Basics in Nursing Care Dr. Abdul-Monim Batiha Prepared By RN, DNSc
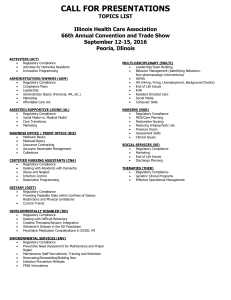
advertisement

Basics in Nursing Care Basics in Nursing Care Prepared By Dr. Abdul-Monim Batiha RN, DNSc Assistant professor of Critical Care Nursing 2010-2011 Unit 1 Introduction to nursing care Definitions of Nursing Definitions of nursing include nursing as caring, an art, a science, client centered, holistic, adaptive, a helping profession, and concerned with health promotion, maintenance, and restoration. The definition of nursing developed by the American Nurses Association has evolved over the years. The current definition states that “nursing is the protection, promotion, and Dr. Abdul-Monim Batiha Page 1 Basics in Nursing Care optimization of health and abilities, prevention of illness and injury, alleviation of suffering through the diagnosis and treatment of human response, and advocacy in the care of individuals, families, communities, and population.” Consumer , patient , and client are terms used to identify the recipients of nursing; however, many nurses use the term client since it emphasizes the responsibility of people for their own health. Discuss historical Back Ground influencing the development of nursing. Many nursing leaders have made contributions to nursing’s history and to women’s history. Florence Nightingale (1820–1910) was the founder of modern nursing. Clara Barton (1812–1912) helped establish the American Red Cross. Linda Richards (1841–1930) was the United States’ first trained nurse and is credited with pioneer work in psychiatric and industrial nursing. Mary Mahoney (1845–1926) was the United States’ first black professional nurse, and she worked for acceptance of blacks into nursing and the promotion of equal rights. Lillian Wald (1867–1940) was the founder of public health nursing and with Mary Brewster founded the Henry Street Settlement and Visiting Nurse Service. Dr. Abdul-Monim Batiha Page 2 Basics in Nursing Care Identify four major areas within the scope of nursing practice. 1. Four major areas within the scope of nursing practice are promoting health and wellness, preventing illness, restoring health, and caring for the dying. Promoting health and wellness involves behaviors that enhance quality of life and maximize personal potential by enhancing healthy lifestyles. The goal of illness prevention is to maintain optimal health by preventing disease. Restoring health includes providing direct care, performing diagnostic and assessment procedures, consulting with other health care professionals, and teaching and rehabilitating clients. Care of the dying involves comforting and caring for dying clients, assisting clients to live as comfortable as possible until death, and helping support persons cope with death. Identify Levels of Communication and discus interpersonal relationship Communication occurs at different levels, with each level influencing the others. Discussed below are the intrapersonal, the interpersonal, and group levels of communication. Dr. Abdul-Monim Batiha Page 3 Basics in Nursing Care Intrapersonal Level Intrapersonal communication is the messages one sends to oneself, including self-talk, or communication with oneself. A person receiving internal or external messages organizes, interprets, and assigns meaning to the messages. The result of this process is the individual’s unique way of perceiving. The message of the speaker may differ from that heard by the receiver because of the intrapersonal communication of each. Also, self-talk can interfere with attention to others and cause much to be missed during interpersonal exchanges. Interpersonal Level Interpersonal communication is the process that occurs between two people either in face-to-face encounters, over the telephone, or through other communication media. Interpersonal communication builds on the intrapersonal level in that each person communicating must communicate with the self in order to communicate with others. An important outcome of interpersonal communication is the development of an interpersonal relationship . Interpersonal skills are essential competencies for nurses. Describe the duties (roles) of nurses. Nurses assume a number of roles, often concurrently, while providing care to clients. These roles include caregiver, communicator, teacher, Dr. Abdul-Monim Batiha Page 4 Basics in Nursing Care client advocate, counselor, change agent, leader, manager, case manager, and research consumer. As caregivers, nurses perform activities that assist the client physically and psychologically. As communicators, nurses communicate with clients, support persons, other health care professionals, and people in the community. As educators, nurses educate clients about their health and health care procedures, teach unlicensed assistive personnel, and share expertise with other nurses and health care personnel. As client advocates, nurses act to protect clients. They represent clients’ needs and wishes to other health professionals and assist clients to exercise rights and speak up for themselves. As counselors, nurses provide emotional, intellectual, and psychological support to help clients recognize and cope with stressful psychological or social problems, develop improved interpersonal relationships, and promote personal growth. As change agents, nurses not only assist clients to make modifications in behavior but also act to make changes in the health care system. As leaders, nurses influence others to work together to accomplish specific goals whether working with individual clients, other health professionals, or community groups. Dr. Abdul-Monim Batiha Page 5 Basics in Nursing Care As managers, nurses manage care for individuals, families, and communities. They delegate nursing activities to ancillary personnel and other nurses, supervising and evaluating their performance. As case managers, nurses work with multidisciplinary health care teams to measure effectiveness of case management plans and to monitor outcomes. As research consumers, nurses are aware of the process of research, are sensitive to protection of the rights of human subjects, participate in the identification of researchable problems, and discriminately use research findings to improve client care. Dr. Abdul-Monim Batiha Page 6 Basics in Nursing Care Unit 2 Management of some of the nursing processes Vital Signs Base line vital signs * Introduction:Vital signs are an important element of the assessment process, they are indictors of the patients present condition , baseline vital signs includes: 1- Respiration. Dr. Abdul-Monim Batiha Page 7 Basics in Nursing Care 234- Pulse. Blood pressure. Body temperature. Other key indications of the patient’s respiratory, cardiovascular and central nervous system are:1. Capillary refill 2. Papillary reaction 3. Level of consciousness 1- Body temperature:It reflect the balance between the heat produced and the lost from the body, the average body temp of an adult is between ( 36.7-37c) . There are four common sites for measuring body temperature. a. Oral route:- Most accessible and convenient and contra indicated for 1. Children under 6 yrs of age 2. For patients who are confused 3. For patients who have convulsive disorders 4. For patients following oral surgery. b. Rectal route:- most reliable (accurate). Contra indicated following: 1rectal surgery. 2newborn babies. 3patient with diarrhea. c. Axillary route:- Safest and non invasive d. Tympanic route:- Readily accessible very fast. Dr. Abdul-Monim Batiha Page 8 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 9 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 10 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 11 Basics in Nursing Care 2- Respiration: Breathing is continuous process in which each breath regularly follows the last with no notable interruption, else it is normally spontaneous automatic process that occurs with out conscious thought, visible effort , marked sounds or pain, you will assess breathing by watching the patient’s chest rise and fall, you must determine the:1. Rate:Are determined by counting the number of breath per a minute normal respiratory rate varies according to age. Newborn 30-60c/m 2 yrs 20-30 c/m 6 yrs 18-26 c/m Adult 12-20 c/m 2. quality :see the table below (characteristics of respiration): Normal Shallow Noisy wheezing 3. 4. 3- characteristics of respiration Breathing is neither shallow nor deep Average chest wall motion No use of accessory muscles Slight chest or abdominal wall motion Labored Increased breathing effort Grunting, stridor Use of accessory muscles possible gasping Nasal flaring, supraclavicular and intercostals retractions in infants and children Increase in sound of breathing, including snoring, Rhythm:- regular or irregular. Depth :- shallow Pulse A wave of blood created by contraction of the left ventricles of the heart, the heart is pulsating pump and the blood enter the arteries with the heart beat causing pulse wave. You must assess the rate, strength and regularity of the pulse. Dr. Abdul-Monim Batiha Page 12 Basics in Nursing Care Blood pressure Arterial blood pressure is define as a measure or the pressure exerted by the blood as it flows through the arteries there are 2 blood pressure measures:1. Systolic pressure:- Is the pressure of the blood as a result of contraction of the ventricles. 