Heparin resistance Agenda BJA, 2002 vol 88, no 4, 467-469
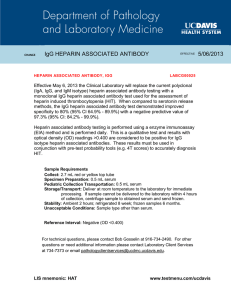
advertisement

Agenda Heparin resistance BJA, 2002 vol 88, no 4, 467-469 J A M Anderson and E L Saenko Overview Heparin was discovered in 1916 Most widely used anticoagulant but not all its actions are fully understood Eg: pain relief in i.v administration for the treatment of DVT, how HIT developed and what is the relevance of the occurrence of heparin resistance Indications Prevention of VTE Treatment of VTE Acute coronary syndrome Surgery: cardiac bypass Introduction Heparin is a negatively charged sulphated glycosaminoglycan composed of alternating uronic and glucoronic acid residues Commercially prepared are isolated fr porcine int mucosa or bovine lungs. There are heterogenous mixtures of polysacharide chains ranging in molecular weight from 3000 to 30,000. Mode of action: MOA 1 1. Antithrombin dependent -Activate AT Hep-AT complex inactivate thrombin, fXa and other coagulation factors The combination of disaccharide units makesup pentasacharide sequence containing high affinity binding site for AT. This sequence occurs in only about 1/3 rd of heparin chains and is randomly distributed MOA 2 2. AT independent Direct Inhibition of the intrinsic tenase complex ( PL complex of FVIIIa, FIXa which generates Fxa) * In plasma milieu, AT-dependent effect predominates In vivo, variation in response to a fixed dose of heparin occurs bet individuals Pharmacokinetics limitation of heparin caused by the binding of hep to plasma proteins Heparin resistance state Significance to know the ‘R’ state 1. Prevent over administration of heparin hemorrhagic consequences Particularly during post-op or in the setting of cardiac bypass surgery and to consider alternative therapy In VTE the phenomenon is of unclear clinical practice 2. Definition of heparin resistance state 1. In the context of VTE: The need for more than 35,000 u/24 hour to prolong the APTT into the therapeutic range 2. Cardiac bypass procedure: The definition is based on the ACT with at least one ACT < 400 secs after heparinization and/or the need for exogenous antithrombin administration Questions 1. What causes heparin resistance 2. Which patient groups are susceptible? Some answers can be gained from the understanding on the limitation of UFH Limitations of heparin 1. Biophysical Reflects the inability of hep-AT complex to inactivate FXa bound to platelets within the prothrombinase, the PL memb bound fVa – fXa complex, in addition to the resistance of fibrin bound thrombin to inactivation by heparin Limitation of heparin 2 2. Pharmacokinetic A. Reflects the binding of hep to plasma proteins including PF4, fib, fVIII and histidine rich glycoprotein As many heparin- binding poteins are acute phaase proteins/reactants- the phenomenon is often encountered in acutely ill pts, malignancy, peri or post partum periods and drugs ( aprotinin and nitroglycerin – hep clearance) B. Lowering of the AT levels by heparin contributes to the resistance state How to monitor the anticoagulant effects of heparin in the lab? … not easy 1. APTT failed to prolonged APTT has its own limitations: Influenced by: -blood collection -Sampling tube composition -Type of anticoagulant -Time of sampling to avoid PF4 mediated neutralization of heparin * APTT response to heparin varies APTT response to Heparin Possibolity of ApTT lies in the target range for heparin therapy whilst the heparin levels is suboptimal occurs in acquired/congenital factor deficiency, LA, warfarin effects. Monitor 2. Anti- Xa monitorring Less dose of heparin is required compared to when APTT is used as monitorring agent The development of heparin resistance is therefore an indication for the use of the heparin assay to measure the anticoagulant effect of the drug Chromogenic anti fXa assays have limitations: assay variation and technique Bedside anti fXa monitorring test to permit a quicker and more accurate asessment of the true anticoagulant activity of heparin: bypass surgery Monitor 3. ACT At present ACT, is the most commonly used lab test to control heparin effects on extracorporeal membrane ACT results also dependent on the instrumentation, vary with the presence of haemodilution and hypothermia Heparin Resistance and CPB CPB circuitECM: activate the coagulation pathway fXa generation. The inhibition of Fxa in these situations involves the AT dependent mechanisms of heparin. Imbalance of activation of FX via extrinsic vs intrinsic p/way In general, hep is given 3mg/kg body wt to prevent extracorporeal clot formation with repeated doses to maintain ACT > 400 sec to maintain level at 3iu/ml Solution to heparin resistance during CPB Potential solution: Argatroban: a selective, reversible thrombin inhibitor Hirudin also a direct thrombin inhibitor : prevent clotting within the CPB circuit of pts with HIT Ecarin clotting time to monitor the antithrombotic effects (PT activation by the snake venom) Pentasacharide: a selective synthetic fXa inhibitors: once daily subcut dose without monitoring requirement (prevention of venous thrombosis) Conclusion Heparin still remains the optimal means of anticoagulation in CPB, but improvements are needed in terms of practical bedside monitorring of its anticoagulant effects. Bedside monitorring permit reasessment of the optimal level of ACT to achieve prior to starting the bypass circuit Significance of heparin resistance In the context of VTE- heparin R has its clinical relevance? What is the outcome of pts treated with empirical doses of heparin when APTT cannot be prolonged into the therapeutic range? The optimal means of monitorring the anticoagulant effects in cardiac surgery? to avoid bleeding post-op and usage of blood products Oral heparin in future and synthetic indirect and direct fXa inhibitors.