Cancer Pain Management Ann L. Janer
advertisement

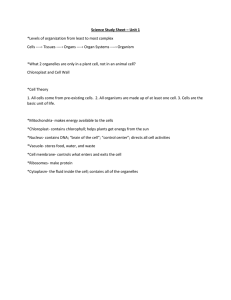
Cancer Pain Management Ann L. Janer Pain Management • Pain is an unpleasant sensation, a symptom, a subjective experience, a complex interaction of neuro-systems with the interaction of biochemical, physiological, psychological, and neocortical processes. It is influenced by attention, anxiety, suggestion, fatigue, prior conditioning and the extent of tissue damage. Pain Receptors • found in abundance in the superficial layers of skin • found in periosteum, arterial walls, joint surfaces and parts of the cranial vault • Deep internal structures have few to no pain receptors Pain Sensation • Pain receptors do not adapt to stimulation as other sensory receptors; • with repeated stimulation, pain receptor sensitivity and sensation may actually increase; • intensity of pain is correlated to rate of tissue damage Causes of Pain Ischemia...as blood flow to a tissue is decreased and blocked, pain results, caused by… • lactic acid (anaerobic metabolism) • cell damage leads to accumulation of bradykinin and proteolytic enzymes Causes of Pain Muscle Spasm as a Cause of Pain • spasm stimulates mechanical pain receptors AND • compression of blood vessels by the spasm induces ischemia Stimulation of Pain Receptors Mechanical • excessive mechanical stretch triggers the response • e.g. inflammation, edema, tumor Thermal • extremes of heat (>45°C) or cold Stimulation of Pain Receptors Chemical • usually responsible for stimulating slow, aching pain which follows an injury. • some chemicals excite the chemical pain receptors and some enhance the sensitivity of pain nerve endings. Pain Message Control Gate Control • The transmission of painful information can be modulated by afferent input from the periphery, descending inhibitory systems, cognitive and emotional factors. Pain Message Control Corticifugal Signals • Inhibitory signals from the cerebral cortex to lower "relay stations" of the thalamus, medulla and spinal cord. • Control the sensitivity of the sensory input. (When input intensity becomes too great, corticifugal signals automatically decrease the transmission.) Pain Message Control Corticifugal Signals cont. • This decreases the lateral spread of sensory signals to adjacent neurons and it keeps the sensory system operating in a range of sensitivity so that signals are neither too low (ineffective) or too high (unable to differentiate sensory patterns). Endogenous Opioids • Enkephalins act at peripheral neural sites occur at the dorsal root ganglion, spinal cord, midbrain, hypothalamus, periaquaductal gray area and rostral medulla. Endogenous Opioids • Enkephalin is believed to cause presynaptic inhibition of both incoming type C and A delta fibers where they synapse in the dorsal horns. The probable mechanism is via calcium channel blockade in the nerve terminals. The inhibition apparently lasts for prolonged periods of time as analgesia lasts from minutes to hours. Other Pain Inhibition Pathways Adrenergic Pathways • Norepinephrine acts at the dorsal horn (descending impluses) to inhibit pain; • By a different mechanism (enhancing prostacycline production), it can also enhance peripheral pain. Other Pain Inhibition Pathways Serotonin Pathways • Centrally mediated pain modulation via a descending pathway along the spinothalamic tract • Presynaptic reuptake inhibition of serotonin and norepinephrine (amitriptyline-Elavil) is key. SSRI's (fluoxetine-Prozac) not as effective modulating neurogenic pain as TCA’s Other Pain Inhibition Pathways Cholinergic Pathway • Binding sites responsive to acetylcholine have been found in the dorsal horn. Other Pain Inhibitory Pathways GABA-ergic Pathway - 2 types of receptors • GABAA sensitive to muscimol and • GABAB which is sensitive to baclofen (Lioresal) • Greatest effect - C fibers; baclofen is effective in treating central pain syndromes especially associated with muscle spasms. Pain Management Goal • The