2. Diastolic pressure:- Is the pressure when the ventricles are at rest. The average blood pressure of a healthy adult is 120/80 mm Hg. Hypertension:- is abnormally high blood pressure over 140 mm Hg systolic and 90 mm Hg diastolic. Hypotension:- Is abnormally low blood pressure below 100 mm Hg systolic and 60 mm Hg diastolic. Dr. Abdul-Monim Batiha Page 13 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 14 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 15 Basics in Nursing Care Types of Thermometers • Electronic • Chemical disposable • Infrared (tympanic) • Scanning infrared (temporal artery) • Temperature-sensitive tape • Glass mercury Dr. Abdul-Monim Batiha Page 16 Basics in Nursing Care Pulse Sites A pulse may be measured in nine sites (Temporal. Carotid. Apical. Femoral. Brachial. Redial. Popliteal. Posterior tibial. Dorsalis pedis). When assessing the pulse, the nurse collects the following data: Tachycardia. An excessively fast heart rate over 100 BPM in adult is referred to as tachycardia. Bradycardia. A heart rate in an adult of 60 BPM or less is called. The pulse rhythm. Is the pattern of the beats and the intervals between the beats. Equal time elapses between beats of a normal pulse. A pulse with an irregular rhythm is referred to as a dysrhythmia or arrhythmia. Dr. Abdul-Monim Batiha Page 17 Basics in Nursing Care Pulse volume, also called the pulse strength or amplitude, refers to the force of blood with each beat. The elasticity of the arterial wall reflects its expansibility or its deformities. A healthy, normal artery feels straight, smooth, soft, pliable. Respirations Respiration is the act of breathing. External respiration refers to the interchange of oxygen and carbon dioxide between the alveoli of the lungs and pulmonary blood. Internal respiration, by contrast, takes place throughout the body; it is the interchange of these same gases between the circulating blood and the cells of the body tissues. Inhalation or inspiration refers to the intake of air into the lungs. Exhalation or expiration refers to breathing out or the movement of gases from the lungs to the atmosphere. Ventilation is also used to refer to the movement of air in and out of the lungs. Altered Breathing Patterns and Sounds 1. Breathing Patterns Rate Tachypnea -----quick, shallow breaths. Bradypnea------abnormally slow breathing. Apnea-------------cessation of breathing. Dr. Abdul-Monim Batiha Page 18 Basics in Nursing Care Volume Hyperventilation------overexpansion of the lungs characterized by rapid and deep breath. Hypoventilation-------under-expansion of the lungs, characterized by shallow respirations. Ease or Effort Dyspnea -----difficult and labored breathing during which the individual has a persistent, unsatisfied need for air and feels distressed. Orthopnea-------ability to breathe only in upright sitting or standing positions Blood Pressure Blood pressure Arterial blood pressure is a measure of the pressure exerted by the blood as it flows through the arteries. Because the blood move in waves. There are two blood pressure: Systolic pressure, which is the pressure of the blood as a result of contraction of the ventricles, that is, the pressure of the height of the blood wave. Diastolic pressure, which is the pressure when the ventricles are at rest. Diastolic pressure is the lower pressure, present at all times within the arteries. Pulse pressure, the difference between the diastolic and the systolic pressures. Dr. Abdul-Monim Batiha Page 19 Basics in Nursing Care Blood pressure is measured in millimeters of mercury (mmHg) and recorded as a fraction. The systolic pressure is written over the diastolic pressure. The average blood pressure of a healthy adult is 120/80 mm Hg. Factors Affecting Blood Pressure Age : Newborns have a mean systolic pressure of about 75 mm Hg. The pressure rises with age, reaching a peak at the onset of puberty, and then tends to decline somewhat. Exercise: Physical activity increases the cardiac output and hence the blood pressure, thus 20 to 30 minutes of rest following exercise is indicated before the resting blood pressure can be reliably assessed. Stress: Stimulation of the sympathetic nervous system increases cardiac output and vasoconstriction of the arterioles, thus increasing the blood pressure reading. However, severe pain can decrease blood pressure greatly by inhibiting the vasomotor center and producing vasodilatation. Race: African American males over 35 years have higher blood pressure than European American males of the same age. Gender: After puberty, females usually have lower blood pressure than males of the same age this difference is thought to be due to hormonal variations. After menopause women generally have higher blood pressure than before. Medication: Many medications may increase or decrease the blood pressure. Obesity: Both childhood and adult obesity predispose to hypertension. Dr. Abdul-Monim Batiha Page 20 Basics in Nursing Care Diurnal variations: Pressure is usually lowest early in the morning, when the metabolic rate is lowest, then rises throughout the day and peaks in the late afternoon or early evening. Disease process: Any condition affecting the cardiac output blood volume, blood viscosity and/or compliance of the arteries has a direct effect on the blood pressure. Hypertension: A blood pressure that is persistently above normal. Primary hypertension an elevated blood pressure of unknown cause Secondary hypertension an elevated blood pressure of known cause. Hypotension is a blood pressure that is below normal. Orthostatic hypotension is a blood pressure that falls when the client sits or stands. Common Errors in Assessing Blood Pressure Bladder cuff too narrow Dr. Abdul-Monim Batiha Page 21 Basics in Nursing Care Bladder cuff too wide Arm unsupported Insufficient rest before the assessment. Repeating assessment too quickly. Deflating cuff too quickly. Deflating cuff too slowly. Failure to use the same arm consistently. Arm above level of the heart. Assessing immediately after a meal or smoker or has pain. Variations in Normal Vital Signs by Age Age Newborns Oral temperature in degree 36.8 Pulse Average and Ranges 130 (80- Respirations Average and Ranges 35(30-80) Blood pressure (mm Hg) 73/55 180) 1 year 36.8 120 (80- 30 (20-40) 90/55 (75- 20 (15-25) 95/57 140) 5-8 years 37 100 120) 10 years 37 70 (50-90) 19 (15-25) 102/62 Teen 37 75 (50-90) 18 15-20) 120/80 Adult 37 80 (60-100) 16 (12-20) 120/80 Older adult (>70 years) 37 70 (60-100) 16 (15-20) Possible increased diastolic Dr. Abdul-Monim Batiha Page 22 Basics in Nursing Care Injections Identify physiologic factors and individual variables affecting medication action. 1Factors Affecting Medication Action Developmental Gender Cultural, ethnic, and genetic Diet Environment Psychologic Illness and disease Time of administration 1. Medication action may be affected by developmental factors, gender, culture, ethnicity, genetics, diet, environment, psychologic factors, illness and disease, and time of administration. The nurse needs to be aware of developmental factors. Pregnant Dr. Abdul-Monim Batiha Page 23 Basics in Nursing Care women must be careful about taking medications, especially in the first trimester, because of the possible adverse effects on the fetus. Infants usually require smaller doses because of their body size and the immaturity of their organs. Older adults have different responses to medications due to physiologic changes that accompany aging and because they may be prescribed multiple drugs and incompatibilities may occur. Gender differences in medication action are chiefly related to the distribution of body fat and fluid and hormonal differences. In addition, most research studies on medications have been done on men. In addition to gender, a client’s response to drugs is also influenced by genetic variations such as size and body composition (pharmacogenetics). Ethnopharmacology is the study of the effects of ethnicity on response to prescribed medications. Cultural factors and practices (values and beliefs) can also affect a drug’s action; for example, an herbal remedy may speed up or slow down the metabolism of certain drugs (see Culturally Competent Care). The diet may contain nutrients that can interact with medications and increase or decrease action. It is important to consider the effects of a drug in the context of the client’s personality, milieu, and environmental conditions (e.g., temperature, noise). Psychologic factors, such as a client’s expectations about what a drug can do, can affect the response to the medication. Dr. Abdul-Monim Batiha Page 24 Basics in Nursing Care Illness and disease can affect how a client responds to a medication. For example, aspirin can reduce body temperature of a feverish client but has no effect on body temperature of a client without a fever. Time of administration is important because medications are absorbed more quickly if the stomach is empty; however, some medications irritate the gastrointestinal tract and are given after a meal. Describe various routes of medication administration. 1 Routes of Medication Administration Oral (PO) Sublingual (SL) Buccal Parenteral o Subcutaneous (SC) o Intramuscular (IM) o Intradermal (ID) o Intravenous (IV) o Intra-arterial (IA) o Intracardiac (IC) o Intraosseous (IO) o Intrathecal (intraspinal) (IT) (IS) o Epidural (ED) o Intra-articular 2 Topical Dr. Abdul-Monim Batiha Page 25 Basics in Nursing Care Dermatological Instillations and irrigations Inhalation Ophthalmic, otic, nasal, rectal, and vaginal 1.Routes of medication administration include oral, sublingual, buccal, parenteral, and topical. In oral administration the drug is swallowed. It is the most common, least expensive, and most convenient route for most clients. In sublingual administration a drug is placed under the tongue, where it dissolves. Buccal means “pertaining to the cheek.” In buccal administration a medication is held in the mouth against the mucous membranes of the cheek until the drug dissolves. The parenteral route is defined as other than the alimentary or respiratory tract. Some common routes for parenteral administration include subcutaneous (hypodermic), into the subcutaneous tissue just below the skin; intramuscular, into the muscle; intradermal, under the epidermis (into the dermis); intravenous, into a vein; intra-arterial, into an artery; intracardiac, into the heart muscle; intraosseous, into the bone; intrathecal or intraspinal, into the spinal canal; epidural, into the epidural space; and intra-articular, into a joint. Dr. Abdul-Monim Batiha Page 26 Basics in Nursing Care 2. Topical applications are those applied to a circumscribed surface area of the body. Routes for topical applications include dermatologic, applied to the skin; instillations and irrigations, applied into body cavities or orifices such as the urinary bladder, eyes, ears, nose, rectum, or vagina; ophthalmic, otic, nasal, rectal, and vaginal topical preparations; and inhalations, administered into the respiratory system by a nebulizer or positive Dr. Abdul-Monim Batiha pressure breathing apparatus. Page 27 Basics in Nursing Care Identify essential parts of a medication order. 1Parts of a Medication Order Full name of the client Date and time the order written Name of drug to be administered Dosage Frequency of administration Route of administration Signature of person writing the order List examples of various types of medication orders. 1Types of Medication Orders and Examples Stat order o Single order o Demerol 100 mg IM stat Seconal 100 mg hs before surgery Standing order o Multivitamin 1 capsule po daily o Demerol 100 mg IM q 4 h x 5 days prn order o Amphojel 15 mL prn - There are four common medication orders: stat order, single order, standing order, and prn order. A stat order indicates that the medication is to be given immediately and Dr. Abdul-Monim Batiha Page 28 Basics in Nursing Care only once (e.g., Demerol 100 mg IM stat). The single order or one-time order is for medication to be given once at a specified time (e.g., Seconal 100 mg hs before surgery). The standing order may or may not have a termination date, may be carried out indefinitely (e.g., multiple vitamins daily) until an order is written to cancel it, or may be carried out for a specified number of days (e.g., Demerol 100 mg IM q4h × 5 days). A prn order or as-needed order permits the nurse to give a medication when, in the nurse’s judgment, the client requires it (e.g., Amphojel 15 mL prn). List six essential steps to follow when administering medication. 