the outcomes (detection) • Cancer risk or unobserved true incidence is smooth Analysis • Graphical Evidence • Estimate the magnitude of the discontinuity using regression – Cancer detection = α + β1(Mcare) + β2(Mcare*a-65) + β3(1-Mcare*a-65) + … + ε – Adjust for age, age2 and age3; sex, race, education, income, marital status, employment at year*year-ofage level from BRFSS • Examine cancers with screening tests separately from those that do not – Breast, colorectal, prostate, cervical (BCPC) • Assess heterogeneous impacts by preMedicare insurance status 100 50 500 -50 0 1000 1500 2000 # of Cases Per 100k 150 2500 200 All Cancers Detection 50 55 60 All Cancer Detection SEER 2000-2006, 12 states; ages 50-80 65 Age 70 75 Age to Age Change in Detection 80 Impact of Medicare on All Cancer Detection OLS OLS Poisson Medicare Cutoff 101.5*** 108.4*** 92.9*** Age Trend Above 75.8*** 75.8*** 150.2 Age Trend Below 87.4*** 85.86*** 179.0 6.4% 6.8% 5.9% Covariates Controls Included No Yes Yes N 77 77 77 % Increase relative to Detection rate at age 64 N=77, * p<=.05, ** p<=.01, *** p<=.001; Data: U.S. SEER 2000-2006 (12 states); Controls: sex, race, income quartiles, education (4), marital status (5), employment. Cutoff coefficient is robust to adding age2 and age3. Poisson model includes age2 and age3. 0 500 1000 1500 2000 Breast, Colorectal, Prostate, Cervical Detection vs. Other Cancers 50 55 60 BCPC Detection SEER 2000-2006, 12 states; ages 50-80 65 Age 70 75 Non-BCPC Detection 80 -50 0 50 100 150 BCPC vs Non-BCPC Age to Age Change in Detection 50 55 60 65 Age BCPC SEER 2000-2006, 12 states; ages 50-80 70 Non-BCPC 75 80 Effect of Medicare on BCPC Detection OLS OLS Poisson Medicare Cutoff 65.7*** 70.3*** 63.2*** Age Trend Above 21.4*** 22.8*** 192.3 Age Trend Below 40.2*** 41.9*** 206.6 9.0% 9.6% 8.7% Covariates Controls Included No Yes Yes N 77 77 77 % Increase relative to detection rate at 64 * p<=.05, ** p<=.01, *** p<=.001; Data: U.S. SEER 2000-2006 (12 states); Controls: sex, race, income quartiles, education (4), marital status (5), employment. Cutoff coefficient is robust to adding age2 and age3. Poisson model includes age2 and age3. Effect of Medicare on Non-BCPC Cancer Detection OLS OLS Poisson Medicare Cutoff 35.8*** 38.0*** 29.7** Age Trend Above 54.4*** 53.0*** -31.8 Age Trend Below 47.2*** 44.0*** -17.8 4.2% 4.5% 3.5% Covariates Controls Included No Yes Yes N 77 77 77 % Increase relative to detection rate at age 64 * p<=.05, ** p<=.01, *** p<=.001; Data: U.S. SEER 2000-2006 (12 states); Controls: sex, race, income quartiles, education (4), marital status (5), employment. OLS cutoff coefficient is robust to adding age2 and age3. Poisson model includes age2 and age3. Stage at Detection for BCP Cancers • 80% of newly detected breast cancer cases are at local or regional stages • 65% of newly detected CRC cases are at regional or distant stages • 81% of newly detected prostate cancer cases are at the local stage • About 45% of newly detected cases for these three cancers are at “treatable” stages* where we expect diagnosis to lead to significant health benefits – Conservative estimate based on concerns about over-diagnosis and treatment * Local and regional for breast; in-situ, local and regional for colorectal; regional for prostate Initial Conclusions • Medicare increases the cancer detection rate by a substantial amount • Medicare’s effects on cancer detection are larger for cancers with recommended screening tests – Breast cancer detection rate: 6% increase – Colorectal and prostate: 9% increases – No impact on cervical cancer detection • Impacts for non-screening cancers as well • An important share of newly detected cases are treatable and health improvements are likely Effects by Pre-Medicare Insurance Status • We expect differential detection effects for those uninsured pre-Medicare – Large change in insurance status – But quality of insurance may change for those previously insured (ie, screening mandates) • SEER does not include insurance status Insured vs. Uninsured Analysis • State Insurance Rates – Variation in insurance rates at age 64 by state, 2000-06 • 77% in Louisiana, 92% Michigan – Correlate RD estimates of the increase in insurance coverage from age 64 to 65 with RD estimates of the change in cancer detection – Control for state and time fixed effects Correlation of RD Estimates Detection Linked to Changes in Insurance Status • State-level variation in health insurance discontinuities due to Medicare can explain 37-71% of the state-level variation in BCPC detection due to Medicare • We did not identify a similar relationship with respect to Non-BCPC detection • Suggests that the extensive margin is important, but it’s possible that quality of insurance coverage also plays a role Conclusions • Health insurance plays a role in improved health in the context of chronic, latent disease • Medicare increases the cancer detection rate by 6.4%, about 100 cancers per 100,000 individuals • Larger detection effects for screening cancers, but also effects for non-screening • The increase in insurance rates at age 65 can account for a significant share of the increase in screening cancer detection