goal is to identify the specific origin and cause of the pain so that medical, surgical or drug treatment may be implemented. The pain threshold can be lowered by fear, anxiety, depression, fatigue, or anger. It can also be raised by rest, mood elevation, sympathy, diversion or understanding. Acute Pain • Injury, trauma, spasm or disease to skin, muscle, somatic structures or viscera; • Perceived and communicated via peripheral mechanisms (pathways) A delta and C fibers • Usually with autonomic response as well (tachycardia, blood pressure, diaphoresis, pallor, mydriasis (pupil dilation); Acute Pain • Usually subsides quickly as pain producing stimuli decreases • Associated with anxiety-(decreases rapidly) • Can be understood or rationalized as part of the healing process. Acute Pain Somatic-Superficial • Initiated in skin, subcutaneous or mucous tissues • Characterized by throbbing, burning, or pricking sensations; associated with tenderness, allodynia (pain from a usually non-pain stimulus) or hyperalgesia Acute Pain Somatic-Deep • Generally initiated in musculoskeletal tissue • Characterized by dull, aching pain which CAN be localized; pain may radiate Acute Pain Visceral • Initiated in the abdomen or thorax difficult to localize • Frequently associated with referred pain sites Referred Pain • • • • Appendix > Umbilicus Esophagus > Neck, Pharynx, Middle Chest, Arm Gallbladder > Right shoulder, Central abdomen Heart > Lower neck, shoulders; Radiates down either arm (left more common than right) Referred Pain • • • • • Kidneys > Lower back, Flank Stomach > Upper abdomen, Chest Ureters > Anterior abdominal wall, Back, Flank Urinary Bladder > Lower abdomen, Vagina Uterus > Lower abdomen, Back, Groin, Pelvis Chronic Pain • • • • Non-malignant Pain persists beyond the precipitating injury Rarely accompanied by autonomic symptoms Sufferers often fail to demonstrate objective evidence of underlying pathology. • Characterized by location-visceral, myofacial, or neurologic causes. Chronic Pain • Malignant • Has characteristics of chronic pain as well as symptoms of acute pain (breakthrough pain). • Has a definable cause, e.g. tumor recurrence • In treatment, narcotic habituation is generally not a concern. Pain Perception Pain perception and response are different • actual tissue injury (mech., thermal, or chemical) • intensity & duration of the insult • function of nerves’ spinothalamic paths • central nervous system pain mediators & neurotransmitters • social, religious, psychological & cultural factors Initial Pain Assessment • • • • Patient Interview including PQRST for pain Intervention History Physical Exam (include MMS) Labs & Radiology (thyroid profile, CBC, ESR, Radiograph, ECG) • Functional Assessment (ADL) & Psychological Assessment • Treatment Access ABCDE of Pain Management • • • • A Ask about pain regularly; Assess systematically. B Believe pt. & family’s report of pain & relief. C Choose pain control appropriate for pt.& family. D Deliver interventions in a timely, logical & coordinated manner. • E Empower pts. & families; Enable them to have as much control as possible. Pain Evaluation PQRST • P palliative/provocative • Q quality • R region/radiation • S subjective/severity • T temporal/time factors Severity Assessment Visual Analog Scale (VAS) • No Pain ---> 10 cm line ---> As bad as it can be • Faces of Pain (Ouchers) - similar to the visual analog scale J ------->L Severity Assessment Numerical Rating Score (NRS - similar to VAS) |----|----|----|----|----|----|----|----|----|----| 0 1 2 3 4 5 6 7 8 9 10 • (for children or adults who understand numerical relationships) Severity Assessment McGill Pain Questionnaire • 0 ----------> 5 • None -------------------> Excruciating • Mild, Discomforting, Distressing, Horrible, in between. WHO Pain Management Scale Step 3 Step 2 Step 1 NSAIDS, + adjuvants NSAID + mild opioids + adjuvant strong opioids + NSAIDS + adjuvants VAS vs WHO VAS 1-3 4-6 7 - 10 WHO Steps Step 1 Step 2 Step 3