1Six Essential Steps for Administering Medications Identify the client Inform the client Administer the drug Provide adjunctive interventions as indicated Record the drug administered Evaluate the client’s response to the drug 1. When administering any drug, regardless of the route of administration, the nurse must identify the client, inform the client, administer the drug, provide adjunctive interventions as indicated, record the drug administered, and evaluate the client’s response to the drug. Dr. Abdul-Monim Batiha Page 29 Basics in Nursing Care JCAHO’s National Patient Safety Goals require a nurse to use at least two client identifiers whenever administering medications. Acceptable identifiers may be the person’s name, an assigned identification number, a telephone number, a photograph, or another personal identifier. If the client is unfamiliar with the medication, the nurse should explain the intended action as well as any side effects or adverse reactions that might occur. It is also very important to listen to the client. Before administering the drug, the nurse should read the medication administration record (MAR) carefully and perform three checks with the labeled medication (See Box 35–3). In addition the ten “rights” of medication administration must be observed (See Box 35–4). Dr. Abdul-Monim Batiha Page 30 Basics in Nursing Care The nurse should provide adjunctive interventions as indicated. Clients may require physical assistance in assuming positions for parenteral medications or may need guidance about measures to enhance drug effectiveness and prevent complications. The nurse must record the drug administered, following agency regulations. In order to evaluate the client’s response to the drug, the nurse should Dr. Abdul-Monim Batiha Page 31 Basics in Nursing Care know the kinds of behavior that reflect the action or lack of action of the drug and its untoward effects (both minor and major) for each medication the client is receiving. The nurse may also report the client’s response directly to the nurse manager and primary care provider. State the “rights” to accurate medication administration. 1Ten “Rights” of Accurate Medication Administration Right medication (Drug) Right dose Right time Right route Right client Right documentation Right client education Right to refuse Right assessment Right evaluation (See Box 35–4). Dr. Abdul-Monim Batiha Page 32 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 33 Basics in Nursing Care Identify equipment required for parenteral medications. 1 Parenteral Medications Common nursing procedure Absorbed more quickly than oral Requires careful and accurate administration Aseptic technique 2 Syringes Parts o Ruber plunger Tip o Barrel o Plunger 3 Types of Syringes Standard hypodermic syringe Insulin syringe Tuberculin syringe Disposable prefilled unit-dose or prefilled cartridges Dr. Abdul-Monim Batiha Page 34 Basics in Nursing Care 4 Needles Stainless steel Most disposable Parts o Hub o Cannula or shaft o Bevel 5 Characteristics of Needles Slant or length of the bevel Length of the shaft Gauge Dr. Abdul-Monim Batiha Page 35 Basics in Nursing Care To administer parenteral medications, nurses use syringes and needles to withdraw medications from ampules and vials. Syringes have three parts: the tip, the barrel, and the plunger. There are several kinds of syringes, differing in size, shape, and material. The three most commonly used types are the standard hypodermic syringe, the insulin syringe, and the tuberculin syringe. Injectable medications are frequently supplied in disposable prefilled unit-dose systems available as a prefilled syringe ready for use or prefilled sterile cartridges and needles that require attachment to a reusable holder. Needleless systems are also available. Needles are made of stainless steel, and most are disposable. A needle has three parts: the hub, the cannula or shaft, and the bevel. Needles used for injections have three variable characteristics: the slant or length of the bevel, the length of the shaft, and the gauge. Dr. Abdul-Monim Batiha Page 36 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 37 Basics in Nursing Care List the most common apprivation used in medications orders. Identify Guidelines for Safe Administration of Medications. Guidelines for Safe Administration of Medications Dr. Abdul-Monim Batiha Page 38 Basics in Nursing Care • Never administer medications that are prepared by another nurse. You are responsible for a medication error if you administer a medication that was inaccurately prepared by another nurse. • Nurses should listen carefully to the client who questions the addition or deletion of a medication. Most clients are aware of their prescribed medications. If a client questions the drug or dose you are preparing to administer, recheck the order. • If a medication is withheld, indicate the exact reason why in the client’s record. Legally you are accountable for giving ordered medications to the client; however, circumstances may prevent you from giving a medication as ordered. Medications may be held for some diagnostic tests, or the client receiving antihypertensive medications may have a blood pressure that is lower than normal. If you gave the antihypertensive, the blood pressure would decrease, causing further hypotension. • Do not leave medications at the client’s bedside for any reason. The client may forget to take the medication, medications can accumulate, and the client could take two or more of the same medication, causing an overdose, or another client who is confused could take the medicine. Do not leave medications at the client’s bedside for any reason. The client may forget to take the medication, medications can accumulate, and the client could take two or more of the same medication, causing an overdose, or another client who is confused could take the medicine. Dr. Abdul-Monim Batiha Page 39 Basics in Nursing Care Ampules and Vials Drugs for parenteral injections are sterile preparations. Drugs that deteriorate in solution are dispensed as tablets or powders and dissolved in a solution immediately before injection. Drugs that remain stable in a solution are dispensed in ampules and vials in an aqueous or oily solution or suspension. Ampules are glass containers of single-dose drugs (Figure 29-13). The glass container has a constriction in the stem to facilitate opening the ampule. Dr. Abdul-Monim Batiha Page 40 Basics in Nursing Care Determine angle and site of injections. Angle of Injection The angle of insertion depends on the type of injection. Figure 29-18 illustrates the angle of insertion for each type of parenteral injection. . Intradermal Injection Sites: A. Inner Aspect of the Forearm; B. Upper Chest; C. Upper Back Dr. Abdul-Monim Batiha Page 41 Basics in Nursing Care Subcutaneous Injection Sites: A. Abdomen; B. Lateral and Anterior Aspects of Upper Arm and Thigh; C. Scapular Area on Back; D. Upper Ventrodorsal Gluteal Area. Dr. Abdul-Monim Batiha Page 42 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 43 Basics in Nursing Care Dr. Abdul-Monim Batiha Page 44 Basics in Nursing Care Identify how to calculation of flow rate. Calculation of Flow Rate The flow rate is the volume of fluid to infuse over a set period of time as prescribed by the health care practitioner. The health care practitioner will identify either the amount to infuse per hour (such as 125 ml per hour or 1000 ml over an 8-hour period). Calculate the hourly infusion rate as follows: Dr. Abdul-Monim Batiha Page 45 Basics in Nursing Care Skill: Administering a Subcutaneous Injection Preparation 1. Assess: • Allergies to medication. • Specific drug action, side effects, and adverse reactions. • Client’s knowledge and learning needs about the medication. • Status and appearance of subcutaneous site for lesions, erythema, swelling, ecchymosis, inflammation, and tissue damage from previous injections. • Ability of the client to cooperate during the injection. • Previous injection sites used. 2. Assemble equipment: • MAR or computer printout • Vial or ampule of the correct sterile medication • Syringe and needle • Antiseptic swabs • Dry, sterile gauze for opening an ampule (optional) • Clean gloves Check the MAR. Check the label on the medication carefully against the MAR to make sure that the correct medication is being prepared. 3. Perfo rmed YNo e s Mastered Comments Follow the three checks for administering medications. Read the label on the medication: • When it is taken from the medication cart • Before withdrawing the medication • After withdrawing the medication. 4. Organize the equipment. Procedure 1. Perform hand hygiene and observe other appropriate infection control procedures. 2. Prepare the medication from the ampule or vial for drug withdrawal. Dr. Abdul-Monim Batiha Page 46 Basics in Nursing Care 3. 4. 5. 6. 7. 8. Provide for client privacy. Prepare the client. Introduce yourself and verify the client’s identity. Assist the client to a position in which the arm, leg, or abdomen can be relaxed, depending on the site to be used. Obtain assistance in holding an uncooperative client. Explain the purpose of the medication and how it will help, using language that the client can understand. Include relevant information about effects of the medication. Select and clean the site. Select a site free of tenderness, hardness, swelling, scarring, itching, burning, and localized inflammation. Select a site that has not been used frequently. Put on clean gloves. As agency protocol indicates, clean the site with an antiseptic swab. Start at the center of the site and clean in a widening circle to approximately 5 cm (2 inches). Allow the area to dry thoroughly. Place and hold the swab between the third and fourth fingers of the nondominant hand, or position the swab on the client’s skin above the intended site. Prepare the syringe for injection. Remove the needle cap while waiting for the antiseptic to dry. Pull the cap straight off to avoid contaminating the needle by the outside edge of the cap. Dispose of the needle cap. Inject the medication. Grasp the syringe in your dominant hand by holding it between your thumb and fingers. With palm facing to the side or upward for a 45-degree angle insertion, or with the palm downward for a 90-degree angle insertion, prepare to inject. Dr. Abdul-Monim Batiha Page 47 Basics in Nursing Care Using the nondominant hand, pinch or spread the skin at the site, and insert the needle, using the dominant hand and a firm, steady push. When the needle is inserted, move your nondominant hand to the end of the plunger. 9. 10. 11. 