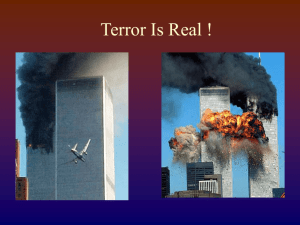
Terror Is Real !
advertisement

Terror Is Real ! Terrorism: Are We Ready? Barbara Russell, RN,MPH,CIC,ACRN Biological and Chemical Terrorism: How Real is the Threat? What is Terrorism? No single definition FBI: “The unlawful use of force or violence against persons or property to intimidate or coerce a government, the civilian population, or any segment thereof, in furtherance of political or social objectives.” “Kill 1, Frighten 10,000” Sun Tzu Anthrax 2001 22 confirmed or suspected cases 11 inhalation (confirmed) 11 cutaneous (7 confirmed, 4 suspected) Inhalation Anthrax (11) 9 confirmed - exposed to mail (other 2 possible) 55% (6) survived Types of Terrorism Biological Nuclear Incendiary Chemical Explosive B-NICE Target Selection SSymbolic target to audience or terrorist Economic, political, social or religious value Highly visible and photogenic Random: To create confusion Diversionary Asymmetrical attack Timing Anniversary of significant historical event Highly visible event in the area Increase in international tensions Chemical & Biological Terrorism 1984: 1991: 1994: 1995: 1995: 1997: 1998: 1998: The Dalles, Oregon, Salmonella (salad bar) Minnesota, ricin toxin (hoax) Tokyo, Sarin and attack Arkansas, ricin toxin (hoax) Ohio, Yersinia pestis (sent in mail) Washington DC, “Anthrax” (hoax) Nevada , non-lethal strain of B. anthracis Multiple “Anthrax” hoaxes Chemical Warfare Agents Tokyo Subway Attack •Odon March 20, 1995, terrorists released sarin, an organophosphate (OP) nerve gas at several points in the Tokyo subway system, killing 11 and injuring more than 5,500 people. Concealed in lunch boxes and soft-drink containers and placed on subway train floors. It was released as terrorists punctured the containers with umbrellas before leaving the trains. •.On April 19th, 1995 repeat attack in subway which the same terrorist group killed seven and injured more than 200 people. Chemical Warfare Agents (CWA) Lethal CWA’s Nerve gas (Sarin, Tabun, soman, and VX) Organophosphates- anticholinesterase Colorless, odorless, tasteless Cyanides Vesicants (=blistering ) agents – mustard gas Nerve Gas Agents All nerve agents belong chemically to the group of organo-phosphorus compounds. Stable and easily dispersed, highly toxic and have rapid effects both when absorbed through the skin and via respiration. Nerve agents can be manufactured by means of fairly simple chemical techniques. The raw materials are inexpensive and generally readily available. Chemical Chemical agents are toxic, but… - They can be detected - You can protect yourself - Victims can be decontaminated Can be inhaled, absorbed through the skin or injected Nerve Agent Symptoms Salivation Lacrimination Urination Defecation Gastrointestinal pain Emesis SLUDGE Decontamination Removes the agent from the patient Reduces the chance of secondary spread Helps the victim psychologically Nerve Gas Poisoning Eyes: excessive lacrimation and pain. Symptoms: minutes to 2 hours Treatment: Atropine, 2-PAM (pralidoxime-2-chloride) Decontamination: Soap & Water, Chlorox Skin: excessive sweating Muscles: involuntary twitching Respiratory: Mucous secretion, dyspnea Digestive: excessive salivation, abdominal pain Sulfur Mustard Poisoning Eyes: reddening, congestion, pain 1/2 -12 hours Skin: itching, burning, erythema, large blisters (1-12 hours) Respiratory: burning throat, cough, dsypnea. (2-12 hours) Digestive: abdominal pain, nausea, blood stained vomiting and diarrhea Treatment: none Decontamination: Soap & Water, Chlorox Care: watch for leukopenia, debride bullae “I’m confident that we can defend against chemical warfare. The one that really scares me to death is biological” Colin Powell - 1993 Potential Biological Weapon Agents