FEATURES AND USE OF DERMATOLOGIC PREPARATIONS
advertisement

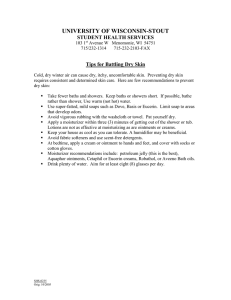
FEATURES AND USE OF DERMATOLOGIC PREPARATIONS Features • Among the dosage forms used in the topical treatment of conditions and diseases of the skin are ointments, creams, gels, pastes, and plasters. • In treating skin diseases, the drug in a medicated application should penetrate and be retained in the skin for a while. • Drug penetration into the skin depends on a number of factors, including: 1. the physicochemical properties of the medicinal substance, 2. the characteristics of the pharmaceutical vehicle, 3. the condition of skin itself. Normal unbroken skin acts as a natural barrier, limiting both the rate and degree of drug penetration. The skin • The skin is divided histologically into , collectively a laminate of barriers protecting against permeation by external agents and loss of water from the body: 1. the stratum corneum (the outer layer), 2. the epidermis 3. the dermis • Blood capillaries and nerve fibers rise from the subcutaneous fat into the dermis and up to the epidermis. • Sebaceous glands, sweat glands, and hair follicles originating in the dermis and subcutaneous layers rise to the skin’s surface. • The stratum corneum is 10- to 15-μm thick layer of flat, partially desiccated, dead epidermal cells. • The stratum corneum is composed of approximately 40% protein (mainly keratin) and 40% water, with the balance being lipid, principally as triglycerides, free fatty acids, cholesterol, and phospholipids. • On the surface is a film of emulsified material composed of a complex mixture of sebum, sweat, and desquamating epidermal cells. • The stratum corneum, being keratinized tissue, behaves as a semipermeable artificial membrane, and drug molecules can penetrate by passive diffusion. • The rate of drug movement across this skin layer depends on the drug concentration in the vehicle, its aqueous solubility, and the oil–water partition coefficient between the stratum corneum and the product’s vehicle . • Substances with both aqueous and lipid solubility characteristics are good candidates for diffusion through the stratum corneum. • Once through the stratum corneum, drug molecules may pass through the deeper epidermal tissues and into the dermis. • If the drug reaches the vascularized dermal layer, it becomes available for absorption into the general circulation (transdermal delivery systems). • Hair follicles and gland ducts can provide entry for drug molecules, but because their relative surface area is so minute compared to the total epidermis, they are minor factors in drug absorption. • Differences in emollient and occlusive effects and ease of application and removal between products is a factor of the base used and product type. • oleaginous bases provide greater occlusion and emollient effects than do hydrophilic or waterwashable bases. • Pastes offer even greater occlusion and are more effective than ointments at absorbing serous discharge. • Creams, usually oil-in-water emulsions, spread more easily than ointments and are easier to remove. • Water-soluble bases are non-greasy and are easily removed. Use 1. before applying a dermatologic product, the patient should thoroughly clean the affected area with soap and water and dry by patting with a soft cloth. 2. In most instances, a thin layer of medication should be applied to the affected area and spread evenly using gentle pressure with the fingertips. 3. Typically, about 1 to 3 mg of ointment or cream is applied per square centimeter of skin. 4. Unless there is a specified need for an occlusive dressing to protect the area from excessive contact or contaminants, a bandage should not be used. examples of treatments appropriate to disorders of the various skin layers • Surface treatment: • mainly by using: 1.a simple cosmetic application, 2.forming a protective layer 3.attacking bacteria and fungi. • Some examples include protective films, sunscreens, and barriers that hinder moisture loss and so avert chapping( prevent cracks ). • For topical antibiotics, antiseptics and deodorants, the surface microorganisms are the target. • Then, effective surface bioavailability requires that the formulation should release the antimicrobial so it can penetrate the surface skin fissures and reach the organisms. Stratum corneum treatment: • The main therapies aimed at the horny layer improve emolliency by raising water content, or stimulate keratosis with, for example, salicylic acid. epidermis and dermis treatment: • Drug examples include topical steroidal and nonsteroidal anti-inflammatory agents; corticosteroids may also be used in psoriasis. • Antibiotics. • Anaesthetic drugs such as benzocaine. • antipruritics and antihistamines alleviate itch. examples of treatments appropriate to disorders of the various skin layers • Skin appendage treatment: • the sweat glands: with antiperspirants such as aluminium or other metal salts. • In acne we use topical exfolients such as salicylic acid, tretinoin (retinoic acid) or