12. Inject the medication by holding the syringe steady and depressing the plunger with slow, even pressure. With many subcutaneous injections, the needle should be imbedded within the skin for five seconds after complete depression of plunger to ensure complete delivery of the dose. Remove the needle. Remove the needle slowly and smoothly, pulling along the line of insertion while depressing the skin with your nondominant hand. If bleeding occurs, apply pressure to the site with dry, sterile gauze until it stops. Dispose of supplies appropriately. Activate the needle safety device or discard the uncapped needle and attached syringe into designated receptacles. Remove gloves. Perform hand hygiene. Document all relevant information. Document the medication given, dosage, time, route, and any assessments. Many agencies prefer that medication administration be recorded on the medication record. Assess the effectiveness of the medication at the time it is expected to act. Variation: Administering a Heparin Injection Procedure Select a site on the abdomen away from the umbilicus and above the level of the iliac crests. Dr. Abdul-Monim Batiha Page 48 Basics in Nursing Care Use a ⅜-inch, 25- or 26-gauge needle, and insert it at a 90-degree angle. If a client is very lean or wasted, use a needle longer than ⅜-inch, and insert it at a 45-degree angle. The arms or thighs may be used as alternate sites. Do not aspirate when giving heparin by subcutaneous injection. Do not massage the site after the injection. Alternate the sites of subsequent injections. Skill: Administering an Intradermal Injection Performed Preparation 1. 2. 3. Yes No Mastered Comments Assess: • Appearance of the injection site. • Specific drug action and the expected response. • Client’s knowledge of drug action and response. • Check agency protocol about sites to use for skin tests. Assemble equipment and supplies: • Vial or ampule of the correct medication • Sterile 1-mL syringe calibrated into hundredths of a milliliter (i.e., tuberculin syringe) and a 25- to 27-gauge needle that is ¼– ⅝ inch long • Alcohol swabs • 2 x 2 sterile gauze square (optional) • Clean gloves (according to agency protocol) • Band-Aid (optional) • Epinephrine Check the MAR. Dr. Abdul-Monim Batiha Page 49 Basics in Nursing Care 4. Check the label on the medication carefully against the MAR to make sure that the correct medication is being prepared. Follow the three checks for administering medications. Read the label on the medication: • When it is taken from the medication cart • Before withdrawing the medication • After withdrawing the medication Organize the equipment. Procedure 1. 2. 3. 4. 5. 6. 7. 8. Perform hand hygiene and observe other appropriate infection control procedures. Prepare the medication from the vial or ampule for drug withdrawal. Prepare the client. Explain to the client that the medication will produce a small wheal, sometimes called a bleb. Provide for client privacy. Select and clean the site. Select a site. Avoid using sites that are tender, inflamed, or swollen, and those that have lesions. Put on gloves as indicated by agency policy. Cleanse the skin at the site using a firm, circular motion, starting at the center and widening the circle outward. Allow the area to dry thoroughly. Prepare the syringe for the injection. Remove the needle cap while waiting for the antiseptic to dry. Expel any air bubbles from the syringe. Grasp the syringe in your dominant hand, holding it between thumb and forefinger. Hold the needle almost parallel to the skin surface, with the bevel of the needle up. Inject the fluid. With the nondominant hand, pull the skin at the site until it is taut. Dr. Abdul-Monim Batiha Page 50 Basics in Nursing Care 9. Insert the tip of the needle far enough to place the bevel through the epidermis into the dermis. The outline of the bevel should be visible under the skin surface. Stabilize the syringe and needle, and inject the medication carefully and slowly, so that it produces a small wheal on the skin. Withdraw the needle quickly at the same angle at which it was inserted. Activate the needle safety device. Apply a Band-Aid, if indicated. Do not massage the area. Dispose of the syringe and needle in the sharps container. Remove your gloves. Circle the injection site with ink to observe for redness or induration per agency policy. Document all relevant information. Record the testing material given, the time, dosage, route, site, and nursing assessments. Skill: Administering an Intramuscular Injection Performed Preparation 1. 2. Yes No Mastered Comments Assess: • Client allergies to medications. • Specific drug action, side effects, and adverse reactions. • Client’s knowledge of and learning needs about the medication. • Tissue integrity of the selected site. • Client’s age and weight, to determine site and needle size. • Client’s ability or willingness to cooperate. Determine: • Whether the size of the muscle is appropriate to the amount of medication to be injected. Dr. Abdul-Monim Batiha Page 51 Basics in Nursing Care 3. 4. 5. Assemble equipment and supplies: • MAR or computer printout • Sterile medication (usually provided in an ampule or vial) • Syringe and needle of a size appropriate for the amount of solution to be administered • Antiseptic swabs • Clean gloves Check the MAR. Check the label on the medication carefully against the MAR to make sure that the correct medication is being prepared. Follow the “three checks” for administering the medication and dose. Read the label on the medication: • When it is taken from the medication cart • Before withdrawing the medication • After withdrawing the medication. Confirm that the dose is correct. Organize the equipment. Procedure 1. 2. 3. 4. Perform hand hygiene and observe other appropriate infection control procedures. Prepare the medication from the ampule or vial for drug withdrawal. Whenever feasible, change the needle on the syringe before the injection. Invert the syringe needle uppermost, and expel all excess air. Provide for client privacy. Prepare the client. Check the client’s identification band. Assist the client to a supine, lateral, prone, or sitting position, depending on the chosen site. Obtain assistance in holding an uncooperative client. Dr. Abdul-Monim Batiha Page 52 Basics in Nursing Care 5. 6. 7. 8. Explain the purpose of the medication and how it will help, using language that the client can understand. Include relevant information about effects of the medication. Select, locate, and clean the site. Select a site free of skin lesions, tenderness, swelling, hardness, or localized inflammation, and one that has not been used frequently. If injections are to be frequent, alternate sites. Avoid using the same site twice in a row. Locate the exact site for the injection. Put on clean gloves. Clean the site with an antiseptic swab. Using a circular motion, start at the center and move outward about 5 cm (2 inches). Transfer and hold the swab between the third and fourth fingers of your nondominant hand in readiness for needle withdrawal, or position the swab on the client’s skin above the intended site. Allow the skin to dry prior to injecting medication. Prepare the syringe for injection. Remove the needle cover and discard without contaminating the needle. If using a prefilled unit–dose medication, take caution to avoid dripping medication on the needle prior to injection. If this does occur, wipe the medication off the needle with sterile gauze. Inject the medication using a Z-track technique. Use the ulnar side of the nondominant hand to pull the skin approximately 2.5 cm (1 inch) to the side. Holding the syringe between the thumb and forefinger, pierce the skin quickly and smoothly at a 90-degree angle, and insert the needle into the muscle. Dr. Abdul-Monim Batiha Page 53 Basics in Nursing Care 9. 10. 11. 12. Hold the barrel of the syringe steady with your nondominant hand, and aspirate by pulling back on the plunger with your dominant hand. Aspirate for 5–10 seconds. If blood appears in the syringe, withdraw the needle, discard the syringe, and prepare a new injection. If blood does not appear, inject the medication steadily and slowly (approximately 10 seconds per milliliter) while holding the syringe steady. After injection, wait 10 seconds. Withdraw the needle. Withdraw the needle smoothly at the same angle of insertion. Release the skin. Apply gentle pressure at the site with a dry sponge. If bleeding occurs, apply pressure with a dry, sterile gauze until it stops. Activate the needle device or discard the uncapped needle and attached syringe into the proper receptacle. Remove gloves. Perform hand hygiene. Document all relevant information. Include the time of administration, drug name, dose, route, and the client’s reactions. Assess effectiveness of the medication at the time it is expected to act. Dr. Abdul-Monim Batiha Page 54 Basics in Nursing Care Unit 3 Patient Care Preoperative care &preparation for anesthesia Discuss various types of surgery according to degree of urgency, degree of risk, and purpose. 1 Various types of surgery Degree of urgency o Emergency o Elective o Major o Minor Degree of risk Purposes of surgical procedures Dr. Abdul-Monim Batiha o Diagnostic o Palliative o Ablative o Constructive o Transplant Page 55 Basics in Nursing Care 1. Surgery is classified by its urgency and necessity to preserve the client’s life, body part, or body function. Emergency surgery is performed immediately to preserve function or the life of the client (for example, to control internal hemorrhage). Elective surgery is performed when surgical intervention is the preferred treatment for a condition that is not immediately life threatening, but may ultimately threaten life or well-being, or to improve the client’s life (for example, hip replacement surgery). Surgery is also classified as major or minor according to the degree of risk to the client. Major surgery involves a high degree of risk. It may be complicated or prolonged, large losses of blood may occur, vital organs may be involved, or postoperative complications may be likely (for example, open heart surgery). Minor surgery normally involves little risk, produces few complications, and is often performed on an outpatient basis (for example, breast biopsy). Surgical procedures have various purposes. A diagnostic procedure confirms or establishes a diagnosis (for example, breast biopsy). A palliative procedure relieves or reduces pain or symptoms of a disease; it does not cure (for example, resection of nerve roots). An ablative procedure removes a diseased body part (for example, removal of gallbladder). A constructive procedure restores function or appearance that has been lost or reduced (for example, breast implant). A transplant replaces malfunctioning structures (for example, kidney replacement). Dr. Abdul-Monim Batiha Page 56 Basics in Nursing Care Describe the phases of the perioperative period. Surgery is a unique experience of a planned physical alteration encompassing three phases: preoperative, intraoperative, and postoperative. The preoperative phase begins when the decision to have surgery is made and ends when the client is transferred to the operating table. The nursing activities associated with this phase include assessing the client, identifying potential or actual health problems, planning specific care based on the individual’s needs, and providing preoperative teaching for the client, the family, and significant others. The intraoperative phase begins when the client is transferred to the operating table and ends when the client is admitted to the postanesthesia care unit (PAC). The nursing activities related to this phase include a variety of specialized procedures designed to create and maintain a safe therapeutic environment for the client and the health care personnel. The activities include providing for the client’s safety, maintaining an aseptic environment, ensuring proper functioning of equipment, and providing the surgical team with the instruments and supplies needed during the operation. The postoperative phase begins with the admission of the client to the postanesthesia area and ends when healing is complete. During the postoperative phase, nursing activities include assessing the client’s response (physiologic and psychologic) to surgery, performing interventions to Dr. Abdul-Monim Batiha Page 57 Basics in Nursing Care facilitate healing and prevent complications, teaching, providing support to the client and support people, and planning for home care. Identify essential aspects of preoperative assessment. 