Characteristics of a Biological Attack: Civilian Targets Likely. Possibility of Large Numbers of Casualties. Symptoms May Not Appear For Days. Initial Symptoms Likely to be Non-Specific. Diagnoses Will Depend Heavily Upon Laboratory Tests. Complex Epidemiology. Ongoing Need to Care for Large Numbers of Patients Concerns About Availability of Drugs, Supplies, Staff Members. Legal Considerations. Coordination with Local, State, and Federal Authorities. Potential Bioterrorism Agents Bacterial Agents Anthrax Brucellosis Cholera Plague, Pneumonic Tularemia Smallpox VEE VHF Source: U.S.A.M.R.I.I.D. Viruses Biological Toxins Botulinum Staph Entero-B Ricin T-2 Mycotoxins Biological Agents of Highest Concern Variola major (Smallpox) Bacillus anthracis (Anthrax) Yersinia pestis (Plague) Francisella tularensis (Tularemia) Botulinum toxin (Botulism) Filoviruses and Arenaviruses (Viral hemorrhagic fevers) ALL suspected or confirmed cases should be reported to health authorities immediately Anthrax - The Weapon Bacillus anthracis (coal = anthrakis) because of black coal like lesions Aerobic, gram-positive, spore forming, non-motile bacillus species. Inhalation Anthrax: Most morbidity and mortality as aerosolized biological weapon. Disease occurs 2 to 43 days after exposure. Anthrax - The Disease Inhalation anthrax: Hemorrhagic thoracic lymphadenitis Hemorrhagic mediastinitis Hemorrhagic meningitis Two Stages 1. Fever, cough, dyspnea, headache, vomiting, chills, weakness 2. Sudden fever spikes, dyspnea, shock, cyanosis, hypotension Mortality: 89%!!!! Anthrax: Diagnosis, Prevention, Treatment CXR: widened mediastinum Blood culture shows growth after 2-6 hours Vaccine: Licensed since 1970, 88% effective, not available! Treatment: PNC, Doxycycline, Ciprofloxacin, first generation cephalosporin, vacomycin, clindamycin Anthrax Cause Bacillus anthracis Incubation 1-60 days, average 7 days Mortality (without treatment) Cutaneous: 20% Intestinal: 25%-60% Inhalation: Usually fatal Varied; 8,000-50,000 spores (inhalation) Yes; antibiotics and supportive care No Infectious Dose Treatable? Human to Human Transmission? Anthrax (bacillus anthracis) What is smallpox? Serious, contagious, viral disease that causes a fever and distinctive rash Treatment: supportive Historically, 30% of smallpox patients died, many developed scars especially on face, some became blind Prevented by smallpox vaccine (>95% effective) How is smallpox spread? By direct, prolonged face-to-face contact Less commonly, indirectly by contaminated bedding or clothing Rarely spread by air Transmission prevented by using airborne and contact precautions in health care settings What is the risk of smallpox? 1972: routine smallpox vaccination discontinued in U.S. 1977: last naturally-acquired case in world Deliberate release is possible but risk is unknown Health care workers at higher risk due to exposure to most severely ill patients In Europe from 1950-71, 50% of smallpox transmission was in hospitals How the skin looks with successful vaccine “take” Smallpox Cause Variola major Incubation 7-17 days, average 12-14 days 30% Mortality (without treatment) Infectious Dose Treatable? Human to Human Transmission? Small Supportive care; vaccine after exposure Yes - Airborne Smallpox vs. Chickenpox Smallpox Distribution of pox Stage of pox development Unique presentation Chickenpox Centrifugal distribution (face, arms, legs) All at same stage of development More covered parts of body, trunk Pox found on palms and soles of feet Uncommon to find pox on palms and soles of feet Various stages of development Smallpox (variola major) Treatment Treatment of smallpox is limited to supportive therapy and antibiotics as required for treating secondary bacterial infections. There are no proven antiviral