Glaucoma & Cataract Dr Ibraheem Bashayreh, RN, PhD
advertisement

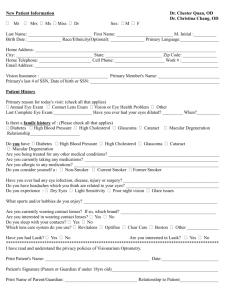
Glaucoma & Cataract Dr Ibraheem Bashayreh, RN, PhD Glaucoma Glaucoma is optic nerve damage (often, but not always, associated with increased eye pressure) that leads to progressive, irreversible loss of vision. Glaucoma Damage to the optic nerve can occur when pressure within the eye increases. The vision loss occurs so slowly that it may not be noticed for a long time. People at risk should have a complete eye examination, including measurement of eye pressures and testing of side (peripheral) vision. Eye pressure needs to be controlled throughout life, usually with eye drops but sometimes with eye surgery Epidemiology Almost 3 million people in the United States and 14 million people worldwide have glaucoma. Glaucoma is the third leading cause of blindness worldwide and the second leading cause of blindness in the United States, where it is the leading cause of blindness among blacks and Hispanics. In the United States, about one third of glaucoma occurs with eye pressures within the average range, a condition called low-tension glaucoma. Risk Factors Age older than 40 Family members who have (or had) the disease Farsightedness or nearsightedness Diabetes Long-term use of corticosteroid drugs Previous eye injury Congenital Mechanism Glaucoma occurs when an imbalance in production and drainage of fluid in the eye (aqueous humor) increases eye pressure to unhealthy levels. Normally the aqueous fluid, which nourishes the eye, is produced by the ciliary body behind the iris (in the posterior chamber) and flows through the pupil to the front of the eye (anterior chamber), where it exits into drainage canals between the iris and cornea (the “angle”). When functioning properly, the system works like a faucet (ciliary body) and sink (drainage canals). Balance between fluid production and drainage— between an open faucet and a properly draining sink— keeps the fluid flowing freely and prevents pressure in the eye from building up. Mechanism In glaucoma, the drainage canals become clogged, blocked, or covered. Fluid cannot leave the eye even though new fluid is being produced in the posterior chamber. In other words, the sink “backs up” while the faucet is still running. Because there is nowhere in the eye for the fluid to go, pressure in the eye increases. When the pressure becomes higher than the optic nerve can tolerate, damage to the optic nerve occurs. This damage is called glaucoma. Sometimes eye pressure increases within the range of normal but is nonetheless too high for the optic nerve to tolerate (called low tension glaucoma). Classification Open-angle glaucoma Closed-angle glaucoma Etiology In most people, the cause of glaucoma is not known, Although both open-angle and closed-angle glaucomas tend to run in families. In others, damage to the eye caused by infection, tumour, inflammation, large cataracts or surgery for cataracts, or other conditions keeps the fluid from draining freely and leads to increased eye pressure and optic nerve damage (secondary glaucoma). Open-angle glaucoma: • • • is more common the drainage canals in the eyes become clogged gradually over months or years. Pressure in the eye rises slowly because fluid is produced at a normal rate but drains sluggishly. Symptoms Open-Angle Glaucoma: painless and causes no early symptoms. The most important symptom is the development of blind spots, or patches of vision loss, over months to years. The blind spots slowly grow larger. Peripheral vision is usually lost first. Vision loss occurs so gradually that it is often not noticed until much of it is lost. Because central vision is generally lost last, many people develop tunnel vision: they see straight ahead perfectly but become blind in all other directions. If glaucoma is left untreated, eventually even tunnel vision is lost, and a person becomes totally blind. Closed-angle Glaucoma is less common than open-angle glaucoma. The drainage canals in the eyes become blocked or covered because the angle between the iris and cornea is too narrow. The blockage can occur suddenly or slowly. If the blockage occurs suddenly, pressure in the eye rises rapidly. If the blockage occurs slowly, the pressure in the eye rises slowly like in open-angle glaucoma. Symptoms Closed-Angle Glaucoma If eye pressure rises rapidly in closed-angle glaucoma (acute closed-angle glaucoma), people typically notice an abrupt onset of severe eye pain and headache, redness, blurred vision, rainbowcolored halos around lights, and sudden loss of vision. They may also have nausea and vomiting as a response to the increase in eye pressure. Acute closed-angle glaucoma is considered a medical emergency, because people can lose their vision as quickly as 2 to 3 hours after the appearance of symptoms if the condition is not treated. People who have had open-angle or closed-angle glaucoma in one eye are likely to develop it in the other. Screening and Diagnosis • • • • An early detection of the disease is extremely important. All people at high risk of glaucoma should have a comprehensive eye examination every 1 to 2 years There are four parts to a comprehensive eye examination for glaucoma Monitoring eye pressure (20-22 mm Hg) Ophthalmoscope and a slit lamp to look for changes in the optic nerve Visual field (peripheral vision) testing allows a doctor to detect blind spots Doctors may also use a special lens to examine the drainage channels in the eye Treatment The goal of glaucoma treatment is to prevent the onset of vision loss or stop its progression. Treatment of glaucoma is lifelong. It involves decreasing eye