1. Preoperative assessment includes collecting and reviewing physical, psychological, and social client data to determine the client’s needs throughout the three preoperative phases. Preoperative assessment data include current health status, allergies, medications, previous surgeries, mental status, understanding of the surgical procedure and anesthesia, smoking, alcohol and other mind-altering substances, coping, social resources, and cultural and spiritual considerations 2. A brief but complete physical assessment pays particular attention to systems that could affect the client’s response to anesthesia and surgery. It also includes a brief “mini” mental status. Respiratory, cardiovascular, and other systems (gastrointestinal, genitourinary, and musculoskeletal) are examined to provide baseline data. The surgeon and/or anesthesiologist orders preoperative diagnostic tests. The nurse’s responsibility is to check the orders carefully to see that they are carried out and to ensure that the results are obtained and in the client’s record prior to surgery. Table 37–2 lists routine preoperative screening tests. In addition to these tests, diagnostic tests directly relating to the client’s disease are performed. Dr. Abdul-Monim Batiha Page 58 Basics in Nursing Care Identify nursing responsibilities in planning perioperative nursing care. 1. The overall goal in the preoperative period is to ensure that the client is mentally and physically prepared for surgery. Planning should involve the client, the client’s family, and significant others. Examples of nursing activities to achieve these goals include preoperative teaching (covered in outcome 6), physical preparation (covered in outcome 7), and psychological preparation. For the perioperative client, discharge planning begins before admission. Early planning to meet the discharge needs of the client is particularly important for outpatient procedures as the client is generally discharged within hours after the procedure is performed. Discharge planning incorporates an assessment of the client’s, family’s, and significant others’ abilities and resources for care, their financial resources, and the need for referrals and home health services. (See Home Care Considerations: Postoperative Instructions.) 2. The overall goals of care in the intraoperative period are to maintain the client’s safety and to maintain homeostasis. Examples of nursing activities to achieve these goals include positioning the client appropriately; performing preoperative skin preparation; assisting in preparing and maintaining the sterile field; opening and dispensing sterile supplies during surgery; providing medications and solutions for the sterile field; monitoring Dr. Abdul-Monim Batiha Page 59 Basics in Nursing Care and maintaining a safe, aseptic environment; managing catheters, tubes, drains, and specimens; performing sponge, sharp, and instrument counts; and documenting nursing care provided and the client’s response to interventions. 3. Overall goals in postoperative period include promotion of comfort and healing; restoration of the highest possible level of wellness; and prevention of associated risks. Postoperative care planning and discharge planning begin in the preoperative phase when preoperative teaching is implemented. To plan for continuity of care for the surgical client after discharge, the nurse considers the client’s needs for assistance with care in the home setting and incorporates an assessment of the client’s and family’s abilities for self-care, financial resources, and the need for referrals and home health services. (See Home Care Assessment: Surgical Clients.) Describe essential preoperative teaching, including pain control, moving, leg exercises, and coughing and deep-breathing exercises. 1. Four dimensions of preoperative teaching have been identified as important to clients: information including what will happen to the client, when it will happen, and what the client will experience, such as expected sensations and discomfort; psychological support to reduce anxiety; roles of the client and support people in preoperative preparation, during the surgical procedure, and during the postoperative period; and skills training such as moving, deep breathing, coughing, splinting incisions with the hands or pillow, and using an incentive spirometer. Dr. Abdul-Monim Batiha Page 60 Basics in Nursing Care Preoperative teaching includes instruction about preoperative and 2. postoperative regimens. Preoperative regimen teaching includes: need for preoperative testing; discuss bowel preparation if necessary, skin preparation, preoperative medications, specific preoperative therapies, visit by anesthetist, need to restrict food and fluids, general timetable of events, need to remove jewelry, makeup and prostheses, preoperative holding area and waiting room; teach deep breathing and coughing exercises, how to turn, move, and splinting of incisions. Postoperative regimen teaching includes: explain PACU routine and emergency equipment; review type and frequency of assessment; discuss pain management; explain usual activity restrictions and precaution when getting up for the first time postoperatively; describe usual dietary alterations; discuss dressings and drains; and provide an explanation and tour of ICU if client is to be transferred there postoperatively. For outpatient surgical clients explain the usual preoperative and postoperative regimens; confirm place and time of surgery, when to arrive, where to register and what to wear; explain the need for a responsible adult to drive or to accompany the client home; discuss medications; communicate by telephone the evening before surgery to confirm time of surgery and arrival time; communicate by telephone within 48 hours postoperatively to evaluate surgical outcomes and identify any problems or complications. 3. The purposes for performing each of these skills include the following: Dr. Abdul-Monim Batiha Page 61 Basics in Nursing Care Moving: to promote venous return, mobilize secretions, stimulate gastrointestinal motility, and facilitating early ambulation. Leg exercises: to promote venous return; prevent thrombophlebitis and thrombus formation. Deep breathing and coughing: to enhance lung expansion and mobilize secretions; prevent atelectasis and pneumonia . Dr. Abdul-Monim Batiha Page 62 Basics in Nursing Care Unit 4 Morning & Evening Care of Surgical patient Describe essential aspects of preparing a client for surgery, including morning care, evening care, nutrition and enema. 1. Physical preparation includes the following: nutrition and fluids, elimination, hygiene, medications, rest, care of valuables and prostheses, special orders, vital signs, safety protocols, and surgical skin preparation. The nurse should identify and record any signs of malnutrition or fluid imbalance. The nurse should also determine whether the client is to be “NPO after midnight” or is permitted food or fluids as recommended by the American Society for Anesthesiology (ASA) revised guidelines. Enemas prior to surgery are no longer routine but may be ordered if bowel surgery is planned. Prior to surgery, straight catheterization or the insertion of an indwelling catheter into the urinary bladder may be ordered. If the client does not have a catheter, the client should empty the bladder prior to receiving preoperative medication. The client may be asked to shower, bathe, and shampoo the evening or morning of surgery (or both). The nails should be trimmed and free of polish, and all cosmetics should be removed. Before going to the operating room the client should remove all hair pins and clips, and put on an operating room gown and surgical cap. Dr. Abdul-Monim Batiha Page 63 Basics in Nursing Care The anesthetist or anesthesiologist may order routinely taken medications be held the day of surgery as well as preoperative medications which are given “on call” or at a scheduled time prior to surgery. To promote rest and sleep, a sedative may be ordered the night before surgery. The nurse should do everything possible to help the client sleep. All prostheses must be removed before surgery. However, hearing aids are often left in place and the operating room personnel are notified. Valuables should be sent home with the client’s family or significant others or be labeled and placed in a locked storage area per agency policy. The nurse checks the surgeon’s orders for any special orders such as insertion of a nasogastric tube, administration of medications, or application of antiemboli stockings . JCAHO has established the Universal Protocol for Preventing Wrong Site, Wrong Procedure, Wrong Person Surgery. This involves three steps: The first step is client verification at the time surgery is scheduled, during admission, and repeated whenever the client is transferred to another caregiver. The second step involves marking of the operative site in an unambiguous manner. The third step is called “time-out.” The surgical team takes a time-out to conduct a final verification of the correct client, procedure, and site. In most agencies skin preparation is carried out during the intraoperative phase. The site is cleansed with an antimicrobial to remove soil and decrease resident microbial count to subpathogenic levels. Dr. Abdul-Monim Batiha Page 64 Basics in Nursing Care The nurse assesses and documents vital signs and reports abnormal findings. o Antiembolic stockings or sequential compression devices (SCD) may be applied. Compare various types of anesthesia. 1. 