Ivermectin
advertisement
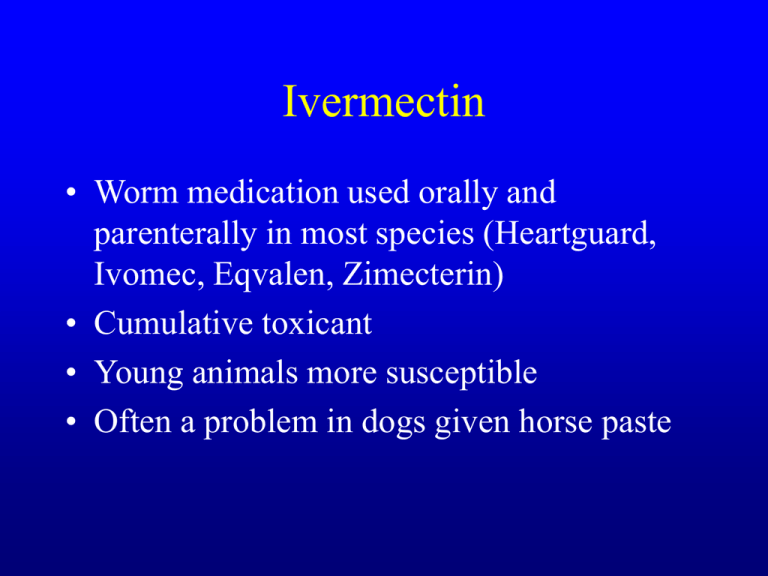
Ivermectin • Worm medication used orally and parenterally in most species (Heartguard, Ivomec, Eqvalen, Zimecterin) • Cumulative toxicant • Young animals more susceptible • Often a problem in dogs given horse paste Ivermectin • Dogs-6ug/kg =heartworm preventive dose; • 2.5 mg/kg PO =mydriasis, 5mg/kg PO= muscle tremors, 40 mg/kg PO= death • Collies, Aust. Shepherd, Shelties, Border Collies0.1 -0.2 mg/kg PO or SC causes toxicity and death • Cats-0.5mg/kg=mydriasis and tremors • Equine-2mg/kg=ataxia and blindness • Cattle and Sheep-4mg/kg=ataxia/death Ivermectin • Mechanism of action is to increase GABA release, affinity of GABA receptor and direct GABA agonist • Onset time is hours to 1 day, affects CNS • Clinical signs-hypersalivation (dogs), tremors, bradycardia, convulsions, coma, mydriasis, blindness, ataxia • Can see anaphylactic reactions in dogs • No visible lesions Ivermectin Diagnosis • History of administration • Brain ivermectin concentration >100ppb Treatment • Short acting barbiturate for convulsions (no benzos) • IV physostigmine (0.04mg/kg) BID in comatose animals • Flumanezil and moxidectin-expt. Benzo antagonists • Epinephrine, fluids for anaphylaxis Household Cleaners • Product warning label indicates level of toxicity – – – – No label = LD50 > 5 g/kg Caution = 0.5 – 5 g/kg Warning = 50 – 500 mg/kg Danger: Poison = <50 mg/kg Soaps, Shampoos, Detergents • Most have low toxicity • Usually cause only vomiting and diarrhea • Cationic surfactants are found in contact lens solutions, fabric softeners, swimming pool algicides; can cause neuromuscular and ganglionic blockade as well as GI ulcerations, acidosis and shock • Anionic surfactants are in many cleaning products like shampoos have the potential to cause hemolysis Disinfectant Cleaners • Products like Lysol contain phenolic compounds mixed with detergents • Pine oil based compounds like Pine Sol • These products are especially toxic to cats due to metabolism by glucuronidation; can cause liver injury, jaundice, and renal damage in conjunction with GI problems • Phenolics also found in creosote and tar paper; watch out for pigs Alkaline Compounds • Ammonia, Oven Cleaner, Most Drain Openers • All have pH of >12 which can cause burns (ulcerations) • Ulcers can be very severe, especially with granular drain openers • Ingestions causes GI ulcerations, vomiting, salivation, dysphagia (esophageal stricture), dyspnea • Bleach and scouring powders with bleach usually not high enough pH to cause ulceration; can be a problem if mixed with ammonia = chloramine gas Acidic Compounds • Toilet bowl cleaners, concrete cleaner, Lime-A-Way, some drain openers • Can cause severe burns, but usually not as deep as alkali • Signs and treatment similar to alkaline products Treating Household Cleaner Ingestions • If a potentially toxic amount of a noncorrosive compound ingested, emesis should be induced; no activated charcoal unless systemic effects are expected • For corrosive compounds 1) dilute with milk or water, 2) determine exactly how much of what material was ingested Treating Toxic Corrosive Ingestions • If there is pain, dysphagia, excessive drooling, or ulceration and the exposure was potentially toxic: – Establish airway and get esophagoscopy – If esophagus can’t be examined quickly, start corticosteroids – If examination indicates burns, give corticosteroids – Symptomatic and supportive care Drano Ingestion – Initial Visit Drano Ingestion – Final Visit Petroleum Products • Gasoline, mineral spirits, kerosene, lighter fluid, nail polish