pressure by increasing fluid drainage out of the eyeball or by reducing the amount of fluid produced inside the eyeball. Some people with high eye pressure who do not have signs of optic nerve damage (known as glaucoma “suspects”) can be monitored closely without treatment. Treatment Eye drops and surgery are the main treatments for open-angle and closed-angle glaucomas. Eye drops containing beta-blockers, prostaglandin-like compounds, alphaadrenergic agonists, carbonic anhydrase inhibitors, or cholinergic drugs are commonly used to treat glaucoma. Laser surgery can be used to increase drainage Cataract A cataract is a clouding (opacity) of the lens of the eye that causes a progressive, painless loss of vision. Epidemiology Cataracts are the leading cause of blindness worldwide. Cataracts are common in the United States, where they affect mostly older adults. Almost one in five people between the ages of 65 and 74 develop cataracts severe enough to reduce vision, and almost one in two people older than 75 have them. Etiology Cataracts usually develop without any apparent cause; however, contributing factors include the following: Injury to the eye Prolonged use of certain drugs (such as corticosteroids) Prolonged exposure to x-rays (such as with radiation therapy to the eye) Inflammatory and infectious eye diseases Diseases such as diabetes Dark eyes Prolonged exposure to direct sunlight Poor nutrition Smoking Alcohol use Heat from infrared exposure Mechanism On the left, a normal lens receives light and focuses it on the retina. On the right, a cataract blocks some light from reaching the lens and distorts the light being focused on the retina. Types of Cataract The lens consists of three layers The outer layer is a thin, clear membrane It surrounds a soft, clear material (cortex) The hard center of the lens is the nucleus A cataract can form in any part of the lens Nuclear Cataract Occurs in the center of the lens In its early stages, the patient may become more nearsighted or even experience a temporary improvement in reading vision This so-called “second sight” disappears as the lens gradually turns yellow and begins to cloud the vision Seeing in dim light and driving at night may be especially troublesome Cortical Cataract Begins as whitish, wedge-shaped streaks on the outer edge of the lens cortex As it slowly progresses, the streaks extend to the center and interfere with light passing through the nucleus Both distance and near vision can be impaired Patients also have problems with glare and loss of contrast Subcapsular Cataract Starts as a small, opaque area just under the capsule shell, usually at the back of the lens, right in the path of light on its way to the retina This type of cataract may occur in both eyes but tends to be more advanced in one eye than the other Often interferes with reading vision, reduces your vision in bright light and causes glare or halos around lights at night Symptoms Blurred vision Increasing difficulty with vision at night Glare, especially at night Halos around lights The need for brighter light for reading Double vision in a single eye Fading or yellowing of colors The lens appears cloudy Diagnosis A doctor can usually detect a cataract while examining the eye with an ophthalmoscope. A doctor can identify the exact location of the cataract and the extent to which it blocks light by using an instrument called a slit lamp, which allows examination of the lens and other parts of the eye in more detail. Prevention Consistent use of sunglasses with a coating to filter ultraviolet (UV) light Not smoking is useful and has other health advantages. People with diabetes should work with their doctor to be sure the level of sugar in their blood is well controlled. A diet high in vitamin C, vitamin A , and substances known as carotenoids (contained in vegetables such as spinach and kale) may protect against cataracts. Estrogen use by women after menopause may also be protective, but estrogen should not be used solely for this purpose. Finally, people who are taking corticosteroids for extended periods might discuss with their doctor the possibility of using a different drug. Treatment Until vision is significantly impaired, eyeglasses and contact lenses may improve a person's vision. Wearing sunglasses in bright light and using lamps that provide over-the-shoulder lighting may decrease glare and aid vision. Occasionally, drugs that keep the pupil dilated may be used to help vision if the cataract is small and located in the center of the lens. The only treatment that provides a cure for cataracts is surgery. MACULAR DEGENERATION MECHANISM – (The area next to optic disc that defines fine details at the center of visual field = macula) * not enough blood supply to area (disappearance of central vision due to deterioration of pigment layer of retina) ETIOLOGY – * age – * atherosclerosis * hemorrhage SYMPTOMS AND SIGNS – * Fine detailed vision is impaired * Sharp vision deterioration (reading) * peripheral vision is not affected * loss of central vision DIAGNOSIS – * Ophthalmoscopy * fluorescein angiography * patient history TREATMENT – * no known cure * laser photocoagulation * increase zinc in diet * strong magnifying glasses DIABETIC RETINOPATHY MECHANISM – * constriction of ocular blood vessels & leakage of blood into retina (microaneurysms, neovascularization = new blood vessels) * leakage of blood into vitreous humor * scar tissue ETIOLOGY – diabetics with uncontrolled glucose levels SYMPTOMS AND SIGNS – * impaired sharp vision * blurred vision * could lead to permanent blindness DIAGNOSIS – * Ophthalmoscopy TREATMENT – * Laser photocoagulation * vitrectomy Thank You!