2. Anesthesia is classified as general, regional, or local. General anesthesia is the loss of all sensation and consciousness. Protective reflexes such as cough and gag reflexes are lost. General anesthetics act by blocking awareness centers in the brain so that amnesia, analgesia, hypnosis, and relaxation occur. They are generally administered by intravenous infusion or by inhalation of gases. 3. Regional anesthesia is the temporary interruption of the transmission of nerve impulses to and from a specific area or region of the body. The client loses sensation in an area of the body but remains conscious. Techniques include the following: topical or surface (applied directly to the skin and mucous membranes, open skin surfaces, wounds, and burns); local or infiltration (injected into a specific area and used for minor surgical procedures); nerve block (injected into and around a nerve or small nerve group that supplies sensation to a small area of the body); intravenous block or Bier block (used most often for procedures involving the arm, wrist, and hand; an occlusion tourniquet is applied to the extremity to prevent infiltration and absorption of the injected intravenous agent beyond the involved extremity); spinal or subarachnoid block (agent is injected into the Dr. Abdul-Monim Batiha Page 65 Basics in Nursing Care subarachnoid space); epidural or peridural (injected into the epidural space); and conscious sedation (minimal depression of the level of consciousness in which the client retains the ability to maintain a patent airway and respond appropriately to commands). Identify essential nursing assessments and interventions during the immediate postanesthetic phase. 1- Essential nursing assessments during the immediate postanesthetic phase include adequacy of airway; oxygen saturation; adequacy of ventilation; cardiovascular status; level of consciousness; presence of protective reflexes; activity; ability to move extremities; skin color; fluid status; condition of operative site; patency of and amount and character of drainage from catheters, tubes, and drains; discomfort; and safety. 2. Interventions include positioning the client on the side, with the face slightly down; elevating the upper arm on a pillow; suctioning as needed until cough and swallowing reflexes return; and helping the client to cough and deep breathe once the oral airway or endotracheal tube is removed. If the client has had spinal anesthesia, keep the client flat for the specified period of time. Dr. Abdul-Monim Batiha Page 66 Basics in Nursing Care Demonstrate ongoing nursing assessments and interventions for the postoperative client. 1- As soon as the client returns to the nursing unit, the nurse conducts an initial assessment. The sequence of assessment varies with the situation. The nurse consults the surgeon’s postoperative orders for the following: food and fluids, IV fluids and position, medications, laboratory tests, intake and output and activity permitted. In addition, the nurse reviews the PACU record for the following: operation performed, presence and location of drains, anesthetic used, postoperative diagnosis, estimated blood loss, and medications administered in the PACU. The nurse assesses level of consciousness, vital signs, skin color and temperature, comfort, fluid balance, dressing and bedclothes, and drains and tubes. 3. Nursing interventions designed to promote client recovery and prevent complications include pain management, appropriate positioning, incentive spirometry, deep breathing and coughing exercises, leg exercises, early ambulation, adequate hydration, diet, promoting urinary and bowel elimination, suction maintenance, and wound care. Dr. Abdul-Monim Batiha Page 67 Basics in Nursing Care Identify potential postoperative complications and describe nursing interventions to prevent them. 1- Potential postoperative problems and preventive nursing interventions include: pneumonia (deep breathe, cough; moving in bed, early ambulation); atelectasis (deep, breathe, cough, moving in bed, early ambulation); pulmonary embolism (turning, ambulation, antiembolic stockings, SCD); hypovolemia (early detection of signs, fluid and or blood replacement); hemorrhage (early detection of signs); hypovolemic shock (maintain blood volume through fluid replacement, prevent hemorrhage, early detection of signs); thrombophlebitis (early ambulation, leg exercises, antiembolic stockings, SCD, adequate fluid intake); thrombus (venous-same as thrombophlebitis; arterial maintain prescribed position, early detection of signs); embolus (turn, ambulate, leg exercises, SCD, careful maintenance of IV catheters); urinary retention (monitor I&O, interventions facilitating voiding, catheterization); urinary tract infection (adequate fluids, early ambulation, straight catheterization, good perineal hygiene); nausea and vomiting ( IV fluids until peristalsis returns, then progression of diet, antiemetic drugs if ordered and analgesics); constipation (adequate fluids, high fiber diet, early ambulation); tympanites (early ambulation, avoid using straws, ice chips and water at room temperature); postoperative ileus (no interventions listed); wound infection (keep wound clean and dry, use surgical asepsis when changing dressings); wound dehiscence and evisceration (adequate nutrition, appropriate incisional support and Dr. Abdul-Monim Batiha Page 68 Basics in Nursing Care avoidance of strain); and postoperative depression (adequate rest, physical activity, opportunity to express anger and other negative feelings). Describe appropriate wound care for a postoperative client. 1. Most clients return from surgery with a sutured wound covered by a dressing. Dressings are inspected regularly to ensure that they clean, dry and intact. Excessive drainage may indicate hemorrhage, infection or an open wound. When dressings are changed, the nurse assesses the wound for appearance, size, drainage, swelling, pain, and status of drains or tubes. Dr. Abdul-Monim Batiha Page 69 Basics in Nursing Care Unit 5 Sterility& sterilization Introduction Nurses are directly involved in providing a biologically safe environment. Microorganisms exist everywhere: in water, in soil, and on body surfaces such as the skin, intestinal tract, and other areas open to outside (e.g., mouth, upper respiratory tract, vagina, and lower urinary tract). An infection is an invasion of body tissue by microorganisms and their proliferation there. Such a microorganism is called an infectious agent. If the microorganism produces no clinical evidence of disease, the infection is called asymptomatic or sub-clinical. Dr. Abdul-Monim Batiha Page 70 Basics in Nursing Care Some sub-clinical infections can cause significant damage, for example, cytomegalovirus (CMV) infection in a pregnant woman can lead to significant disease in the fetal. A detectable alteration in normal tissue function, however is called disease. Microorganisms vary in their virulence (i.e., their ability to produce disease). Microorganisms also vary in the severity of the disease they produce and their degree of communicability. If the infectious agent can be transmitted to an individual by direct or indirect contact, through a vector or airborne infection, the resulting condition is called a communicable disease. Asepsis is the freedom from disease-causing microorganisms. To decrease the possibility of transferring microorganisms from one place to another, asepsis is used. There are two basic types of asepsis: medical and surgical asepsis. 1. Medical asepsis: includes all practices intended to confine a specific microorganism to a specific area, limiting the number, growth, and transmission of microorganisms, in medical asepsis, objects are referred to as clean, which means the absence of almost all microorganisms, or dirty (soiled, contaminated, which means likely to have microorganisms, some of which may be capable of causing infection. 2. Surgical asepsis or sterile technique, refers to those practices that keep an area or object free of all microorganism, it includes practices that destroy Dr. Abdul-Monim Batiha Page 71 Basics in Nursing Care all microorganisms and spores. Surgical asepsis is used for all procedures involving the sterile areas of the body. Sepsis is the state of infection and can take many forms, including septic shock. Types of microorganisms causing infections Four major categories of microorganisms cause infection in humans: 1. Bacteria can live and be transported through air, water, food, soil, body tissues and fluids, and inanimate objects. 2. Viruses consist primarily of nucleic acid and therefore must enter living cells in order to reproduce. Common virus families include the rhinovirus (causes the common cold) hepatitis, herpes, and human immunodeficiency virus. 3. Fungi include yeasts and molds. Candida albicans is a yeast considered to be normal flora in the human vagina. 4. Parasites live on other living organisms. They include protozoa such as the that causes malaria. Types of infection BY AREA a) Local – limited to a specific body part Dr. Abdul-Monim Batiha Page 72 Basics in Nursing Care b) Systemic – microorganisms have spread BY LENGTH OF TIME a) Acute – appears suddenly/lasts short b) Chronic – appears slowly, over long periods of time, may last months/years BY CULTURE a) Bacteremia – a culture of person’s blood reveals microorganisms b) Septicemia – when bacteremia has multiplied and spread in a person’s blood circulation Signs of Localized Infection • Localized swelling • Localized redness • Pain or tenderness with palpation or movement • Palpable heat in the infected area • Loss of function of the body part affected, depending on the site and extent of involvement • Fever • Increased pulse and respiratory rate if the fever high • Malaise and loss of energy Dr. Abdul-Monim Batiha Page 73 Basics in Nursing Care • Anorexia and, in some situations, nausea and vomiting • Enlargement and tenderness of lymph nodes that drain the area of infection Signs of Infection • Laboratory data • Elevated WBC count • Increase in specific WBC types • Elevated ESR • Cultures of urine, blood, sputum, or other drainage Risks for Nosocomial Infections • Diagnostic or therapeutic procedures – Iatrogenic infections • Compromised host • Insufficient hand hygiene Factors Influencing Microorganism’s Capability to Produce Infection • Number of microorganisms present Dr. Abdul-Monim Batiha Page 74 Basics in Nursing Care • Virulence and potency of the microorganisms (pathogenicity) • Ability to enter the body • Susceptibility of the host • Ability to live in the host’s body Anatomic and Physiologic Barriers Defend Against Infection • Intact skin and mucous membranes • Moist mucous membranes and cilia of the nasal passages • Alveolar macrophages • Tears • High acidity of the stomach • Resident flora of the large intestine • Peristalsis • Low pH of the vagina • Urine flow through the urethra Nosocomial infections Dr. Abdul-Monim Batiha Page 75 Basics in Nursing Care Nosocomial infections are classified as infections that are associated with the delivery of health care services in a health care facility(hospital acquired infection). Nosocomial infections can either develop during a client's stay in a facility or manifest after discharge. The incidence of nosocomial infections is significant. Major sites for these infections are the respiratory and urinary tracts, the bloodstream, and wounds. Factors that contribute to nosocomial infection risks are invasive procedures, medical therapies, the existence of a large number of susceptible persons, inappropriate use of antibiotics, and insufficient hand washing after client contact and after contact with body substances. Chain of infection Six links make up the chain of infection: the etiologic agent, or microorganisms; the place where the organism naturally reservoir; a portal of exit from reservoir; a method of transmission; a portal of entry into a host; and susceptibility of the host. 1. Etiologic agent The extent to which any microorganism is capable of producing an infectious process depends on the number of microorganisms present. 