remover, solvents, motor oil, furniture polish • Biggest worry is aspiration causing hydrocarbon pneumonia • Pneumonia risk related to viscosity; less viscous = more toxic Systemic Toxicity of Hydrocarbons • Most hydrocarbons are CNS depressants • Some volatile hydrocarbons sensitize the heart to catecholamines and can cause sudden death due to cardiac arrest • Many hydrocarbons cause dermal irritation and hair loss Signs of Hydrocarbon Toxicity • Depression, lethargy, ataxia, seizures, coma • Dyspnea, coughing, wheezing, X-ray changes in lungs with pneumonia – Spontaneous vomiting and aspiration often occurs with more volatile compounds Treating Hydrocarbon Ingestions • Wash for dermal exposures • Do not try to increase viscosity by adding heavier compound • Do not induce emesis unless a large, life threatening ingestion (>1 ml/kg) • Monitor for pneumonia; treat with antibiotics if present Oak (Acorn) Poisoning • Red Oak are most toxic due to high tannins, Live Oak is questionable • problems are seasonal, usually in fall after a storm or during summer droughts • primarily affects cattle; calves are more susceptible • Toxic priniciple is thought to tannins or their metabolites • Animals must consume large amounts of acorns or buds to be toxic Oak poisoning • Cases have relatively low morbidity with moderate mortality (35-80%) • Animals usually ingested acorns for 1 week prior to signs • Symptoms are primarily renal and GI-anorexia, depression, weakness and possible nasal discharge; progresses to rumen atony, black tarry diarrhea, ventral edema, dehydration. • terminal animals are often recumbent near water Cyanogenetic Plants • Wild and choke cherry, Sudan and Johnson grass, Flax, Sugar beet tops, Arrow grass • contain glycosides with cyanide groups Thiaminases • Horsetails and Bracken Ferns • Thiaminases destroy thiamine causing neurological problems; causes aplastic anemia in ruminants • Primarily affects horses and ruminants • Usually occurs if other forage is inadequate Bracken Fern Calcium Oxalate plants • Members of Araceae family contain calcium oxalates; Dieffenbachia (Dumb Cane), Philodendron, Elephant ear, Calla lily, Arum lily, Caladium • All parts of plant are toxic; stalk more toxic than leaves • Usually occurs in cats, dogs, birds, and lizards • Rarely life-threatening Calcium Oxalate plants • Preformed calcium oxalate crystals embed in all parts of GI tract; also contain proteolytic enzymes that cause histamine release • Onset time is immediate; primarily affects GI system • Clinical signs include head shaking, salivation, dyspnea, vomiting, diarrhea, loss of voice Calcium Oxalate plants • Diagnosis is by history of exposure and compatible clinical signs • Treatment • • • • Rinse mouth with water Anithistamines for dyspnea Demulcents (Kao-pectate; no Pepto in cats) Fluids for severe vomiting and diarrhea Precatory Bean; Rosary Pea • Grows in Carribean • Commonly sold as rosary “beads” • Extremely toxic, 1 pea can kill a child or dog • Severe enteritis leads to shock Castor Bean • Common plant in S. Florida • Mole plant • Seeds are extremely toxic due to ricin Oleander • Contains cardiac glycosides (much like digitalis) • Highly toxic Cassia • Coffeeweed, sicklepod • Causes muscle degeneration Crotalaria • Rattlebox • Causes liver injury Cycas and Zamia • Sago Palms, Coontie Plants • Seeds are especially toxic • Causes liver injury Sesbania • Seeds are most toxic part • Produce severe hemorrhagic or necrotic enteritis Cestrum • Day and night blooming jessamine • Contains Vitamin D • Kidney damage Lantana • Causes photosensitization secondary to liver injury