isotretinoin, and benzoyl peroxide and antibiotics such as erythromycin and Clindamycin. • Depilatories usually contain strontium or barium sulphides, or thioglycolates; FEATURES AND USE OF OPHTHALMIC OINTMENTS AND GELS FEATURES • The major route by which drugs enter the eye is simple diffusion via the cornea. Lipophilic drugs are more capable of penetration than hydrophilic compounds. • For drugs that are poorly absorbed by the cornea, the conjunctiva and sclera provide an alternate route. FEATURES • Compared with ophthalmic solutions, ophthalmic ointments and gels provide extended residence time on the surface of the eye, increasing the duration of their surface effects and bioavailability for absorption into the ocular tissues. • Medicinal agents are added to an ointment base either as a solution or as a finely micronized powder. FEATURES • The ointment base selected for an ophthalmic ointment must: 1. not be irritating to the eye 2. permit the diffusion of the medicinal substance throughout the secretions bathing the eye. 3.have a softening point close to body temperature, both for comfort and for drug release. FEATURES • Most often, mixtures of white petrolatum and liquid petrolatum (mineral oil) are used. • Sometimes a water-miscible agent such as lanolin is added. • A gel base of PEG and mineral oil is also used; this form permits water and water-insoluble drugs to be retained within the base. FEATURES • ophthalmic ointments must meet the USP sterility tests. • When an antimicrobial preservative is needed, among those used are methylparaben (0.05%) and propylparaben (0.01%) combinations, phenylmercuric acetate (0.0008%), chlorobutanol (0.5%), and benzalkonium chloride (0.008%). USE • the hands should be washed and dried thoroughly. • Then the ointment tube is held between the thumb and forefinger and the tip placed near the eyelid without touching it. • The patient’s head should be tilted back, and with the index finger of the opposite hand, the lower eyelid of the affected eye should be gently pulled downward. • The tip of the ointment tube should be held slightly above the inside portion of the sack between the lower eyelid and eyeball. • Without touching the tip to any part of the eye, a thin ribbon of ointment, approximately 0.25 to 0.5 in., should be placed along the inside of the lower lid. • The patient should face down and slowly close the eye for a few seconds. • Then any excess ointment should be wiped from the eyelids and lashes with a clean tissue. • After use, the ointment must be capped quickly and tightly. • The patient should be advised that blurred vision will occur as the ointment spreads over the eye and not to be alarmed. • If the ointment is to be administered only once daily, it is often preferable to do so at bedtime, when vision impairment will be inconsequential. • It is important to emphasize to the patient that ocular products if handled improperly can become contaminated by bacteria that cause ocular infections, which may lead to serious consequences. • Thus every effort must be made to avoid touching the tip of the tube to the eye, eyelid, fingertip, or any other surface, and the ointment should be used by only one person. FEATURES AND USE OF NASAL OINTMENTS AND GELS • Drugs introduced into the nasal passage are primarily for local effects on the mucous membranes and underlying tissues (e.g., nasal decongestants). • However, drug absorption to the general circulation does occur through the rich blood supply feeding the nasal lining. • The nasal route of administration is also used for the systemic absorption of a number of drugs. FEATURES AND USE OF RECTAL PREPARATIONS FEATURES AND USE OF RECTAL PREPARATIONS • Ointments, creams, and gels are used for topical application to the perianal area and for insertion within the anal canal. • They largely are used to treat local conditions of anorectal pruritus, inflammation, and the pain and discomfort associated with hemorrhoids. • Substances applied rectally may be absorbed by diffusion into the general circulation via the hemorrhoidal arteries and accompanying veins in the anal canal. (suppositories) • The bases used in anorectal ointments and creams include combinations of PEG 300 and 3350, emulsion cream bases using cetyl alcohol and cetyl esters wax, and white petrolatum and mineral oil. • When antimicrobial preservatives are required, methylparaben, propylparaben, benzyl alcohol, and butylated hydroxyanisole are frequently used. Rectal ointment with perforated inserter/ applicator tip. FEATURES AND USE OF VAGINAL PREPARATIONS FEATURES AND USE OF VAGINAL PREPARATIONS • Topical products are used to treat vulvovaginal infections, vaginitis, conditions of endometrial atrophy, and for contraception with spermatocidal agents. • Creams with water-washable bases are preferred to oleaginous ointments. • Although some preparations are applied externally to the vulva, most are intended to be delivered to the vagina by means of applicator tips that accompany the products. Vaginal cream with inserter.