2. Reservoir Dr. Abdul-Monim Batiha Page 76 Basics in Nursing Care There are many reservoirs, or sources of microorganisms, common sources are other humans, the client's, plants, animals, or general environment. 3. Portal of exit from reservoir Before an infection can establish itself in a host, the microorganisms must leave the reservoir. 4. Method of transmission there are three mechanisms 1. Direct transmission involves immediate and direct transfer of microorganisms from person to person through touching, biting, kissing, or sexual intercourse. Droplet spread is also a form of direct transmission. 2. Indirect transmission material objects, such as toys, soiled clothes, cooking or eating and surgical instruments, or dressing, water, food, blood, serum, and plasma. Animal or flying. 3. Airborntransmission may involve droplets or dust. 5. Portal of entry Before a person can become infected, microorganisms must enter the body. The skin is a barrier to infectious agents; however, any break in the skin can readily serve as a portal of entry. 6. Susceptible Host Dr. Abdul-Monim Batiha Page 77 Basics in Nursing Care A susceptible host is any person who is at risk for infection. A compromised host is a person at "increased risk" Practicing Homosexual/Bisexual Intravenous Drug Users Multiple Blood Transfusion HIV+ Persons/Immunocompromised Multiple Sexual Partners High-Risk Behaviors Very Young And Very Old Increased Length Of Stay Cancer Patients/Immunosuppressed Persons Under Stress Malnutrition Dr. Abdul-Monim Batiha Page 78 Basics in Nursing Care 1 Etiologic agent (microorgnanisms) 6 2 Susceptible host Reservoir (source) Chain of Infection 5 3 Portal of entry to the susceptible host Portal of exit from reservoir 4 Method of transmission Breaking the Chain of Infection • Etiologic agent – Correctly cleaning, disinfecting or sterilizing articles before use – Educating clients and support persons about appropriate methods to clean, disinfect, and sterilize article Dr. Abdul-Monim Batiha Page 79 Basics in Nursing Care • Reservoir (source) – Changing dressings and bandages when soiled or wet – Appropriate skin and oral hygiene – Disposing of damp, soiled linens appropriately – Disposing of feces and urine in appropriate receptacles – Ensuring that all fluid containers are covered or capped – Emptying suction and drainage bottles at end of each shift or before full or according to agency policy • Portal of exit – Avoiding talking, coughing, or sneezing over open wounds or sterile fields – Covering the mouth and nose when coughing or sneezing • Method of transmission – Proper hand hygiene – Instructing clients and support persons to perform hand hygiene before handling food, eating, after eliminating and after touching infectious material – Wearing gloves when handling secretions and excretions Dr. Abdul-Monim Batiha Page 80 Basics in Nursing Care – Wearing gowns if there is danger of soiling clothing with body substances – Placing discarded soiled materials in moisture-proof refuse bags – Holding used bedpans steadily to prevent spillage – Disposing of urine and feces in appropriate receptacles – Initiating and implementing aseptic precautions for all clients – Wearing masks and eye protection when in close contact with clients who have infections transmitted by droplets from the respiratory tract – Wearing masks and eye protection when sprays of body fluid are possible • Portal of entry – Using sterile technique for invasive procedures, when exposing open wounds or handling dressings – Placing used disposable needles and syringes in punctureresistant containers for disposal – Providing all clients with own personal care items • Susceptible host – Maintaining the integrity of the client’s skin and mucous membranes Dr. Abdul-Monim Batiha Page 81 Basics in Nursing Care – Ensuring that the client receives a balanced diet – Educating the public about the importance of immunizations Category-specific Isolation Precautions • Strict isolation • Contact isolation • Respiratory isolation • Tuberculosis isolation • Enteric precautions • Drainage/secretions precautions • Blood/body fluid precautions Transmission-Based Precautions Category Private Room Contact If Gowns possible; Required If precautions cohort available Required Dr. Abdul-Monim Batiha Gloves if not Masks anticipate Not required contact with soiled items; patient is incontinent; Page 82 Basics in Nursing Care diarrhea, ileostomy, colostomy, wound drainage Droplet If possible; Not precautions cohort or Not required required Required when within maintain 3 feet separation of 3 feet Airborne Required. Not precautions Negative air pressure, required 6–12 air changes Not required N95 respirator required for known or per suspected hour, keep door tuberculosis closed, discharge and measles air or varicella if outdoors or not immune HEPA filter Disease-specific Isolation Precautions Dr. Abdul-Monim Batiha Page 83 Basics in Nursing Care • Outline practices for control of specific diseases – Use of private rooms with special ventilation – Cohorting(grouping) clients infected with the same organism – Gowning to prevent gross soilage of clothes Universal Precautions (UP) • Used with all clients • Decrease the risk of transmitting unidentified pathogens • Obstruct the spread of bloodborne pathogens (hepatitis B and C viruses and HIV) • Used in conjunction with disease-specific or category-specific precautions Body Substance Isolation (BSI) • Employs generic infection control precautions for all clients • Body substances include: – Blood – Urine Dr. Abdul-Monim Batiha Page 84 Basics in Nursing Care – Feces – Wound drainage – Oral secretions – Any other body product or tissue Standard Precautions • Used in the care of all hospitalized persons regardless of their diagnosis or possible infection status • Apply to – Blood – All body fluids, secretions, and excretions except sweat (whether or not blood is present or visible) – Nonintact skin and mucous membranes • Combine the major features of UP and BSI Transmission-based Precautions • Used in addition to standard precautions • For known or suspected infections that are spread in one of three ways: Dr. Abdul-Monim Batiha Page 85 Basics in Nursing Care – Airborne – Droplet – Contact • May be used alone or in combination but always in addition to standard precautions Bloodborne Pathogen Exposure • Report the incident immediately (incident report) • Complete injury report • Seek appropriate evaluation and follow-up. This includes: 1. Identification and documentation of the source individual when feasible and legal 2. Testing of the source for hepatitis B, C and HIV when feasible and consent is given 3. Making results of the test available to the source individual’s health care provider 4. Testing of blood exposed nurse (with consent) for hepatitis B, C, and HIV – please check these to match style used in book – fairly certain it should be caped antibodies Dr. Abdul-Monim Batiha Page 86 Basics in Nursing Care 5. Postexposure prophylaxis if medically indicated 6. Medical and psychologic counseling For Puncture/Laceration • Encourage bleeding • Wash/clean the area with soap and water • Initiate first aid and seek treatment if indicated • Mucous membrane exposure (eyes, nose, mouth): -Flush with saline or water flush for 5 to 10 minutes Postexposure Protocol (PEP) for Hepatitis B • Anti-HBs testing 1 to 2 months after last vaccine dose • HBIG and/or hepatitis B vaccine within 1 to 7 days following exposure for nonimmune workers Postexposure Protocol (PEP) for Hepatitis C There is currently no vaccine against the virus no post exposure prophylaxis. Prevention remains the primary goal. Dr. Abdul-Monim Batiha Page 87 Basics in Nursing Care Human body area reservoirs, common infectious microorganisms, and portal of exit common Body area Respiratory tract infectious microorganisms Parainfluenza virus Mycobacterium tuberculosis Gastrointestinal tract Hepatitis a virus, Salmonella species Portal of exit Nose or mouth through sneezing coughing, breathing, or talking. Mouth: saliva, vomitus, anus: feces, ostomies Urinary tract Escherichia coli Urethral meatus and urinary diversion Reproductive tract Neisseria gonorrhoeae Vagina: vaginal discharge; urinary Herpes simplex virus type2 Blood Hepatitis B virus, HIV Staphylococcus meatus:semen, urine Open wound, needle puncture site, any disruption of intact skin or mucous membrane surface Tissue Staphylococcus Drainage from cut or wound Streptococus Dr. Abdul-Monim Batiha Page 88 Basics in Nursing Care Factors Increasing Susceptibility to Infection 1. Age influence the risk of infection. Newborns and older adults have reduced defenses against infection. 2. Heredity influences the development of infection in that some people have a genetic susceptibility to certain infections. 3. The nature, number, and duration of physical and emotional stressors can influence susceptibility to infection. Stressors elevate blood cortisone. Prolonged elevation of blood cortisone decrease anti-inflammatory responses depletes energy stores, lead to a state of exhaustion, and decrease resistance to infection. For example: a person recovering from a major operation or injury is more likely to develop an infection than healthy person. 4. Resistance to infection depends on adequate nutritional status. 5. Some medical therapies predispose a person to infection. For example, radiation treatments for cancer, some diagnostic procedures may also predispose the client to an infection. 