agents effective in treating smallpox. Plague Found in rodents and their fleas in many parts of the world Bites from an infected flea Bubonic, septicemic, pneumonic Seen in rural areas (US: 10-15 cases per year) Two recent human cases of primary pneumonic plague contracted from cats Plague (cont) US: 390 cases from 1947-1996 - 84% bubonic (standard precautions) - 13% septicemic (standard precautions) - 2% pneumonic (droplet precautions) Patients may present with GI symptoms (N/V, abd pain) Treated with antibiotics Plague (cont) BBiological terrorism release clues: - Pneumonic plague outbreak 1-6 days after exposure - Initial severe respiratory illness - Death occurs quickly after onset of illness - Infection in persons with no known risk factors Plague (cont) BBiological terrorism release clues (cont) - Occurrence of cases in areas not known to have previous cases - Absence of prior rodent deaths (which may be present after natural disaster) Plague vs. Anthrax presentation Plague (yersinia pestis) Plague Cause Yersinia pestis Incubation 2-6 days Mortality (without treatment) Infectious Dose 50% (bubonic); near 100% (pneumonic) Small Treatable? Yes; antibiotics and supportive care Pneumonic: Yes Bubonic: No Human to Human Transmission? Botulism Most potent naturally occurring lethal substance known to man Possible routes of exposure: Ingestion (food), Inhalation (terrorist), Injection (drug users), dirty wound In 1999…………. 174 cases 26 food borne 107 intestinal / infant 41 wound Botulism (cont) CCardinal Signs - Fever is absent (unless infection is present) - Neurological symptoms are symmetrical - Patient remains responsive - Heart rate normal or slow - Sensory deficits do not occur (except for blurred vision) Botulism (cont) IIncubation period - Food borne: 12-36 hours (preformed toxin) - Intestinal (Infant): 1-2 weeks - Wound: 4-14 days Botulinum Toxin Cause Clostridium botulinum Incubation 2 hours – 8days, average 1272 hours (foodborne) High Mortality Lethal Dose Treatable? Human to Human Transmission? 1 ng/kg (about 0.00000009g/200lb person) Yes; antitoxin and supportive care No Tularemia Reservoir: Numerous wild animals (i.e.: rabbits, beavers, some ticks) Can also be found in contaminated water, soil, vegetation Infections occur in North America (US: 171 cases / year) – AKA Rabbit Fever, Deer Fly Fever Infection caused by handling infectious animal tissues or fluids, direct contact with contaminated water, food, soil and inhalation of aerosols. Tularemia (francisella tularensis) Tularemia Cause Francisella tularensis Incubation 1-14 days, average 3-5 days Varies; 5%-60% Mortality (without treatment) Infectious Dose Treatable? Human to Human Transmission? 10 organisms Yes; antibiotics and supportive care No Hemorrhagic Fevers Ebola, Marburg, Lassa, Junin & related viruses Presentation: Initially febrile illness, malaise, myalgias, H/A, vomiting, diarrhea followed by bleeding, hypo tension, shock Mode of Transmission: Contact with infected blood or other materials, higher risk at late stages of illness Hemorrhagic Fevers (cont) Incubation period (days): - Ebola 2-21, -Lassa, commonly 6-21 - Junin 7-16 - Marburg 3-9, Diagnostic Tests Available Significant number of people with hemorrhagic fever symptoms Intensive supportive care Standard and Contact Precautions Hemorrhagic Fever Cause Varies; viral Incubation Varies; days to weeks Mortality (without treatment) Infectious Dose Varies; high (as much as 80%) Unknown Treatable? No; supportive care only Human to Human Transmission? Yes Key Points Increase Level of Awareness Be familiar with Workplace Plan Be familiar with County Plan Have a Family Plan No “I” in Response – It’s a Team Effort Personal Protective Equipment Be sure that it is Appropriate to the hazard(s)