6. Certain medication also increase susceptibility to infection. Anticancer medications may depress bone marrow function, resulting inadequate production of white blood cells, anti-inflammatory and antibiotics medications. Dr. Abdul-Monim Batiha Page 89 Basics in Nursing Care WHO IS AT RISK FOR INFECTION? THE HOSPITAL STAFF/SERVICE PROVIDERS They are exposed to potentially infectious blood and body fluids on a daily basis CLIENTS IN THE HOSPITAL Service providers who do not wash hands in between clients and procedures. NOSOCOMIAL INFECTION: Hospital-acquired infection IATROGENIC INFECTION: Direct result of procedures or therapeutic treatments or diagnostic examinations THE COMMUNITY Unsanitary waste disposal, improper disposal of medical wastes such as contaminated sharps, dressings STOPPING TRANSFER OF INFECTION 1) handwashing – the singlemost effective control measure to control infections 2) asepsis– medical asepsis versus surgical asepsis 3) wearing of gloves 4) proper handling and disposal of sharps 5) proper instrument processing Dr. Abdul-Monim Batiha Page 90 Basics in Nursing Care 6) proper waste disposal Cleaning, Disinfecting, and Sterilizing The first links in the chain of infection, the etiologic agent and the reservoir, are interrupted by the use of antiseptics (agents that inhibit the growth of some microorganisms) and disinfectants (agents that destroy pathogens other than spores) and by sterilization. Cleaning Cleanliness inhibits the growth of microorganisms. When cleaning visibly soiled objects, nurses must always wear gloves to avoid direct contact with infections microorganisms. Most objects used in the care of clients, whether forceps or draw sheets, can be cleaned by rinsing them in cold water to remove any organic material, washing them with hot soapy water, then rinsing them again to remove the soap. Disinfectants are antimicrobial agents that are applied to non-living objects to destroy microorganisms, the process of which is known as disinfection. Sanitizers are high level disinfectants that kill over 99.9% of a target microorganism in applicable situations. Very few disinfectants and sanitizers can sterilize. Antiseptics are chemical agents used on living objects to reduce the number of microorganisms on skin and mucous membranes without causing tissue damage. They can prevent the growth and development of some microorganisms. Dr. Abdul-Monim Batiha Page 91 Basics in Nursing Care Used for: surgical scrub, skin prep of clients, handwashing in high risk cases of newborn, immunocompromised clients Antiseptics: Iodophors (betadine), Iodine(povidine), Sodium hypochlorite, Hydrogen peroxide 3%, alcohol, ethyl or isopropyl alcohol, chlorhexedine Antiseptics do not have the same killing power of disinfectants Disinfectants: 1) Glutaraldehyde (Cidex) – irritating, used for sterilization of medical/surgical instruments; Formaldehyde – acqueous solution used for embalming(preserving) 2) Halogens (Chlorine, Sodium hypo) – strong oxidizing agents used for decontamination, high-level disinfection Dr. Abdul-Monim Batiha Page 92 Basics in Nursing Care Prevention Contamination of Antiseptics: Use sterile solution as diluent. Pour out antiseptics into sterile containers. Open caps and put on a surface with sterile side up. Never leave cotton balls or gauze soaked in an antiseptic solution. Never dip cotton or gauze into antiseptics. Instead, pour the antiseptic on the cotton or gauze. Clean the area on which solutions are prepared. Prevention Contamination of Antiseptics: Dr. Abdul-Monim Batiha Page 93 Basics in Nursing Care Properties of Common Antiseptics • IODOPHORS (Betadine) - Contain iodine in noncomplex form; non-irritating, nontoxic - Effective against a range of microorganisms - USAGE: For surgical scrub and client prep; effective 1-2 minutes after application; use full strength - ADVANTAGES: Less irritating than iodine - DISADVANTAGES: Effectiveness is reduced by presence of blood and other organic materials • IODINE; TINCTURE OF IODINE - Effective against a range of microorganisms - USAGE: For skin decontamination, wound packing and irrigation iodine must be allowed to dry and then removed from the skin using alcohol - ADVANTAGES: Fast acting - DISADVANTAGES: Too irritating for surgical scrub or for mucous membranes. Effectiveness is reduced by presence of blood and other organic materials • ALCOHOL (60%-90%) Dr. Abdul-Monim Batiha Page 94 Basics in Nursing Care - Effective against a range of microorganisms - USAGE: skin prep before injection, Cannot be used when skin is visibly dirty; wash the area first; must dry completely to be effective - ADVANTAGES: Kills microorganisms rapidly. Most effective in reducing microorganisms. - DISADVANTAGES: Has drying effect on skin. Cannot be used on mucous membranes. Effectiveness is reduced by presence of blood and other organic materials -Hydrogen peroxide 3% (H2O2) kill decomposes necrotic tissue and used for wound irrigation, cleaning of pus and necrotic tissue. PROPER HANDLING AND DISPOSAL OF SHARPS Avoid recapping the needle Do not bend, cut or break needles Dispose of needles and sharps in a puncture-resistant container Wear utility gloves when disposing of sharps container PROPER INSTRUMENT PROCESSING 1. DECONTAMINATION – makes items easier to clean by softening blood, body fluids, tissues; makes items safer to clean Dr. Abdul-Monim Batiha Page 95 Basics in Nursing Care Chlorine: - Disinfectant; powerful killer of microorganisms - Deodorizes; not poisonous in its concentration - Leaves no poisonous residue - Colorless, easy to handle, economical to use - Acceptable household/hospital disinfectant is 0.5% chlorine solution 2. CLEANING: Refers to scrubbing with a brush, detergent and water Removes organic material, dirt and foreign matter that can interfere with sterilization. Reduces the number of microorganisms Removes contaminants in joints, grooves and teeth of items 3. STERILIZATION: Ensures freedom from all microorganisms For surgical instruments, needles, that come in contact with bloodstream or tissues 3 methods a) Steam sterilization - “autoclaving”, or moist heat under pressure Dr. Abdul-Monim Batiha Page 96 Basics in Nursing Care b) Dry heat – high heat for prolonged period of time c) Chemical – for heat-sensitive items (Cidex) HIGH-LEVEL DISINFECTION Eliminates microorganisms but does not kill endospores which gas gangrene, tetanus Suitable for items that come in contact with broken skin or intact mucous membrane 3 methods: a) Boiling – longer than 20 minutes b) Chemical – for heat-sensitive items (Cidex, Chlorine) c) Steam – best for gloves 5- USED OR STORED If items are not properly stored, all efforts will have been wasted, items may be contaminated Always store instruments dry Do not store them soaked in antiseptic or disinfectant solutions 6. PROPER WASTE DISPOSAL General Housekeeping Guidelines: Dr. Abdul-Monim Batiha Page 97 Basics in Nursing Care Wear thick gloves when cleaning Reduce spread of dust and microorganisms by damp(wet) mop or cloth for walls, floors and surfaces Scrubbing is the most effective way to remove dirt and microorganisms Wash surfaces from top to bottom so that debris falls in the floor is cleaned up last Change cleaning solutions whenever they appear dirty Cleaning up spills(drops): Clean up immediately any potentially infectious fluids Always wear gloves when cleaning spills If spill is small, clean with cloth that’s saturated with disinfectant If spill is large, flood with a disinfectant, mop it and then scrub the area with a disinfectant cleaning solution Change cleaning solutions whenever they appear dirty Do not put a cloth over a spill for cleaning up later Three kinds of waste in the community: 1. General waste – poses no risk of injury or infection (bottles, boxes, food-related trash, plastic containers..) Dr. Abdul-Monim Batiha Page 98 Basics in Nursing Care 2. Medical waste – generated in the diagnosis, tx, or immunization 3. Hazardous chemical waste – those that are potentially toxic or poisonous, and radioactive compounds Three kinds of waste in the hospital: 1. Biodegradable – any organic wastes that are perishable(subject to decay) and are rotten(fragile from use) 2. Non-biodegradable – those that are not perishable like plastics, bottles, packaging materials 3. Infectious – those that have come in contact with blood and body fluids (sponges, needles, sharps etc.) Sterilizing Sterilization is a process that destroys all microorganisms, including spores and viruses. Four commonly used methods of sterilization are: 1. Moist heat: for sterilizing, moist heat (steam) can be employed in two ways: as steam under pressure attains temperatures higher than the boiling point. Autoclaves supply steam under pressure of 121 to 123C. Free steam 100C is used to sterilize objects that would be destroyed at the higher temperature and pressure of autoclave. Contamination can occur at latent time, so packaging should be checked for integrity. Because the object is considered sterile only for specified period, always check the expired date. Dr. Abdul-Monim Batiha Page 99 Basics in Nursing Care 2. Gas: Ethylene oxide gas destroys microorganisms by interfering with their metabolic processes. Its advantages are good penetration and effectiveness for heat-sensitive items. Its major disadvantage is its toxicity to human. 3. Boiling water: this is the most practical and inexpensive method for sterilizing in the home. The water temperature rises no higher than 100C. Boiling a minimum 0f 15 minutes is advised for disinfection of articles in the home. Boiling water is not an effective sterilization measure as some viruses and spores can survive boiling water. Objects that have been boiled in water for 15 to 20 minutes at 121°C (249.8°F) are considered clean but not sterilized However, boiling water is still the best and most common sterilization measure used in the home. For example, boiling baby bottles and nipples makes them safe for use. 4. Radiation: both ionizing and nonionizing radiation can be used for disinfection and sterilization. Ultraviolet light, a type of non-ionizing radiation, can be used for disinfection. Ionizing radiation is used effectively in industry to sterilize foods, drugs, and other items that are sensitive to heat. Its main advantage is that it is effective for items difficult to sterilize, its chief disadvantage is that the equipment is very expensive. Dr. Abdul-Monim Batiha Page 100 Basics in Nursing Care Sterile Technique: An object is sterile only when it is free of all microorganisms. The basic principles of surgical asepsis: 1. All objects used in a sterile field must be sterile. 2. Sterile objects become unsterile when touched by un-sterile objects. 3. Sterile items that are out of vision or below the waist level of the nurse are considered unsterile. 4. Sterile objects can become unsterile by prolonged exposure to airborne microorganisms. 5. Fluids flow in the direction of gravity. 6. Moisture that passes through a sterile object draws microorganisms from un-sterile surfaces above or below to the sterile surface by capillary action. 7. The edges of a sterile field are considered un-sterile. 8. The skin cannot be sterilized and is un-sterile. 9. Carefulness, alertness, and honesty are essential qualities in maintaining surgical asepsis. Dr. Abdul-Monim Batiha Page 101